An ongoing dialogue on HIV/AIDS, infectious diseases,
July 13th, 2021
To First-Year ID Fellows, Incredible Gratitude and Respect — Especially for This Past Year
Two things happened earlier this month in most U.S. hospitals — the academic year started, and the number of people hospitalized with COVID-19 reached a low point not seen since the early phase of the pandemic.
(No, hospitalizations are not down everywhere. We ID docs are very much aware that COVID-19 isn’t over. But the national numbers are historically low — single digits in my hospital right now.)
The turn of the academic calendar means it’s a good time to express gratitude to the ID fellows who just finished their first year — especially this year, because unless you went through it yourself, I would argue that these past two years could not have been more difficult for these trainees. Historically so.
Let’s start with early 2020, the second half of senior medical residency for most ID fellows just completing their first year.
In normal, non-pandemic years, senior medical residency acts as a wonderful consolidation of all that’s learned in the preceding two years. With fewer clinical demands, senior residents can master the intricacies of inpatient medicine, teach on intern and medical student teams, handle their outpatient clinics, check out subspecialty electives, and participate in research projects. Senior residents also plan the next phase of their lives by either applying for fellowships or looking for a “real” job.
And yes, there’s a certain amount of gliding on cruise control. Plus all kinds of wonderful camaraderie, celebrations, and parties.
But 2020 offered nothing like this for senior medical residents. Here’s Dr. Eric Bressman’s account when he was Chief Medical Resident at Mt. Sinai Hospital, describing spring 2020 in New York:
Pretty soon we were just completely inundated, both at Sinai and Elmhurst, Elmhurst even more so. And while we were working a lot on the weekends, during the week it was all administrative in terms of completely remaking the structure of our floors, completely remaking the schedules of the residents to design a safer experience, both for the patients and for the residents. And we were pretty quickly working 24 hours [a day] to try and get that done, and I probably didn’t have a day off for two months.
Safe to say that there was no cruise control for these residents. Lots of unplanned inpatient coverage needed, especially in the ICUs. And the celebrations and parties? Prohibited for infection control reasons.
Plus remember this — for people who had applied to and then matched in ID, they chose ID before COVID-19 was even a thing. What had they signed up for?
Yes, when they arrived to start fellowship last July, case numbers were down in some regions. But the first year of ID fellowship already has enormous challenges for multiple reasons, even without a pandemic. It’s hard! Rewarding too, but no piece of cake. A brief summary, including several items highlighted in a previous post:
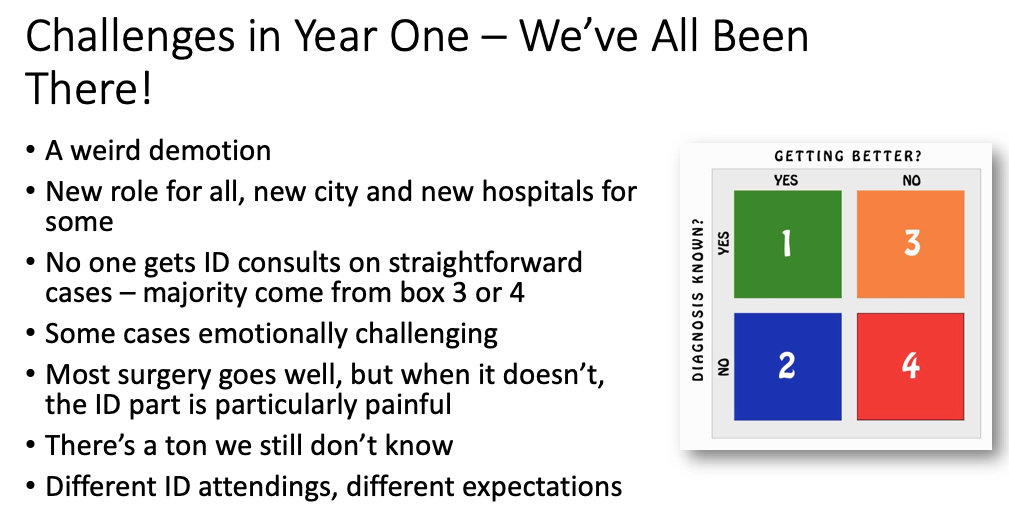
I didn’t previously mention the “weird demotion,” but it’s true. July rolls around, and BAM! First-year ID fellows become beginners again. An internship redux, only now their entire clinical service consists of patients that medical and surgical teams can’t handle on their own (orange and red boxes in figure above). Challenging!
Then, as 2020 progressed, into the tricky mix of first-year ID fellowship came COVID-19 again.
In Boston, it was like a ghoul from a horror movie prematurely left for dead, only now back and just as strong and as scary as ever. COVID-19 wards reopened. ICUs again had critically ill patients, some of them shockingly young. Consults and pages about testing, treatment, and infection control all took off, including at night — but this time the rest of the hospital activities continued at the same time, in parallel. There was plenty of non-COVID-19 ID work to be done. Yikes.
I distinctly remember walking into our fellow work room one dark afternoon in December, two fellows sitting there nervously at their computers. For a bit, no words — then one said to me, quietly:
We all have COVID fear …
A completely understandable reaction to a completely terrifying situation, one we all shared. Only I strongly suspect, for reasons cited above, that the level of post-traumatic stress disorder experienced by first-year ID fellows seeing COVID-19 cases go up again probably clocked in at the 99th percentile or higher.
It was the combination of recapitulating their difficult senior residencies, the legitimate concerns about being overworked, the need to be the expert on a disease with still so many unknowns — plus the very real fear of personally catching the infection.
Which is why, when the first supplies of the vaccines became available to healthcare workers, and queries went out to prioritize vaccine recipients, the answer for us in ID was a no brainer. First-year ID fellows! Of course!
So thank you, just-graduated first-year fellows. You did an amazing job under such difficult circumstances. Enjoy both the relative calm that second-year brings with it, and this helpful owl trying to interpret a CT scan:
Trying to read a CT when radiologist read is pending pic.twitter.com/O919wIg2hK
— Adi (@IDdocAdi) July 11, 2021



I’m a just graduated first year fellow and I can totally relate with everything you said! I appreciate this post and thank you so much for acknowledging everything we went through. #theptsdisreal
The ID fellows at the Brigham are extraordinarily fortunate to have you as a mentor.
Based on the past experiences and JAMA viewpoint – Rethinking HowAntibiotics Are Prescribed (doi: 10.1001/jama.2018.19509), I tried to make a simplified approach ‘I-OCD’ for Antibiotic Decision Making in Clinical Practice.
1. Does this patient have an Infection? Focus/Site?
2. Does this infection require antibiotics? Likely Organism?
3. Cultures (blood/body fluids) obtained before empirical antibiotics?
4. Daily check for Dose/Duration/De-escalation of antibiotics