An ongoing dialogue on HIV/AIDS, infectious diseases,
July 5th, 2023
The Yin and the Yang of Cabotegravir-Rilpivirine: Part Two, the Limitations
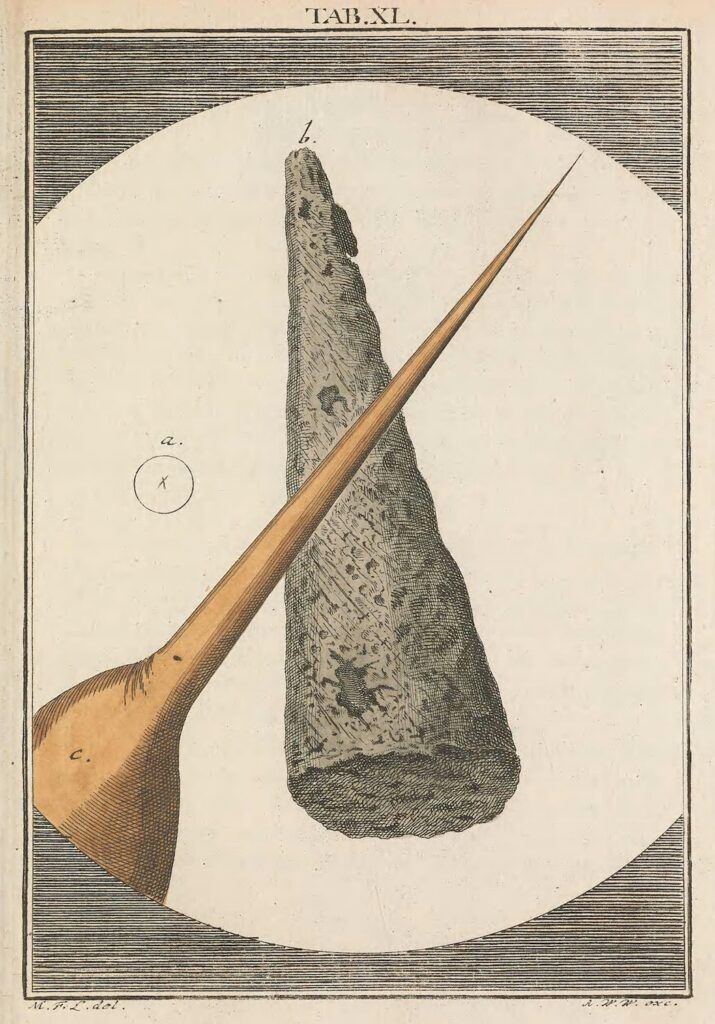
Tip of Needle and Stinger of a Bee, from Martin Frobenius Ledermüller’s Microscopic Delights (1759–63).
In the last post, I cited examples of patients who are doing much better now because they are on long-acting cabotegravir-rilpivirine (CAB-RPV). One of these patients said he preferred it because it’s “simpler,” by which he meant he no longer had to go to the pharmacy to refill his medications each month.
I’ll grant for him it’s simpler, but for the rest of us? Because when I teach ID fellows about antiretroviral therapy, I have a slide that is entitled “Limitations of CAB-RPV.” It includes nine bullet points, meaning not only am I breaking the rules of good slide-making, but more importantly, it’s proof that CAB-RPV is anything but simpler.
Here are the bullet points, with further discussion — because if you’re an ID/HIV doctor and don’t yet offer this treatment to your patients, it’s important that before you do so, you go in with your eyes open:
Complex logistics to implement and monitor. Based on an optimistic interpretation of the voluminous direct-to-patient advertisements for the regimen, some might think that doctors can just write a prescription for CAB-RPV and voila, a patient can go to the pharmacy, pick it up, and get started.
Think again.
At our site, we have a dedicated, energetic, and wonderful nurse practitioner who took making this treatment option available to our patients an important priority. Without her leadership, it’s no exaggeration that we never could have done it (thank you, Cathy!). Chatting with colleagues around the country, I’ve heard that all these clinics that offer CAB-RPV have someone who took this on as their primary responsibility. It could be a nurse as in our case, or a doctor, or an ID pharmacist, or a case manager. I guarantee that all these fine people have in common great administrative skills, executive function, and perseverance.
In short, if you don’t have a “champion” going through the logistics of how you’re going to get the medications to your clinic and administer them, you won’t get very far. If you want to supplement this post with a comprehensive video covering the myriad issues you need to consider before getting started, I highly recommend this outstanding summary by the Mountain West AIDS Education and Training Center, with Ji Lee, PharmD.
It’s over 20 minutes long. “Simpler” indeed.
Risk of treatment failure with resistance, even with adherence to the regimen. True, the risk is small (around 1%) — but we have become accustomed to guaranteed treatment success with dolutegravir- and bictegravir-based regimens, with essentially zero risk of resistance with good adherence. Not only can CAB-RPV treatment fail, but the consequences (integrase inhibitor and NNRTI resistance) means that boosted-PI regimens become the default option, with all their disadvantages.
An important paper recently appeared in Clinical Infectious Diseases highlighting risk factors for resistance derived from the clinical trials:
Virologic failure despite adherence to CAB-RPV is rare (1%), but it happens, with bad consequences (INSTI and NNRTI resistance). Risks:
– RPV RAMs
– Subtype A6/A1
– BMI > 30Really important paper in @CIDJournal, with lead author @profchloeorkin https://t.co/lopLUqmXjH
— Paul Sax (@PaulSaxMD) June 21, 2023
While some of these risk factors can be assessed or intuited ahead of time — for example, I won’t use this treatment in people with any NNRTI resistance, not just RPV resistance — and anecdotally treatment failure can rarely occur even in the absence of risk factors.
