An ongoing dialogue on HIV/AIDS, infectious diseases,
May 22nd, 2016
Drug Prior Authorizations Are a Very Blunt Tool for Cost Containment — And They’re Annoying
 Insurance prior authorizations, or prior approvals (PAs) — those dreaded forms clinicians have to fill out, usually triggered by prescribing a non-formulary drug — are much on my mind these days. And most of it has to do with three letters, specifically “TAF.”
Insurance prior authorizations, or prior approvals (PAs) — those dreaded forms clinicians have to fill out, usually triggered by prescribing a non-formulary drug — are much on my mind these days. And most of it has to do with three letters, specifically “TAF.”
As readers of this site probably know, there are now three tenofovir alafenamide (TAF)-based coformulations approved for HIV treatment, all theoretically available for prescription alongside the older tenofovir disoproxil fumarate (TDF)-forms. In comparative clinical trials, TAF has consistently had a more favorable effect on bone and renal health than TDF — a benefit of considerable importance to older patients with HIV.
Why do I bring up these older patients? If you’ve been doing HIV clinical care for a while, your patient population is probably a lot like mine:
- Of a certain vintage — note I didn’t say “old”, though this apt definition isn’t far off the mark. In one of my patient sessions last week, the average age was 57 (range 45 – 71); for the record, the oldest patient with HIV seen in our practice last week was 88.
- On HIV treatment for a long time — often more than a decade.
- Virologically suppressed — they are great at taking their antivirals.
These characteristics mean that AIDS-related complications are very unlikely to happen. If I found out that one of my stable HIV patients were hospitalized after being struck by a meteorite or falling satellite, this would surprise me only a little more than if one were admitted with Pneumocystis pneumonia. If we consider the health concerns of these individuals, non-AIDS diseases are far more likely to occur than those related to HIV.
And while we clinicians can’t control the random showering of space debris, we can try to minimize drug toxicity — which brings me back to the TAF-based HIV treatments, and whether we should be using them, and in whom.
I’d argue that these older HIV patients are ideal candidates for TAF (as opposed to TDF) -based drugs, and I’ve found myself wanting to switch them from TDF to TAF multiple times each week. Aging intrinsically leads to declines in renal function and bone density, and increases the likelihood that there will be comorbid conditions further impacting the kidneys and bones (hypertension, diabetes, menopause for women). Furthermore, a patient’s lengthy HIV treatment often means that they have been on TDF for a long time — probably the most important risk factor for clinically important TDF-induced toxicity.
This clinical reasoning, however, is currently lost on most of the payers, who have set up their favorite tool — the “PA” (cue scary music here) — to discourage use of these new drugs.
As far as I can tell, it’s not that they have critically reviewed the data comparing TAF with TDF, and concluded that they disagree, or find it scientifically inaccurate. It’s simply that the TAF treatments are new, and new means you have to jump through hoops to get it.
Or, even worse, you can’t get it at all. Here’s an email I received from a pharmacist trying to help me on one of these cases, this for a 70-year-old man with osteopenia currently on TDF/FTC in whom I thought TAF/FTC would be a safer choice:
The medication is not covered and is excluded from coverage because it is a new drug to market. [Insert payer or pharmacy management company here] said that a review for coverage is not possible and that an appeal would be denied outright. They also said that a letter of medical necessity would not help to obtain coverage, either.
Thank you! Have a nice day!
Dan
Glad he can be so cheerful!
Look, I get it — drug costs are high, and PAs theoretically are a way of avoiding inappropriate use of new, more costly agents when older drugs would do the job just as well.
And though all three of the TAF formulations are cost-neutral to the older TDF treatments based on Average Wholesale Price, one has to assume there have been negotiations on price between the payers and manufacturers with TDF, deals that haven’t yet been made with TAF. (Or made public to us or our patients — “transparent” is never the word used to describe these deals.)
In addition, payers may well be looking forward to generic TDF, which is scheduled to become available next year and presumably would cost even less. It presumably will be easier to switch patients to generic TDF from branded TDF than from TAF, as a TAF to TDF switch could be viewed as switching to a potentially more toxic drug. Who would do that?
