An ongoing dialogue on HIV/AIDS, infectious diseases,
December 3rd, 2017
Why, Even with Depressing Predictions About Flu Vaccine Effectiveness, We Should Still Recommend and Get It
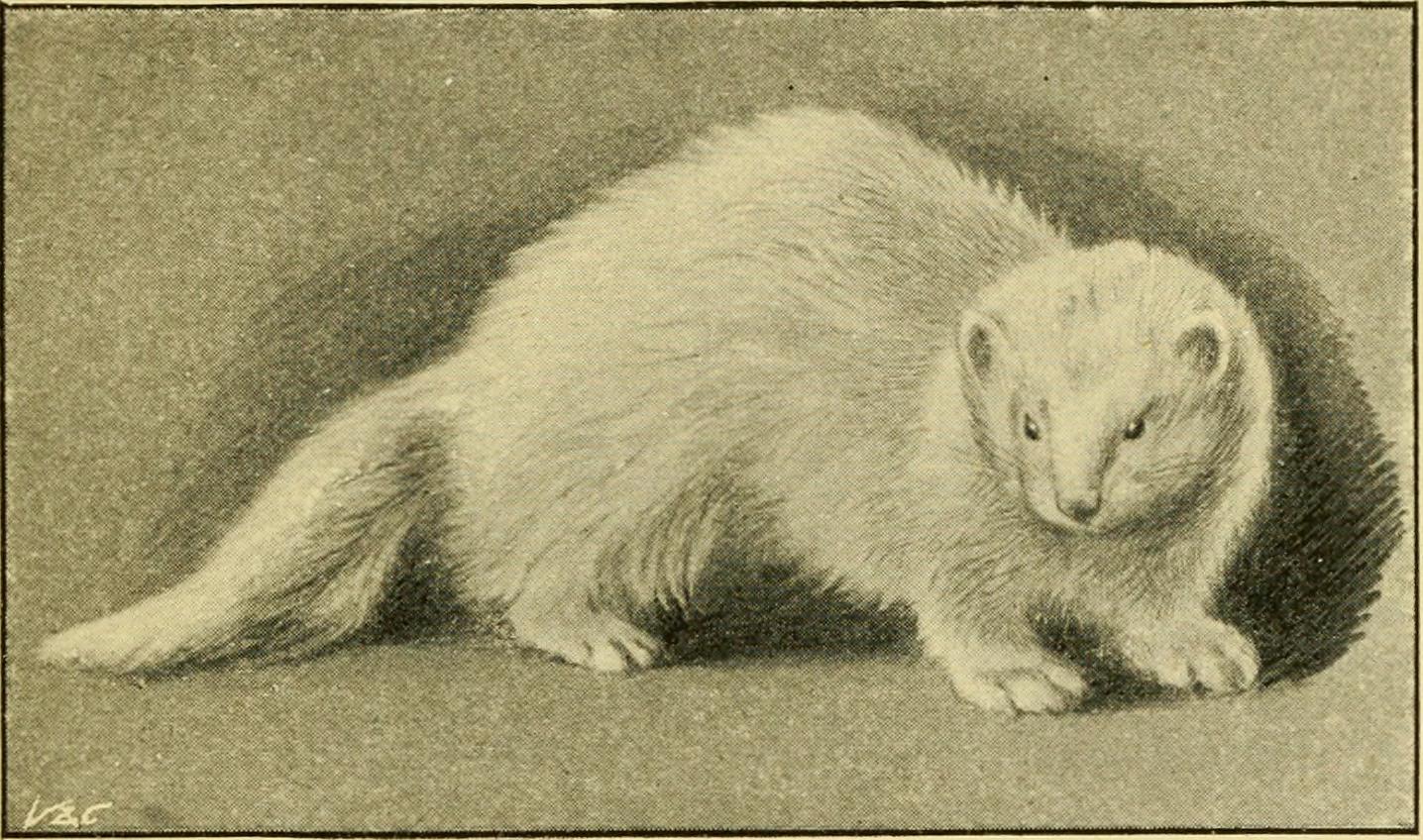
Image from “Ferrets : their management in health and disease with remarks on their legal status”, 1897.