Cost. Cabotegravir-rilpivirine costs more than oral ART, which has become increasingly expensive, even when accounting for inflation. This has consequences for insurance coverage, and, as any HIV clinician can tell you, our treatments are now aggressively managed by many payers. With CAB-RPV, there is often a complex and lengthy benefits check and pre-approval process before the treatment can start.
And this cost issue only refers to the medications. It doesn’t account for the nursing, pharmacist, case manager, or physician time to get the approvals, to prepare the medications, to administer them, and to chase down people who miss appointments.
All that takes time — time that could be spend doing other things. As economists will remind us this is a cost too, especially in a time of widespread healthcare provider shortages. I am aware of at least one HIV clinic that has had to limit their new patient enrollments for CAB-RPV due to this shortage.
Injections must be delivered by a healthcare provider. CAB-RPV administration is not like a simple insulin injection or flu shot — watch an instructional video, you’ll see what I mean. (Go to Video Library, “How to administer injectable medicine”).
In addition, most practices carry a very limited supply of medications available for in-office injections. One of my patients, a Boston “snowbird” spending the winter in a warmer southern state, contacted me saying he wouldn’t be back in time for his injections, but he was confident he could get it from a primary care clinician he sees sometimes when he’s down there. I told him that unless this doctor had a large practice of people with HIV (they didn’t), there was zero chance this would be possible — which turned out to be the case. He went back on oral ART until April, when he returned to Boston.
Fortunately, the company that makes CAB-RPV posts a locator for alternative sites for receiving the injections, which is a great idea both for when patients travel and for clinics that don’t have the resources to offer this treatment themselves. It’s not clear how often people are using these sites, however, and availability is limited. For example, the only one I see in the Boston-area requires a trip to Providence, around 50 miles away.
Frequency of visits. Most people receive their CAB-RPV at their doctor’s office, coming in six times a year for the two injections. Before that, while on stable ART, visits typically occurred every 6 months, or even annually.
Allow me to do the calculation: that’s four or five extra trips into the clinic each year. Not easy for many people, and an additional cost (parking, transit, time out of work, away from family).
Injection site reactions. Like anything that involves a needle piercing the body, these shots hurt some people more than others. In the clinical trials, most reported them as mild or moderate in severity, but a small number did find them severe enough to stop treatment. This is consistent with our experience in clinical practice.
Pain relievers, ice- or warm-packs, stretching all can help. And patient education ahead of time is critical!
Limited data for patients with resistance, history of treatment failure, or viremia. So far, the exciting data on using CAB-RPV in people who are viremic and can’t take oral ART has not been replicated elsewhere in a prospective study — just anecdotes here and there, as in the 4th case I cited in the previous post. As a result, use of CAB-RPV is explicitly not recommended in treatment guidelines for virologic failure — even though such a practice would arguably be even more transformative than CAB-RPV’s current indication.
Also applicable for everyday patient care would be a large cohort of people with a prior history of treatment failure, but no documented integrase inhibitor or NNRTI resistance. When will we see those data?
Not recommended during pregnancy and breast feeding. As with every novel HIV treatment, this important patient population not been prospectively studied, at least not yet. But given the increased volume of distribution seen during pregnancy, and the low resistance barrier of rilpivirine, I would strongly discourage its use.
Does not treat or prevent hepatitis B. One of the great benefits of tenofovir is that it’s also our best current treatment of hepatitis B. Switching to CAB-RPV removes this advantage, and indeed one of the participants in the licensing trials contracted hepatitis B during the study.
Lesson for us — make sure to check hepatitis B status prior to starting CAB-RPV, and update vaccination as needed.
These limitations to CAB-RPV are understandable. After all, this is the very first long-acting ART option, and the fact that we have it at all is remarkable. Furthermore, we can expect progress in this area as other compounds become available, preferably some that can be administered even less often, or at home.
But for now, all of us doing HIV care must dial up our counseling skills when patients ask whether they should switch to long-acting injectable ART — and they will ask, since the advertising bombards them regularly. As noted previously, this treatment option gives us a great chance to engage in shared decision making, to elicit patient preferences and to deliver information at the appropriate level of medical literacy.
They should hear about the benefits, and the risks, and the practicalities. Give them plenty of time to ask questions and join them in the decision process of whether it’s a good idea to switch.
Then you should both watch this video, because even with these limitations outlined here, it’s truly a miracle how far we’ve come with HIV treatment. And about that we can be very grateful!
(Thanks to Dr. Darcy Wooten and Cathy Franklin, NP for reviewing this post, and Mass General Brigham for producing the video.)


Thank you for that remarkable video. Your voice, the tone of your voice, your facial expression, and your overall demeanor exemplify the empathy and compassion that are the aspiration of all dedicated physicians. I cannot help but reflect in sadness how these time honored qualities are being killed off in American medicine by the cut throat, private equity, money grabbing capitalism that has come to rule since the election of Reagan and then the steady march toward regressive right wing dominance.
We too have had to halt our new cab-rpv starts due to limited nursing bandwidth.
I know a hospital-based ID practice that hasn’t started at all — no “champion”.
Still, glad we have this option. It can only get better from here, right?
In reading blog, we noted that you avoid Cabotegravir in any patient with an NNRTI resistance. Can you explain your rationale?
Thanks,