An ongoing dialogue on HIV/AIDS, infectious diseases,
October 2nd, 2016
“Brink of HIV Cure” ID Link-o-Rama
 There, that title got your attention, didn’t it?
There, that title got your attention, didn’t it?
Anyway, this HIV cure news thing and a few other ID/HIV topics to contemplate while buying your pumpkin, celebrating the New Year in October, or shaking your head that all the stores seem to be putting out their Christmas stuff already. I mean, come on — it’s not even Halloween!
- Are British scientists really on the “brink” of an HIV cure? No. Very glad they are making “remarkable progress”, but sounds like overly ambitious headline-writing to me. Reminiscent of this story from a few years ago.
- Nice summary over the latest controversies involving the flu vaccine, in case your patients are asking. Repeated vaccines leading to reduced response, status of the live attenuated nasal vaccine (not dead yet — pun intended!), effect of statins (but not NSAIDs — remember that?) — lots of good stuff here. And yes, we should still be encouraging the annual shot.
- Another complication of severe influenza infection — invasive aspergillosis. Everyone knows about bacterial superinfections, now here’s another one to watch out for this flu season.
- Serious illness appears to be rare among children who acquire Zika. Refreshing to have some good news on this particular subject. Note that most of the children in this series were older (median age 14), hence it’s not known whether acquisition of Zika in a newborn would have different clinical manifestations (in particular, long-term neurologic complications).
- On the topic of Zika, CDC now recommends that men wait at least 6 months from last possible exposure (if even if asymptomatic) before attempting conception with their partner. This 6 month wait was previously recommended only for men who had symptoms. Is there a role for antibody testing after possible exposure? Unknown, but I bet good money that people will do it (understandably).
- Tenofovir alafenamide works just as well as tenofovir disoproxil fumarate for hepatitis B. As we’ve seen in other comparative studies with TDF, there was a more favorable effect on bone and renal markers. Since treatment is going to be lifelong, the rationale behind using TAF over TDF in hepatitis B is going to be just as strong as it is with HIV. (And you can use TAF in co-infected patients, despite the package inserts for TAF/FTC, ECF-TAF, and RF-TAF.)
- From 2010-2013, approximately 1 in 4 people newly diagnosed with hepatitis C already had laboratory evidence of advanced fibrosis. Suspect the situation is much better now — there’s been a huge push for screening — but these data indicate a substantial burden of HCV-related disease regardless.
- Prospective study shows that patients with HCV-related cirrhosis have significantly better outcomes after HCV cure. Important outcomes, too — lower rates of hepatic decompensation, hepatocellular carcinoma, and death. People with HCV-related cirrhosis are analogous to HIV with CD4 < 200, or AIDS complications — that is, those likely to benefit the most, and soonest, from treatment.
- A single dose of azithromycin significantly reduced the risk of post-cesarean section infection when added to standard cephalosporin prophylaxis. Putative explanation is azithromycin’s activity against Ureaplasma urealyticum. Data from this study seem very convincing, and likely to change standard of care soon.
- One mother explains why she’s no longer anti-vaccine after her whole family — including her three children — developed severe rotavirus infection. Very brave to go public with something like this, and valuable, too, as turnarounds from previous anti-vaccination individuals seem particularly persuasive. For the record, my pediatrician wife says her practice saw a decline in hospitalizations only months after the rotavirus vaccine was approved.
- The HPV vaccine is already reducing the incidence of incidence of cervical intraepithelial neoplasia. It will be fascinating to see how guidelines for cervical cancer screening are modified (with presumably reduced need for screening) as the cohort of vaccinated females ages.
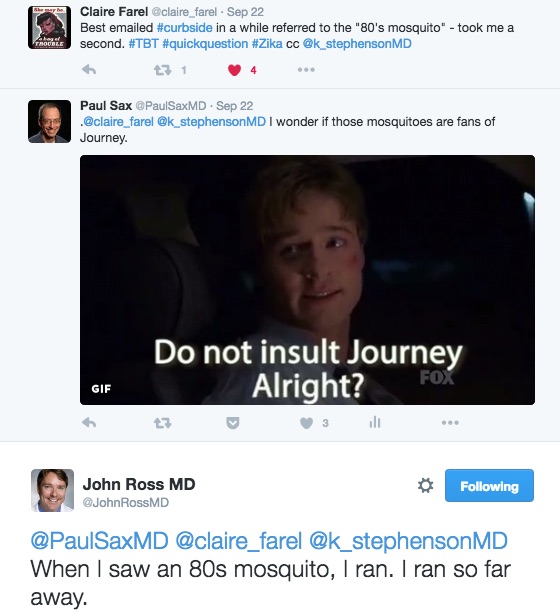
Meanwhile, allow me to finish with this very funny curbside (at least funny to us).
Yes, I know — ID geek jokes. 80s mosquito, ha.
Sorry.


I laughed at the 80’s mosquito jokes, and I’m not an ID geek. An ID groupie, maybe. 😉
Reading the Statnews article was somewhat depressing. I am really hoping we can get beyond the argument that “Some protection is better than none” when it comes to the flu vaccine. True that, but not terribly convincing to our patients. Of course, the only way we will be able to get beyond that is to have a vaccine that is highly effective from year-to-year. I can hope, can’t I?
Important news about the effects of HCV Tx on patients with compensated cirrhosis. I tell my students that as HCV is becoming less of a factor in the US liver transplant rate, NAFLD/NASH is stepping up to the plate and becoming more of a factor. (See, I got a baseball reference in, Paul!) Also depressing.
I’d better go listen to some Journey to lift my mood. Right now! Thanks for all the condensed and important info, Paul.
Hi Paul – Thanks for the links and summaries; as always, very helpful. I find it interesting that only 64% and 67% of HBV eAg+ patients achieved full viral suppression at 48wks, despite there being no known resistance to tenofovir (and this is not too different from previously published rates of viral suppression on TDF). Have you found a good explanation for why, in the absence of resistance mutations, a sizeable proportion of patients don’t suppress, even in situations where we have a good marker of adherence in HIV co-infected patients whose HIV VL is suppressed? Thanks – Phil
Good question. At least part of it is the kinetics of HBV DNA response, which are much slower in the late phases than HIV. Can take many more months of Rx to suppress HBV than HIV, and even then some lower level viral load can be detected.
Paul
Interestingly enough, there has been only one reported cured patient with HIV, “the Berlin patient”, which happened to have recieved a SCT with a homozygous CCR5 mutation that confer immunity to HIV. Now i wonder, do I want to be immunosupressed for the rest of my life from a STC or having a nearly normal life with a pill? So, to keep the funny curbside, “Do not insult the pill, Alright?”