An ongoing dialogue on HIV/AIDS, infectious diseases,
November 7th, 2025
Favorite ID Fellow Consults: Johns Hopkins Edition
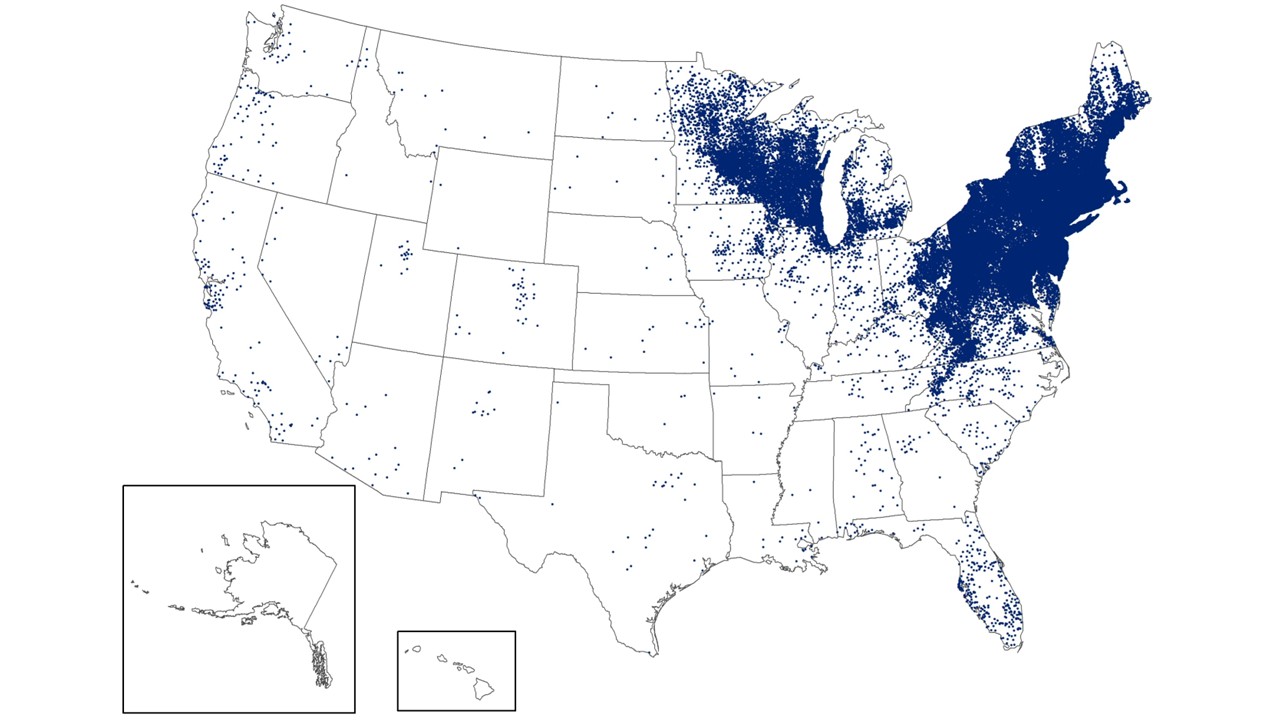
Lyme disease cases, 2023 (CDC). Each dot represents a new reported case.
Just back from a visit to the Infectious Diseases Division at Johns Hopkins, thanks to the kind invitation of current ID chief Dr. Amita Gupta and her predecessor, Dr. David Thomas.
On a personal note, this visit was only a few decades late. When I applied to medical school, Hopkins never invited me to interview — an awkward omission since my father’s family is from Baltimore, and my aunt had generously offered to host me when I was “interviewing at Hopkins.”
Oops.
That said, all is forgiven. They could not have been more welcoming this time around. In a busy day spent mostly chatting with ID faculty, a highlight was sitting down to lunch with their current ID fellows — and not just because of that delicious lunch.
I asked them a simple question: What are your favorite ID consults? I already know the greatest hits from our Harvard ID fellows; would responses from another academic powerhouse be similar?
Here’s what they said:
“Patient coughed up a worm.”
A perennial crowd-pleaser, sure to bring gasps of delight when the consult question pops up on the beeper. (We ID doctors are weird.) In hospitalized patients, this is most likely Ascaris lumbricoides — typically when adult worms migrate from the gastrointestinal tract into the respiratory tract, sometimes triggered by anesthesia in patients with a heavy worm burden. Treatment is a single dose of albendazole or mebendazole. And no, they do not require respiratory (or other) precautions.
Fever of unknown origin in a previously healthy person.
Don’t confuse this with fever of “unknown” origin in a patient who has been in the ICU after surgical complications that occurred shortly after Memorial Day, with today being hospital day #160. That’s actually a Fever of Too Many Origins (FOTMO), as brilliantly described by Dr. Harold Horowitz in his classic NEJM piece. (Required reading for all ID docs.) By contrast, true FUO in a previously well patient remains one of the most challenging and intellectually satisfying puzzles in medicine.
