An ongoing dialogue on HIV/AIDS, infectious diseases,
September 4th, 2016
The Most Common Question About the New HIV Testing Algorithm, Answered
 A primary care doctor in the Boston area recently emailed me this question:
A primary care doctor in the Boston area recently emailed me this question:
Hi Paul,
A 28yo woman had a positive 4th gen +Ag/Ab assay, but a negative HIV-1/2 differentiation assay and negative HIV viral load. She had no signs of acute HIV, but is not using condoms with her partner, whose HIV status she doesn’t know. We repeated the test yesterday and she is again Ag/Ab+, the remainder of the test is pending. If we get the same results again, would you try to get a Western blot?
Thanks,
Morgan
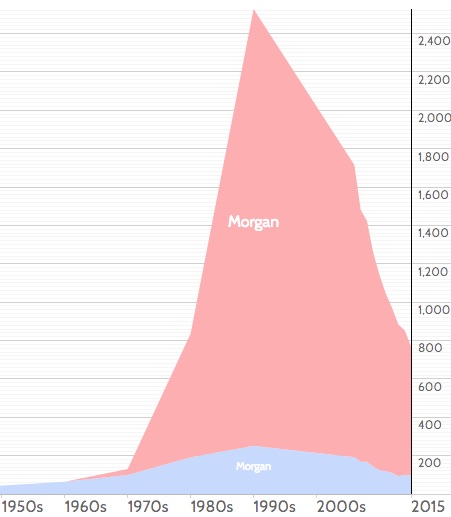
[Not her real name, but I did just meet a doctor named “Morgan” for the first time, so feel compelled to comment here. If you look at this name popularity graph, I guess we have an explanation for the rarity of this name among MDs to date. Did you know Morgan was the 30th most common girl’s name in the USA during the 1990s? So expect more Morgan MDs soon!]
“Morgan’s” question has come up numerous times since the new algorithm kicked in, and it reflects a misunderstanding of what the newer tests can and can’t do.
Remember, the big advance in moving from the 3rd to the 4th generation screening test was the addition of p24 antigen to the sensitive ELISA antibody. This shortens the window period from HIV acquisition to a positive screening test by about a week.
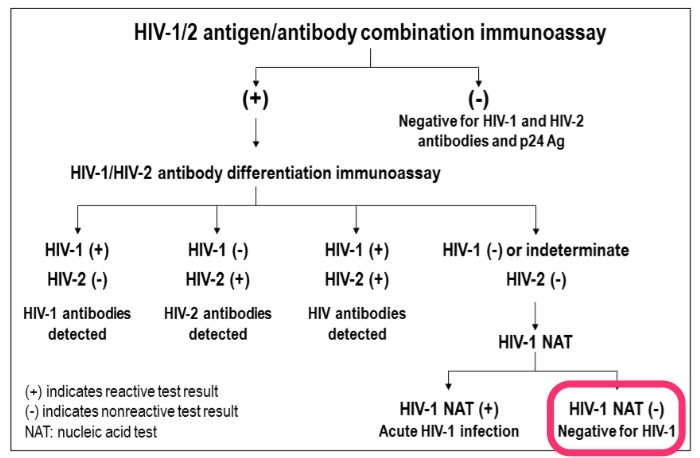
The second big change is that the confirmatory test is now a differentiation assay, an antibody test that tells us if the person has HIV-1 or HIV-2 — the Western blot couldn’t do that. If it’s negative, an HIV RNA (viral load or other nucleic acid test, NAT) is recommended, since the screening test (with its antigen component) is more sensitive early in disease than the differentiation assay. Importantly, the Western blot — may it R.I.P. — offers no advantage in sensitivity over the FDA-licensed differentiation assay (in fact, it’s a bit worse), so won’t be of help in these cases.
However, if the HIV RNA is negative, then we’re dealing with a false-positive screening test, and this is exactly the scenario in the email. For relatively low-risk patients, this is a far more common explanation for the positive 4th generation screen/negative differentiation assay pattern than true acute HIV infection, just as it was for a reactive ELISA with negative Western blot.
