An ongoing dialogue on HIV/AIDS, infectious diseases,
March 8th, 2020
As Testing Ramps Up, Diagnoses of Coronavirus Disease in the U.S. Will Soon Increase Substantially — How Will We Respond?
Brace yourself. As coronavirus disease (COVID-19) occurs at multiple locations around the United States, the number of confirmed cases here is about to increase big time.
There are two reasons:
- New infections
- More testing
Believe it or not, despite statements by certain politicians, COVID-19 tests still cannot be ordered by any clinician who believes it should be done. In many parts of the country — including, as of today, Massachusetts — a local health department continues to be the only place to get the test. These state labs have limited resources, and hence must offer the test only to those who have a clear exposure, or have a severe respiratory illness without other obvious cause.
That’s about to change. Two of the largest commercial labs in the country, LabCorp and Quest, announced that they have tests ready to go.
Plus, multiple academic medical centers plan to modify their existing molecular diagnostic assays by adding the coronavirus genetic sequence as a target. This will enable testing to be done rapidly “in house” at hospitals that see the highest volume of critically ill and immunocompromised patients.
And not a moment too soon. By all objective measures, our testing has been woefully inadequate, meaning that the reported number of diagnosed COVID-19 cases are the proverbial tip of the iceberg — an iceberg of the pre-climate change magnitude.
Consider — today’s report shows 484 cases reported with 20 deaths. Remember that these tests were done mostly on the sickest people. That’s why our mortality rate is so high at 4.1%.
By contrast, consider South Korea, which already has widespread disease and an aggressive testing policy (they have apparently done over 140,000 tests). They have diagnosed 7,314 COVID-19 cases, with 50 deaths, for an estimated mortality rate of 0.6%.
If we apply that 0.6% mortality rate to the 20 deaths we’ve had here, this would mean there are already around 3,000 cases in the United States. We just haven’t been testing enough to find them.
(Apologies to epidemiologists for the crude estimates. Hey, math is hard.)
There are several ways we could — as clinicians, scientists, media, public — react to this surge of cases that will inevitably dominate the headlines in the coming weeks.
On the negative side is panic, which will bring with it further hoarding behavior, conspiracy theories, and unproductive accusations. On this last one, I’d like to emphasize what I posted here about the people I know who work at CDC and the department of public health — they are not to blame:
Agree. The people I know who have worked at @CDCgov and at @MassDPH have been hard-working, mission-driven, and science-based individuals who want to do the right thing. They must be given the resources they need. https://t.co/iukkqLkRMb
— Paul Sax (@PaulSaxMD) March 7, 2020
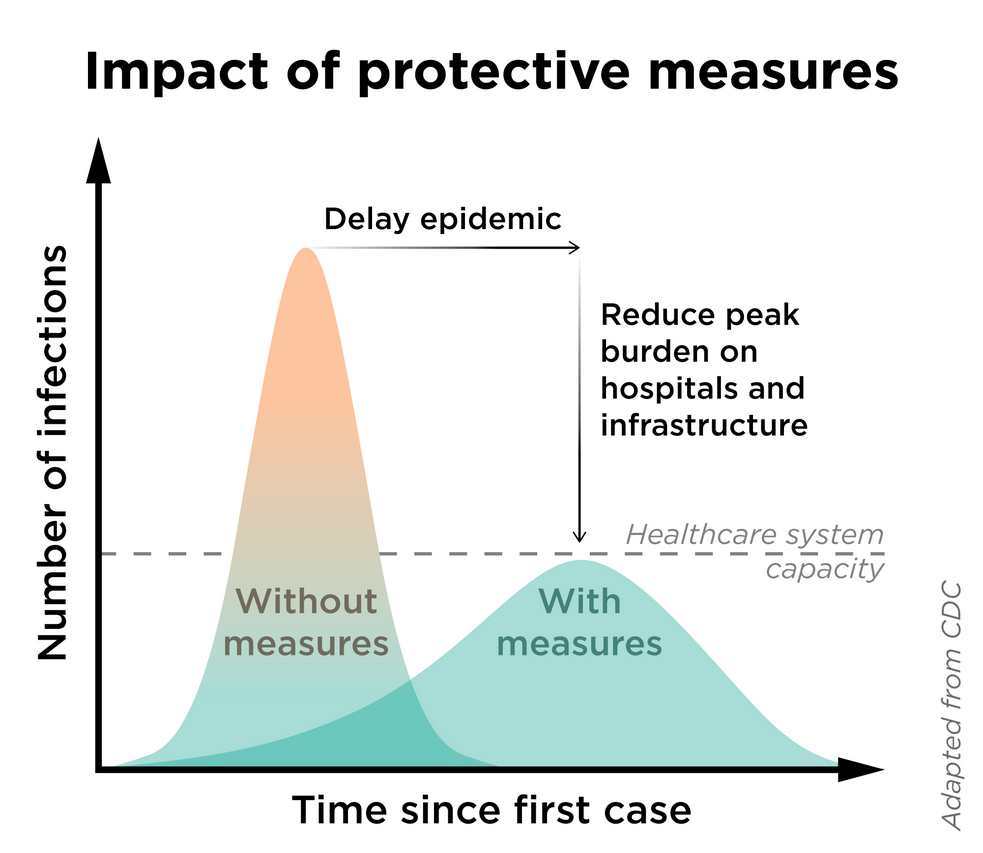
Another terrible reaction will be to suppress the information.“I like the numbers being where they are” is not an effective mitigation strategy — a strategy which will be critical to prevent the overburdening our healthcare system (see figure).