Each year, the print and broadcast media round up a bunch of experts on influenza and ask them to predict the severity of the upcoming flu season.
Most of the time their responses are noncommittal — predicting how bad the flu season will be year to year is tricky business, akin to picking stocks, making 12-month weather forecasts in an almanac, or naming the winner of the World Series during spring training.
But this year is different. A particularly bad flu season in Australia, mostly due to H3N2 influenza A, has public health officials concerned we’re going to see the same thing here in the Northern Hemisphere.
And our flu vaccine’s estimated effectiveness against the H3N2 strain?
This low effectiveness isn’t due to a strain-vaccine mismatch. The problem appears to be related to alterations in key flu vaccine proteins during egg-based vaccine production. Or, if you prefer a more technical explanation, here’s a quote from an excellent perspective on challenges in the flu vaccine published last week in the NEJM:
Antigenic characterization using ferret reference antiserums indicates that egg-propagated vaccine viruses acquired changes in the hemagglutinin that subsequently altered antigenicity against circulating strains.
(You have to love that sentence.)
Regardless of the mechanism, even by the meager standards we hold the flu vaccine, this 10% number is a disappointment.
But this low efficacy notwithstanding, you might note that the CDC, public health officials, and the vast majority of ID doctors still strongly recommend the vaccine. They/We do so for several reasons:
- The Australia experience with H3N2 may not be recapitulated here. Although H3N2 is widespread in the USA early in the flu season, circulating flu strains change even within an individual year. In this terrific summary, read how even flu experts grapple with the vagaries and unpredictability of seasonal flu activity. And that person next to you in the subway with the cough and drippy nose may have influenza B, against which our vaccine provides much better protection.
- Even partial protection is better than none. A recent paper found that the flu vaccine prevented influenza-related hospitalizations, suggesting attenuation of severe illness. It adds to existing data supporting that the vaccine provides benefit even when it doesn’t completely prevent the illness.
- If you’re a healthcare provider, you owe it to your patients. This is especially the case if your patient population includes babies, or pregnant women, or the elderly, or people with cardiopulmonary disease, or individuals struggling with obesity, or immunocompromised hosts. Good chance this covers 100% of clinicians!
- It’s the only thing we’ve got. At least on the vaccine front, this is sad but true. There are various common-sense activities we can educate our patients about, but the adherence to these practices won’t be high.
- It’s safe. The vaccine does not cause the flu. Furthermore, the vaccine does not cause the flu. Finally, the vaccine does not cause the flu. Got it?
We doctors, nurses, PAs, and pharmacists can be forgiven if the the weak efficacy data might take some of the energy out of our annual recommendation. But let’s try to keep giving the vaccine.
And hey, you smart vaccine researchers working on that “universal” flu vaccine — we’re rooting for you!
So is the ferret.


see http://www.anvita.info/wiki/Influenza_Virus_Vaccine and
http://www.anvita.info/wiki/Influenza
for a summary of influenza and influenza virus vaccine.
Influenza is a respiratory pathogen that replicates in ciliated columnar epithelial cells of the respiratory tract and is transmitted via aerosolized droplets of nasal secretions or contaminated hands. It is true that recovery from influenza infection produces IgM, IgG and IgA, but I see no attempt to explain how an IM injection will afford much protection from a respiratory pathogen. It seems as if a surgical mask would be much more effective… and I have often wondered why the nasal vaccine was dropped rather than fixed. I can’t help but envision financial incentives are at play here.
Ohhhhhhhhhh if I had a nickel for every time I heard one of my HIV patients complain about how the flu shot *gave* them the flu or how they don’t need a flu vaccine because they “never get sick” I could retire.
‘tis the season for arguing until I’m blue in the face…..
