An ongoing dialogue on HIV/AIDS, infectious diseases,
May 8th, 2023
As the Public Health Emergency Comes to an End, How Are We Feeling About This?
As you no doubt heard, on Friday, May 5, 2023, the WHO declared the end of the global health emergency from COVID-19.
Here in the U.S., the federal public health emergency will expire on May 11. That’s Thursday, just a few days from now.
These events reflect two realities that, while seemingly contradictory, make these decisions reasonable — my constitutionally worried ID-doc mentality notwithstanding.
On the one hand, COVID is far from gone. Our patients, family, and friends are still getting this pesky bug, many of them now repeat episodes. And it always bears mentioning that, for certain people with weakened immune systems or multiple other medical problems, COVID is the cause, or the trigger, of severe illness. Some will get long COVID, though fortunately the incidence of this complication has declined over time.
Some worry about the increase in cases that will likely occur in the South as summer heats up and people move indoors. Or they are concerned about the most recent genetic offspring of Omicron, the scarily named Hyperion (XBB.1.9.1) or Arcturus (XBB.1.16).
All valid points. But let’s look at the other side of the current reality. Deaths due to COVID globally and in the U.S. have been below April 2020 levels and stable for over a year. The same holds true for hospitalizations for severe COVID-related illness.
The cause? Widespread immunity, giving protection from severe illness:
By the end of 2022, an estimated 99% of the US population had some form of immunologic exposure to SARS-CoV-2 (infection or vaccination or both). https://t.co/7iioxJUG8h
— Paul Sax (@PaulSaxMD) May 2, 2023
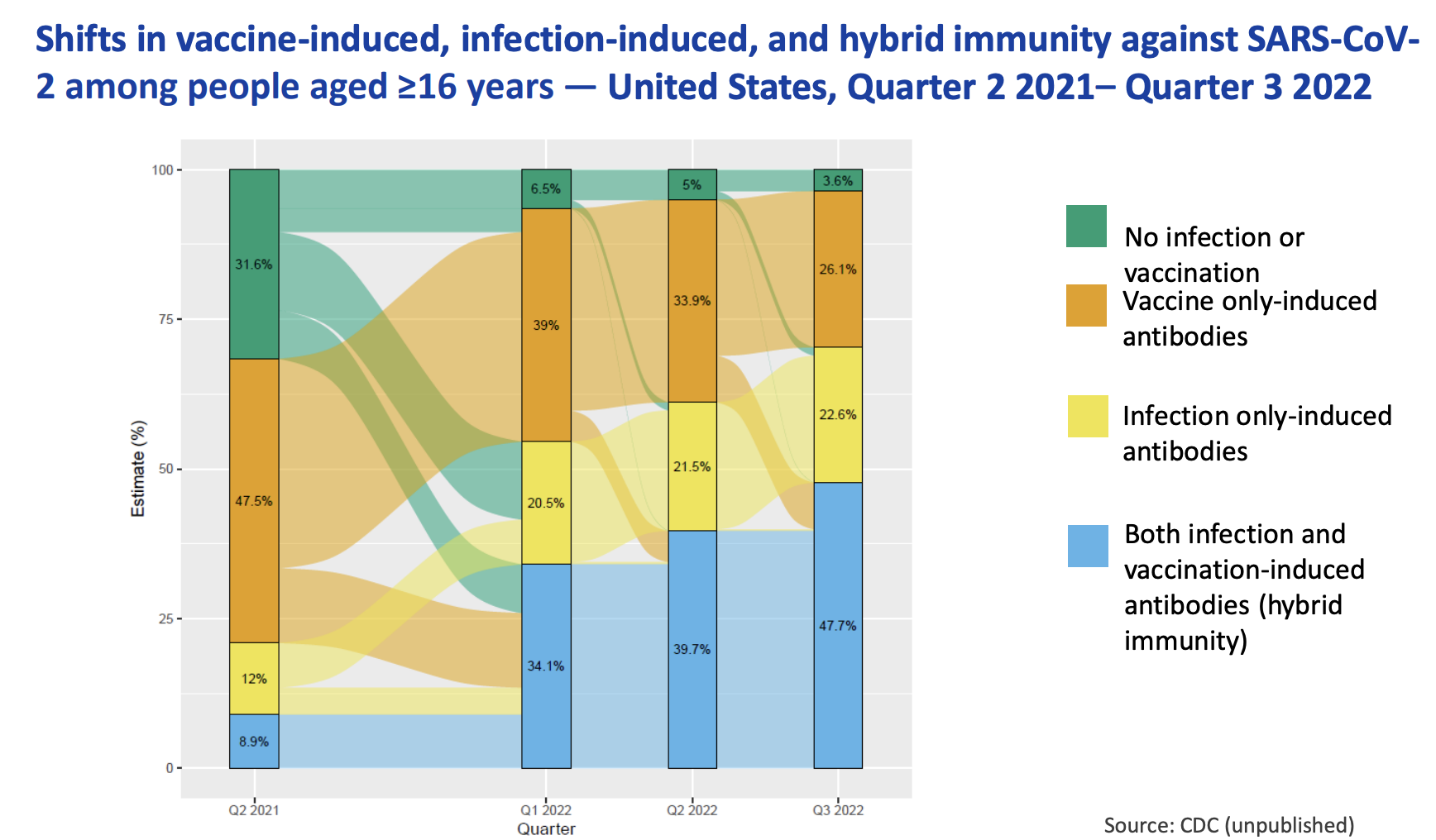
If you don’t like that study, here’s the CDC’s version, which they presented last week:
So COVID isn’t gone. But it sure is different now.