What I’m hoping for?
Let’s welcome the accurate data, even though the numbers will sound scary. It’s time for expansive tests for COVID-19, even introducing them as soon as possible on our multiplex respiratory virus testing platforms.
Such information will give us a much better sense of the spectrum of the illness here, as well as the risk factors both for COVID-19 acquisition and severe disease. It will also allow us to institute more sensible infection control policies, to allocate resources where the disease is most prevalent, and to construct viable strategies to turn the tide against the epidemic.
When Knowledge is Power confronts Ignorance is Bliss during a public health emergency, give us the first one every time.


Do we know how long one must have been infected before a test can be positive? What’s the window period?
2-14 days is the current best guess for the incubation period. The time to positive testing is likely on the order of 4-5 days.
More thoughtful and balanced information from Dr Sax.
Yes tears for all clinically appropriate cases not NOT for any cold or worried person. That will only drive false positives.
The problems with testing are myriad
The biggest issue is who will test the ill?
Private physicians and staff cant risk a 2 week quarantine due to exposure
You cant bring sick people into an office commingled with well patients
Test centers must be organized to handle ill patients. Drive thru testing should be organized in short order
Full disclosure I am not a physician. I have been paying attention to medical blogs to stay informed on this virus. Most say the virus is spread through physical contact not airborne. If medical office staff practice standard procedure (gloves, hand washing, masks) wouldn’t that suffice? As far as commingling with well patients isn’t that a daily situation in a Dr’s office? I just think a drive through testing center is a bit of a stretch.
Per the CDC COVID-19 is believed to primarily spread through droplet (coughing/sneezing) and may live on surfaces for up to 48 hours.
https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fabout%2Ftransmission.html
Thank you for this post.
I am a physician in Manhattan, New York City. M’y patients are asking me if I can test for COVID-19. Last week Quest said they had no test kits. I am glad to hear that has changed.
I do have a few patients who merit testing.
I’m all for actually getting good data from more testing. Your comments about “Another terrible reaction will be to suppress the information.“I like the numbers being where they are” is not an effective mitigation strategy” is reminiscent of recent articles about medication errors at major chain pharmacies, who in response to the press stated that they have exceptionally low rates of medication errors, which is more suggestive of underreporting than of exceptionally good systems.
I would much rather have accurate data than “good numbers.”
We must start by giving us the capacity to test every patient in our hospitals that is having any respiratory symptoms. The COVID carrier that masks as a COPD or pneumonia will destroy our most precious resource in the upcoming weeks- able bodied healthcare workers.
Paul,
Please give your thoughts on serological testing used for broad based surveillance. I think we need the full picture in our numbers including those who were infected and have now cleared the virus.
Including these subjects in the denominator of our estimates will provide data to the public that might be reassuring.
Thank you Dr. Sax, once again for you thoughtful and sensible post.
The number of deaths reported in the US is only confirmed or highly suspicious COVID-19 cases. It is likely that during January/February, we had more extensive disease burden among hospitalized patients with respiratory infections who were unable to be tested or the treating clinicians did not think that they should be tested because they did not meet the restrictive criteria set by the CDC (i.e. did not have direct travel to Wuhan, China or have direct contact with a known COVID-19 case). I think that the 0.6 mortality rate may be somewhat accurate, but I suspect that we have much more than 3,000 cases here in the USA.