How much more common? In this review (pages 34–36) by the primary architect of the algorithm, Bernie Branson, we get some numbers:
The specificities of 4th generation HIV assays are >99.6% — which means that as many as 40 per 10,000 test results may be false-positive. In most populations of persons testing for HIV, the prevalence of acute HIV infection is 2 per 10,000 persons tested or less. Thus, the frequency of false-positive immunoassay results usually far exceeds the prevalence of acute HIV infection.
For those who prefer all this stuff explained graphically, here’s the key figure from the latest HIV testing guidelines; I’ve highlighted this case’s results in bright fluorescent pink:
To summarize:
- The 4th generation screening test shortens the window period after HIV acquisition.
- The differentiation assay tells us if the person has antibodies to HIV-1 or HIV-2.
- In screening test positive/differentiation test negative cases, the next step is an HIV RNA (or other NAT).
- Most (but not all) will have a negative HIV RNA, and therefore don’t have HIV.
In other words, false-positive screening tests will continue to happen — even with the new algorithm.
Thank you very much for your attention, and enjoy this amazing video, which must have taken its creator many, MANY hours to complete. Wow.
And if there are any other doctors named Morgan out there, I look forward to hearing from you.
(H/T to IMS for the video, though it looks like many millions of people have beaten us to it.)


Paul, thanks for the clarification. Thanks also for the video. I’ve seen it before but can never get enough of it. Here’s another one: https://www.youtube.com/watch?v=uHisd9P2M-Y
All the best,
Mimi Breed
Just wondering about the diagnosis of acute HIV-2 infection. The above algorithm specifies that HIV-1 NAT testing to be performed (which I presume was the negative result) – but what if the patient was recently exposed to HIV-2? Could it be missed in the type differentiation assay and then only detected using NAT?
The short answer is that the algorithm doesn’t account for acute HIV-2 — you’d need to send a dedicated HIV-2 viral load. However, transmission of HIV-2 is so uncommon in non-endemic areas such as the USA that this will not be clinically relevant often enough to incorporate this step into the algorithm.
Paul
Paul, “Morgan’s” question was a near exact replica of a MKSAP review question I encountered a couple of days ago, i.e. positive 4th gen assay, negative differentiation test, negative viral load. The question was, “What’s the next thing that should be done?” The answers (and the percent who responded with that answer) were A) Repeat HIV-1/2 antigen/antibody combination immunoassay in 6 weeks (16%); B) T-cell subset testing (2%); C) Western blot HIV-1 antibody testing (36%) and D) No further testing (45%). So that Western blot inclination lingers….at least among those prepping for their IM re-certification!
And thanks for that incredible video. Like you said: wow.
Hi Paul- I wonder what the common causes for the false-positive testing are, and what additional testing may be necessary to determine the cause of the false-positive? I’ve had false positive testing with syphilis in the past, but wonder what else is on your differential. Thanks!
Various things can have been reported to cause false-positive HIV screening tests (autoimmune diseases, multiple transfusions, even flu shots!), but most of the time no cause is found, and no further w/u is needed.
Paul
Thanks Paul. What about Elite Controllers? Could Morgan have identified a case? Where do they fall in the algorithm?
“Elite controllers” have positive HIV screens then positive differentiation assays for HIV-1. Some do have very weak antibody responses over time, but not permanently (i.e., you’ll detect antibody most of the time).
Persistently negative HIV antibodies in patients with established HIV-1 infection are very rare. Situations include patients treated EXTREMELY early during acute HIV infection with weak antibody responses (but of course were once HIV RNA positive), and a subset of rapid progressors who can’t develop humoral immunity to the virus. They also would be p24 antigen and HIV RNA positive.
Here’s an example of the latter (rapid progressor, seronegative):
http://ofid.oxfordjournals.org/content/3/1/ofv209.full
Paul
But what about the reported 7% who have a negative viral load. Are the new NAT tests so sensitive that everyone who is positive is detected. I thought that was the only justifiable use of the WB today or is this passe.
Hi Ellen, I don’t understand your question — 7% of what group has a negative viral load?
As noted in my post, the HIV differentiation assay (an antibody test) is more sensitive for detecting antibody than the WB.