Tick-bite infections.
Always gratifying — especially when it’s anaplasmosis and the patient shows that magical overnight response to doxycycline. And in case anyone in New England feels that we have the privilege to be uniquely obsessed with these critters, a glance at the Lyme map shows the mid-Atlantic states are similarly stricken. It’s no wonder long-time Hopkins faculty member Dr. Paul Auwaerter is a lead researcher in the phase 3 Lyme vaccine clinical trial — we eagerly await results!
Exposure history that sounds like a parody of an exposure history.
An example they offered: A patient from rural Maryland lives on a farm, processes their farm’s poultry on-site in a mobile unit, and works long days in fields and buildings teeming with insects and rodents. Oh, and last week they cleaned out a chicken coop with a leaf blower without wearing respiratory protection. Now, they’re admitted with fever, cough, and pneumonia. You know, your typical ID board certification question, only real life. (For non-medical readers out there, this could be anything — viral, bacterial, fungal, allergic.)
A case right in your ID attending’s wheelhouse.
Imagine the fellow is on service with a world-famous expert in syphilis. A consult comes in for a patient with eye pain, redness, photophobia, and blurred vision; the ophthalmologist has already diagnosed pan-uveitis. The history reveals many high-risk sexual exposures and prior bacterial STIs. You can be sure the attending will be thrilled to deliver a state-of-the-art lecture on syphilitic ocular disease, ready for publication as a review article, references already formatted.
The mystery culture nobody recognizes.
The microbiology lab reports a result that sounds vaguely extraterrestrial, and the primary team panics. Enter ID: “Oh — that’s really just Old Familiar Bug X, renamed Y thanks to the NGS/MALDI-TOF revolution.” Diagnosis: MALDI-TOF-itis*! Treatment: reassurance and something sensible. (*Am I the first person to coin that term? If so, I claim patent rights.)
Fever in a returning traveler.
One of the great ID pleasures: The vicarious thrill of taking a highly detailed travel history. Where did they go? When? What did they eat? Swim in? Where did they sleep? (And with whom, ahem.) Sure, malaria must always be ruled out, but we quietly delight in the diagnostic breadth: dengue, chikungunya, typhoid, rickettsioses, schistosomiasis — and the occasional diagnosis you only see every five years but remember forever.
These are all great examples, and I enjoyed our conversation enormously. And full credit to them for giving me the idea for my latest blog post (this), and for that, I’m grateful enough to send along a free subscription.
And — circling back to my opening question — were their picks similar to those from the Harvard ID fellows? Absolutely. In every program, what excites trainees most is the same rich blend of detective work, unexpected biology, and quirky human detail that draws us to infectious diseases in the first place.
Overall, it was a terrific visit — the kind that reinvigorates your enthusiasm for our field and for the bright future embodied by the next generation, even against today’s storm clouds (about which the less said, the better).
Now, about that medical school interview …
(If you’d like a more informal take on a recent ID headline — the latest listeria outbreak — I’ve written about it on my Substack.)


Thanks to you and the fellows for this great list, Paul.
I have always been a big fan of a good FUO. Such a good puzzle!
But I would also love the syphilis lecture (“the great pretender”) from the esteemed attending.
Well done as usual, Paul! Thanks so much for the visit. Next time you apply to medical school I personally guarantee you an interview- by zoom.
Loved these topics, Paul! In my lecture (yesterday!) about pneumonia, the topic of psittacosis came up when discussing atypical causes. I told my nursing students that psittacosis is one reason why ID consults always include a question about pets in the home, including birds! I also got to talk about the Philadelphia connection to Legionnaires’ Disease (I am, ahem, old enough to remember the now-infamous American Legion convention in Philly in 1976).
Why do you suppose Hopkins declined to interview you? It’s hard for me to believe you didn’t have excellent grades and MCAT scores and a beautifully written essay.
(Since this question may seem impertinent, I take no offense if you decline to answer).
To be fair to them, I had an unconventional application (English major), and one major blemish on my pre-med grades. It was physics, which I took the year I was editor of one of the Lampoon editions. Let’s just say it wasn’t my finest moment academically!
– Paul
Paul, I resemble that remark! I received no interview invitation from JHU SOM, either! Actually, I was a worse candidate – rejected by 9 schools, waitlisted by one (Vanderbilt, my undergrad alma mater).
I also was unconventional, having transferred from Caltech to Vanderbilt halfway through college. Happily, Vanderbilt accepted me from the waitlist with weeks to go before classes started.
I often tell trainees to prepare for a gauntlet – but not to get discouraged if they have the passion.
Nice to know that I presented with one of the ID favorites – FUO. I wish I had known so that I could share in the merriment. At one point I had three physicians arguing over the etiology – GP, surgeon, and GI. Cancer? Parasite? IBD? The winner? IBD – Crohn’s Disease with the diagnoses made only after surgery. The GP won the argument.