But are these mandatory PAs really the right way to decide whether a treatment is indicated — based solely on whether it’s new, and whether the clinician and his/her team have the endurance to fill them all out? Colleagues of mine delve deeper into the TAF vs TDF cost issues here, a welcome review of the relative values of these two drugs.
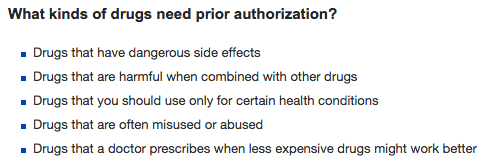
Meanwhile, over on an insurance company’s web page, they list the reasons behind PAs as follows:
As far as I can tell, bullet #5 is by far the most common reason for a PA — especially if the drug is new.


It is possible to implement information management tools which encourage the standard of care rather than resorting to prior authorization notices. If the standard of care needs to be updated for newer drugs on the market, there should be a process for this that does not involve prior authorization notices. I suspect the ID community should take the lead in assuring the standard of care is up to date.
Don’t even get me started, Paul. PAs, which I also call hoop-jumping, are time-consuming and usually pointless. And almost always required because a new drug was prescribed or — my favorite — the PBM (pharmacy benefits manager) has negotiated a better deal with one manufacturer.
When a bunch of PBMs switched from Lantus insulin to Levemir insulin as their “preferred” long-acting insulin, I had lots of PAs to deal with. It was very frustrating to have an insurance company decide that my stable patients with good glycemic control should switch to another insulin. It was also frustrating to be told by the PBM that Lantus and Levemir act the same and can be substituted in a 1-for-1 manner. When I tried to explain that Levemir’s pharmacokinetics are different from Lantus’s, especially at lower doses, I didn’t get very far. Needless to say, the insurance companies made Lantus so prohibitively expensive for my patients (even with a PA), that I and others in my group had to switch patients to Levemir and monitor them closely until we figured out what dosage worked.
Remind me again why we put up with this. Yes, I know. Our patients cannot afford the non-formulary drugs.
The entire US drug pricing and payer reimbursement system is broken. Unfortunately, the precious health of patients and time of their providers is being held hostage by the current disastrous vicious cycle of exorbitant drug pricing and cost-containment measures such as prior approval (PA) and specialty tiering. In the recent past, drug manufacturers have had it all their own way, charging what the market will bear. Now, as a result of the Affordable Care Act, the pendulum has swung toward the payers that now have greater power. While I applaud checks on drug pricing, unfettered and often times irrational PA and specialty tiering practices are not the answer.
What is the solution to this US nightmare? It is obviously Congressional legislation that is also being held hostage to bipartisan nonsense and campaign contributions. We have seen some election year Congressional action against the most egregious offenders. Will any changes really occur once the election is over? The election circus we are witnessing while Rome burns is a symptom of US governmental dysfunction as is the outrage of the people. Hopefully, our collective answer will not be a “No Nothing” president.
What we need are solutions like reasonable price controls based on the actual cost of bringing drugs to market and transparency in what drug companies charge payers as well as the ability of government payers to negotiate all drug prices. Our current system needs to be completely overhauled. The dirty BIG secret is that this mess is causing unnecessary patient morbidity and mortality and provider burn-out.
I agree with Loretta’s sentiments. Yes PAs are bad, but what’s worse are these formulary changes: insulin types, any class with 3+ drugs on the market, or an inhaler that I suddenly have to request a prescription for and learn how to use a brand new device.
But yes sometimes it feels like PAs are setup default for new drugs and is frustrating. They have people to analyze the data (usually), but will often delay for cheaper alternatives as you mentioned generic TDF. It happened for HCV treatment and will likely continue.
There is only one solution for the annoyances you have described such as PA’s and all the other bullshit we have to go through. I am a general internist. None of these problems is going to get better. (and isn’t it ironic that Medicare doesn’t require PA’s for imaging?)
The only solution I have found is insulation against the bullshit, provided by 40 mg fluoxetine daily. It allows me, a non-depressed person, to focus on the joys of medicine and be less aggravated by the indignities.