Paul
Dear Paul Sax,
In your HIV testing algorithm, it is recommended that If the HIV 1 and 2 antibody test missed to detect HIV infection, you recommend to go for HIV 1 RNA PCR or NAT. If that individual has HIV 2 infection or if the individual has both HIV and 2, then the possibility of missing HIV 2 infection could be there. So the recommendation must be to have HIV PCR for both separately to rule out the false positive case. Though the prevalence is low with HIV 2 infection, we should not miss a single case of
HIV 2 infection.
Dr S.Murugan
Hi, I get different answers from different labs so I go to the very top. You write:
“Remember, the big advance in moving from the 3rd to the 4th generation screening test was the addition of p24 antigen to the sensitive ELISA antibody. This shortens the window period from HIV acquisition to a positive screening test by about a week.”
But what is a reasonable answer to the question: “How long is this window period in healthy adults in low risk circumstances?”
My question is whether HIV DNA tests (PCR) designed for Early Infant Diagnosis for HIV (Qualitative) is good enough to use as the NAT tests in adult clients? In Low and Middle Income Countries esp in Africa where i am based, we only have VL and EID as the NAT tests to confirm/rule out acute HIV infection.
I have heard that the HIV DNA PCR qualitative test (Roch Taqman) is specifically designed for blood samples from pediatrics in whom i understand there is high white cells/cc of blood. The sensitivity of the test is said to be lower in adults especially if there are already on ART.
Also it is important to highlight that the VL was not designed to diagnose HIV hence, it can be very difficult to interpret if TND is obtained (Target not Detected) or indeed if the VL is on the low side. VL >1000 copies/mL you can be pretty sure the patient is positive.
Dear Paul Sax,
Thank you very much for your explanation and a great VDO.
What about the false positive HIV NAAT test to detect early infection?
I had a case of positive HIV NAAT as a screening test for a clinical trial on HIV cure treatment from other institution but refused to participate. He subsequently tested negative on 4th generation test at 1 and 3 months later. The case could have been misinterpreted as a cured case on early treatment?
Paul,
Isnt this algorithm bound to fail if the infection took place, say 7 days prior, before p24 antigens are produced to be detected by the combo test? Should we supplement it with doing a RNA PCR test if the HIV 1/2 p24 combo test is negative?
Also, I have patients every once in a while who show up after having completed the PEP course initiated within 72 hours post exposure. Should we still follow the above algorithm, with the window period starting from the end of the PEP medicine?
Thanks,
Gaurav
1) You are correct that it cannot pick up very early acute infection — which is why we should supplement this algorithm with HIV RNA (viral load) testing if we clinically suspect acute HIV, or if the patient says his/her exposure was very recent.
2) Yes, but would have low threshold for using HIV RNA in those finishing PEP since presumably it was high risk exposure that got them on PEP to begin with!
Paul
Paul
Thanks Paul. Personally, I am a bit hesitant in using viral load tests for patients finishing PEP (despite them being extremely keen on it!) because of the theoretical risk of viral suppression sustained after ART. My advice to them is to rely on antibody test 4-6 weeks after PEP for conclusive results.
What has your experience been with post PEP testing? PEP patients are typically the most anxious group I have to deal with in my clinical practice!
Cheers,
Gary
1) Excellent point about early use of vl testing.
2) Yes, very anxious. But no transmissions yet! Fortunately this is a very rare event in most PEP cases.
Paul
1) Good point about VL testing.
2) Standard (Ag/Ab) testing 4 wks, 12 weeks after exposure. And yes they are anxious, but fortunately transmission very rare in this setting!
Paul
RE: coughing on airplanes.
Recently while returning on an 11 hour flight from Europe I shared cabin space with two coughers. One sat directly in front of me. It occurred to me why don’t the airlines offer masks? I concluded it’s a legal thing or just denial or perhaps there is no scientific evidence. Then I wondered what iif in the future I would travel with some so Much could offer it to some one. I would offer a price of candy or chocolate and then innocently say “Bye the way I have a mask if you like?”. Worse case I guess I could put a mask on (but th I would feel really neurotic). So far it’s been a week since returning home and I’m still healthy. The other thing I noticed is how many people cough into th it hand and then touch everything…maybe when th ask you if you packed your own suitcase etc they could explain proper cough etiquette/hygine? Or do we travel with small printed cards we could hand the cougher with pictorial instructions?