In 2001, I spent 10 days in bed with the flu. I remember very little of those 10 days, except how much my back hurt from laying in bed so long! Unfortunately, my husband got it at the same time and could not even take care of me. I joke that were it not for canned Progresso soup, we would have starved to death, as we were both incapable of doing any more than heating a can of soup and then running back to bed. I tell this story to explain why we both get the flu shot every year, no matter how lousy the virus match seems to be. Yes, as a healthcare provider, I want to protect my patients and not give them the flu if at all possible. But the memory of those 10 days is still painful. I have found that my patients who are most eager to get the flu vaccine have either had a similar experience, or someone close to them had a similar experience.
P.S. Our pantry is already stocked with Progresso soup cans. Just in case.
This is why I get the flu shot. A horrible experience with the flu. And if it doesn’t work 100%, well, it was worth a shot.
(The pun just appeared there like magic.)
As a helpful trick, the flu shot should be offered not in the form of a “question”, e.g. would you like to get your flu shot today? and more as a summary for today’s visit: “First you will get your vitals, then you will get your flu shot, then you will see your MD”. It is more assertive and harder to opt out from.
so much for shared decision making
Sheldon…how reasonable and well studied! Thank you! I taught Logic and um….thinking…oh…oh..my metaphorical red pen is dancing with excitement with some truly blatantly illogical posts here. In the excitement to justify offering up not only their own arm…but trying to force our’s (and it appears to be with the hopes of a bullied patient who is hopefully kept ignorant by a system living up to all that was fought for against thimerosal…a shot in the dark). Sigh!
Transparency is always the answer…not an overbearing system that doesn’t hold the government, doctors, or bureaucrats up to the highest of standards of respect to who you care for. I think maybe some posters here owe the vaccine movement a huge thank you for cleaning up the shots…not a gag…or trickery.
What’s your take on prophylactic Tamiflu versus this year’s flu vaccine for patient’s whose spouse is diagnosed with influenza A?
Dear Dr. Sax,
I have, for years, monitored the world for pandemic influenza. I led the US government’s team that tracked the spread of H5N1 as it emerged in Asia and spread to Europe. Also successfully anticipated the vaccine drift of 2007/2008 [https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=3&ved=0ahUKEwjU3bbi9fHXAhVM2oMKHWKfDiwQFgg0MAI&url=https%3A%2F%2Fwww.hsgac.senate.gov%2Fdownload%2Fwilson-testimony-pandemic-surveillance-100407&usg=AOvVaw3eNlWi0s9FWEN1UF7o9D45]
I am also the private intelligence analyst who provided warning of the 2009 H1N1 influenza pandemic [https://doi.org/10.1080/02684527.2016.1253924].
For several months now I have been working to de-escalate the claim of “severe” associated with the 2017 Australia influenza season. And I did contact Dr. Sullivan regarding the report she just published in NEJM. I have been monitoring Australia for years, and I will tell you they have seen worse seasons. In this case, the Australians changed their mortality reporting protocol in midseason. ***Most importantly, they reported increased case counts but did not associate that with an actual increase in clinical severity. I will point out there continues to be no international standard with which to define “severe” as it pertains to seasonal influenza. With this entire discussion, the key question is, “What is TRUE severity as it pertains to an influenza season?”
Nuance. Nuance that requires closer scrutiny of the data before attempting to alert the world to a hemispheric threat. If you monitor the media from the UK and CAN, you will see they picked up on this claim of severity- some outlets even declaring the cause of the “severity” was A/H2N2, a virus not seen since the pandemic of 1957. Some claimed Australia had seen the worse season in the last 50 years. Apparently 2009 didn’t happen…
So, I am surprised to see NEJM propagate this information in such a way as to potentially mislead its readers. No drift variant of A/H3N2 was identified to be emergent and in dominance.
For context, here are the latest statistics for the last 17 seasons comparing the Australia season to the US season:
1. You have an 88% chance of seeing the same influenza type dominance (i.e. type A or B) in Australia also appear later in the US.
2. However, you have about a 50% chance of seeing the same influenza A subtype dominance (i.e. A/H1N1 or A/H3N2) in Australia also appear in dominance later in the US.