People do not die instantly of COVID-19. If the average person dies in 3 weeks, then the 20 individuals who have died suggest about 3000 people had the infection 3 weeks ago. The number would be much higher given the new infections that would occur over the last three weeks.
Thanks Dr. Sax, for useful advice as always. I think the main issue now is how to implement a sensible social distancing policy.
well. hi to all, sorry for my english, i’m not english native, as about the window period, here in Italy this is about 5-6 days, this match with the average of the chinese study seen on NEJM, the cllinic is about a person who present cough and fever since 4-5 days but do not complain of feeling sick than a decise worsening of the clinick with important dispnoea and ipocapnic ipossiemic and alcalose pattern besides this leucopenic neutropenic on cbc, i hope this can serve.
Thank you for this thoughtful, factual balanced article. This sane examination of this topic is welcome. Please continue to inform us and know that your work is appreciated.
We constructed a mathematical modelling on late Jan about the medical resources (numbers of beds occupied in isolation ward and ICU) in China, which is similar to the current situation in the US.
This calls for the implemented anti-transmission measures (e.g., closure of schools and facilities, suspension of public transport, lockdown of city) and further effective large-scale interventions spanning all subgroups of populations aiming at obtaining overall efficacy with at least 70% to ensure the functioning of and to avoid the breakdown of health system.
Breaking down of healthcare system: Mathematical modelling for controlling the novel coronavirus (2019-nCoV) outbreak in Wuhan, China
https://www.biorxiv.org/content/10.1101/2020.01.27.922443v2
This Asia Times article discusses the role that a rapid response has played in mitigating the illness and trajectory of the infection rates.
https://webmail.pedsnw.net/owa/redir.aspx?C=11kjK1qOIEX42sajuhWeQEAcXKPNrv_JPMYDowtgjoxjn3XDxcTXCA..&URL=https%3a%2f%2fasiatimes.com%2f2020%2f03%2fwhy-are-koreas-covid-19-death-rates-so-low%2f
I would like to read your blog.
Is it possible that Covid 19 was in China and the US earlier than we thought? Both my husband and I, both healthcare workers in WA state, and we both had a severe respiratory infection in November 2019. I developed super infection, which required two rounds of antibiotics. I have heard other WA state healthcare workers tell me the same.
Hi Paul, I never cease to enjoy your thoughtful perspectives. This is needed now more than ever. I’ve been concerned about the impact of COVID-19 on emotional wellbeing and had opportunity to co-author this blog at CredibleMind. Please share with colleagues helping people cope and loved ones who may be anxious.
https://crediblemind.com/articles/calm-in-calamity-coronavirus-2
I am surprised that the number drops to zero much faster “without measures”! Is that really true?
So a 0.6 mortality rate, but break it down by susceptibility to death by acute disease, including factors such as increased age, pre-existing pulmonary issues and other pertinent co-morbidities, and see what mortality rate is among the healthy.
Then do the same for flu and compare THOSE numbers.
The panic has been driven by fact that public has not had explained (as dine here). That the reason there are so FEW infections is that we only test those where we have high rate of suspicion and THAT only occurred recently, I have a hard time believing this thing suddenly exploded out of China. Seems far more like that while it was brewing to critical mass there, patients 0 thru several hundred left China and spread infection.
I’d like to see us test 1000 random people in each country and see how many test positive and best case if can test for antibodies. Bet we find a significant number are positive and either fought it off or had minor symptoms they either mistook for flu (could this be reason flu vaccine is historically in 50% range in effectiveness—it ain’t all flu).
I’m not a doctor but just asking.
Dr Sax for President!
What can you tell us about virus shedding before symptoms? How are you contagious before coughing and sneezing?
It is my understanding that vinegar kills bacteria and viruses. Is it likely to kill Covid 19?
Coronavirus is very threatening for all… So, as I was searching form many of the precautions and safety rules, I found this video useful for all https://youtu.be/O8GtGHy4GpI
Seattle Times published an article last year that Influenza related American deaths during flu season in 2018 were 80,000. Perspective seems completely avoided. How can the hysteria be contrasted and reconciled?
The coronavirus is now testing the global population in ways no microbe has for a century. Much is unknown about exactly how this particular virus causes the disease known as COVID-19, but much IS known about how best to stop it. The basic principles of disease mitigation that have worked reliably for millennia—hygiene and social distancing—are no less applicable today.
Source;https://notesread.com/
“Thank you for sharing such great information.
It has help me in finding out more detail about HIV patient with coronavirus“