Importantly, not gone also are innumerable other infectious threats, including RSV and influenza and tuberculosis and Lyme disease and malaria and Staph aureus and you-name-it. No global or federal emergency for them — though I suspect first-year ID fellows all think we should have one for staph.
The passing of the COVID emergency inevitably brings to us ID docs certain feelings and recollections, even if it’s just the creepy feeling that if we let our guard down this SARS-CoV-2 thing is going to pounce again.
Even writing that makes me nervous. To be concise, it’s a combination of relief and trepidation.
So … how are you feeling about this?
Interested in hearing from both the ID and non-ID community!


Non-ID person here. I would feel better about the end of the COVID emergency if I thought we were prepared for the next pandemic, and/or prepared to deal with a more virulent and highly infectious strain of COVID-19. But the reality is that the emergency will end, and life will go on. I will continue to take any and all personal precautions that I think are necessary, including masking in places where appropriate.
Non-ID, retired MD here. I am very concerned because of the lack of adequate reporting & tracking of cases. My husband is young elderly, eats nutritiously, and exercised regularly until recent illness. He had mild chronic lymphopenia, had Covid twice but beat it, but now it’s worse from radiation therapy. It may be permanent. Yes, we can and do wear high quality masks when out. But we live in a rural area and need to travel for the concerts & museums that make a real life. We carry our lunch, but it was depressing to eat in the car a 2nd time for dinner. We did that when the pandemic was worse. So we eat out where there is more table spacing. But we really need info as to when & where the pandemic is worse, so that we can for those times adjust our lives. I do feel left adrift. Understandably, he won’t “live in the bunker” forever. I’m so afraid of him being one of those “well, he was immunocomprised, it’s unfortunate” cases.
The end of the “emergency” status for the continuing worldwide pandemic, and the endemic nature of COVID in the US scares me in that these changes may be used to justify lesser efforts at collecting data that reconfirms the continuing benefits and safety of vaccines. One of many significant challenges that gained traction for the purposes of purely political power,”identity” and as being revealed, money, reaching our highest court, the Supreme Court, are the continuing antivaxxer misinformation campaigns. These groups are still actively attacking the ability of whole communities including public health departments, school districts, doctors’ offices and more, to protect themselves via mandates for vaccines. They are doing so with attorneys in the courtroom. We are not just going to be unprepared; we are going to find ourselves with our hands tied behind our backs by the politicians, and the attorneys who can make a buck at the expense of the lives of all the rest of us. Doctors who know their patients can work with the individual patient to design a personal plan of care including if a vaccine is truly more risky than the disease. Politicians, judges and the courts cannot. We need as much continuing data as we can get going forward. Additionally, even before the fall, every health care provider and organization needs to continue to frequently state the facts. Our only hope is that the truth stated over and over again, can outpace the lies that have normalized dangerous misinformation.
Gail, thank you for sharing this. You expressed a concern many of us hold. Your diligence is to be applauded.
The tendency to minimize deaths by allocating them to the immunocompromised continues to be a political club that won’t go away. Best wishes to you and your husband
I’ll offer a PSA:
Public health is not the same as personal health.
Public health determines a level of acceptable level of death and disability based on many factors including the ability of the health care system to function. In some ways, public health policy reflects the health of our economic and healthcare systems. It focuses on harm reduction and risk mitigation at a population level. The WHO says the pandemic hasn’t ended, but the public health emergency has. That makes sense from a public health perspective.
Personal health is altogether different. Public health said “get the first vaccine available to you, including J&J”. Personal health said “isolate a bit longer and get an mRNA vaccine that is far more effective”. There is a different tolerance for death and disability at a personal level. The end of mask mandates doesn’t necessarily reflect the need for people to mask for personal health.
As someone just diagnosed with long COVID (thanks to taking my first significant risk in 3 years by taking a nonstop flight wearing a KN95), I caution against communication that minimizes the impact to personal health by citing decreasing numbers – it can come across a bit insensitive.
Thank you, Dr. Sax for eloquently articulating your thoughts about these official declarations about COVID. Thank you, as well, to the thoughtful readers who responded. Please continue to address COVID as it evolves! I shared many of your thoughts with both worried and cavalier family members and colleagues during the “official” pandemic as the sole voice of reason. Carry on!
My greatest feeling is one of frustration at our failure to learn from this emergency. It’s disheartening to expect that we won’t do better next time – maybe worse, if the next vaccine effort will not succeed as quickly.