3. Of the roughly 50% of seasons with a matched influenza A subtype (H1N1 or H3N2), about 88% exhibited strain match as well (e.g. A/Fujian/411/2002(H3N2).
4. Four vaccine mismatches were reported during this period, and two of these times involved A/H3N2 drift of a strain seen in dominance in both countries.
I encourage your staff to review key measures of true severity for these 17 seasons. Examples include mortality data and ICU admissions. You will see the surveillance data is not uniformly standardized nor necessarily comparable between AUS and the US.
So, I would have been quite a bit more cautious attempting to claim the US was going to have a severe season simply based on the Australian experience. And to say we have an “early” season here in the US? Based on a five year baseline? Come on, we can do far better than that- especially given we have surveillance data going back further than 5 years.
No one will disagree we need a better vaccine. But hyping claims of severity is arguably a poor communication tool- particularly when our healthcare provider community is significantly split on mandatory vaccination of healthcare employees. They are also significantly split regarding whether to recommend influenza vaccination to their patients. This kind of communication (after hearing debunked claims of “pandemic potential” with Zika and “pandemic potential” with seemingly every new influenza virus described in Asia) continues to erode trust in public health officials. Indeed, this conversation claiming the vaccine will be 10% effective plays right into anti-vaccinators’ hands- many of whom are our fellow physicians.
Careful thought is required when handling health security intelligence, and something to monitor closely as the season progresses. NEJM needs to be circumspect in 1) ensuring what was reported out of Australia was accurate in the first place and 2) understanding how this information may be perceived by our healthcare community and patients.
James M Wilson V, MD FAAP
Director, Nevada Medical Intelligence Center
University of Nevada-Reno
That is some pretty bad argumentation.
The effectiveness rate of flu vaccines is, indeed, depressing. Several other meta-analyses have found no evidence for a reduction in hospitalisation days or complications, especially in healthy adults, no evidence for increased protection of patients through healthcare worker vaccination, no effect on working days lost in healthy adults, et cetera.
That it is safe (nevertheless causing serious complications in anecdotal cases), is hardly an argument. Homeopathy, too, is safe. Does that mean it’s reasonable? The same can be applied to the “only thing we’ve got” argument.
“Partial protection is better than no protection” is nonsense. Especially when the importance of herd immunity is, correctly, stressed among other vaccines.
I hate to have to make this point, but… people ARE getting filthy rich selling these vaccines. Not to mention quite some hours spent administering
them and – I do know the vaccine does not cause the flu – having annoying symptoms for some hours afterwards.
This entire article contains only one valid argument: the article referenced. All the rest is appeal to emotion, humour, false equivalence,…
Given the questionable efficacy these products have, it’s about time we physicians stop cowering behind lousy arguments to defend bad medicine.
Cheers
I’m involved in one of the Australian surveillance systems focused on hospitalisations with confirmed influenza.
Our impression from this year was that there were an increased number of admissions with confirmed influenza (more than twice that the previous year in the same sentinel hospitals) except in WA and NT. Tthe clinical severity of the admitted cases (based on ICU admission and in-hospital mortality) was similar to previous seasons. Because there were more patients with flu coming through the door, this translated to more ICU admissions and in-hospital deaths.
An overall summary of the Australian season, based on a a number of different surveillance systems, has recently been published by the Australian Department of Health.
http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-ozflu-flucurr.htm/$File/2017-season-summary-22112017.pdf
Flublock influenza vaccine is not egg-based, eggs are not used at any point at all in its production.
Hence “egg-propagated vaccine viruses acquired changes in the hemagglutinin that subsequently altered antigenicity against circulating strains” would not seem to be possible
It would be interesting to see if this vaccine is more efficacious during this flu season
Any chance the Brigham will switch to cell-based FLUCELVAX next year to avoid the mutation issues with egg-based vaccines? (e.g. this year’s issue http://www.pnas.org/content/114/47/12578 )