An ongoing dialogue on HIV/AIDS, infectious diseases,
October 14th, 2019
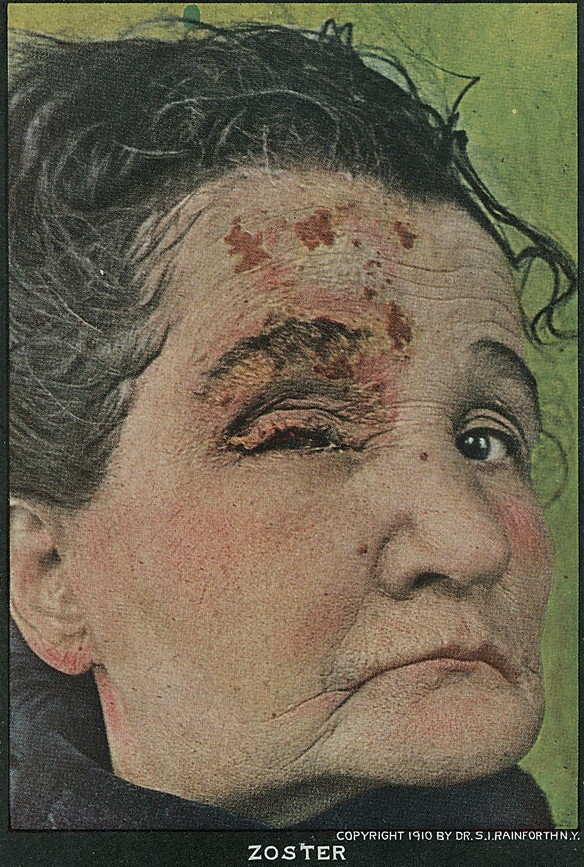
Common Questions About the Shingles Vaccine — Answered Here!
Here’s an interesting email from my friend and ID-colleague Dr. Carlos Del Rio (shared with his permission):
Went Tuesday to see my PCP for a routine visit and had my second dose of Shingrix that day. I had gotten my first dose about 3 months ago and had severe chills and even a fever of 38.5 after the first dose. With the second dose the response was not as severe but did have chills and rigors for about 18 hrs. Stupid of me, but the next day I went to get my labs checked, and everything was fine except my HS-CRP which was 14.72 (nl < 10 and in the past I had been < 1.0).
Anyway…..Shingrix is a good vaccine but it is a tough one to take and really gives you a nice TNF storm!
For the few of you out there in ID-World who don’t know him, you must understand it takes quite the force to slow down the high-energy machine that is Carlos. He is the very definition of indefatigable. So it’s not surprising he told me he went to work after both shots, rigors and all.
(Brief aside — congratulations, Carlos, on your well-deserved award!)
But Carlos’ post-shingles vaccine experience reminds me that we’re now two years into the recombinant zoster vaccine (RZV, Shingrix) era, and that immunization for this common adult infection — shingles, or zoster — has brought with it all sorts of new questions.
So here are a bunch of common ones we ID doctors field on a regular basis:
- Who should get it? The vaccine is recommended for essentially all immunocompetent people over 50. So if you were born anytime before October 1969, this means you. People conceived during the Woodstock music festival or right after the Miracle Mets won the World Series are off the hook, at least for a few months longer. Two shots, separated by 2-6 months.
- “Immunocompetent” adults — so nobody else? While immunosuppression is not a contraindication to the RZV, the data supporting its use in this population have not yet informed current guidelines. For now, it’s totally reasonable to offer RZV to people over 50 receiving low-dose immunosuppression, or to those with stable HIV on treatment, or to individuals who have had an autologous stem cell transplant. For higher degrees of immunosuppression, adopt an individualized approach — and remember that there is a theoretical concern that the adjuvant in the vaccine might stimulate organ rejection or a flare of an underlying autoimmune condition. We’ll see if this turns out to be a legitimate worry, so far it hasn’t.
- No upper age limit? Use your judgment — if it’s a healthy 88-year-old with few medical problems, go ahead and give it. The risk of shingles increases as we age, and such a person will likely live several more years and could benefit from the vaccine. However, if it’s someone with multiple serious comorbid medical problems, then skip it. And yes, there are side effects — see Carlos’ email — which might be difficult for the frail elderly to tolerate.
- What about people younger than 50 who have had shingles? While it’s understandable that they might be interested in the vaccine, it’s not been tested in people under 50, and is not formally recommended in this group. Reassure them that recurrent shingles is actually quite rare, especially within the first few years of an attack.
- My patient never had chickenpox. Should they still get the zoster vaccine? Generally yes. For people born in the U.S. before 1980, essentially all have latent infection with varicella zoster virus — they either had a mild case of chickenpox or don’t remember having it. There might be a small fraction of people over 50 who never had chickenpox, test negative for antibody, and don’t want to risk the side effects of the vaccine. For them, consider the vaccine optional! (Many would recommend the chicken pox vaccine instead.)
- How long after a case of shingles should my over-50 patient wait before getting the vaccine? No one knows. But since active zoster boosts a person’s immune response, it makes sense to wait at least until the current episode has completely resolved. I then add some additional time derived from the sophisticated ID time machine calculators. “At least 6 months” sounds reasonable, doesn’t it?
- We had a shortage of the vaccine, now it’s now been more than 6 months since some of our patients had their first dose. Do they need to start over? Fortunately (for many reasons), no. Just give it when it becomes available.
- Speaking of the shortage, what’s going on? Because of high demand for the vaccine, there have been widespread shortages of RZV ever since the vaccine became available. While these seem to have eased somewhat, especially in the last 6 months, not all practices or clinics or hospitals have it in stock. Fortunately, there’s a handy vaccine finder tool that I hear is quite reliable for pharmacies that offer the vaccine. Many hospital-based clinics also have it (we do).
- Should I still give the new vaccine to people who got the old one? Definitely — not only is the RZV vaccine more effective, but that original live-virus vaccine (Zostavax) becomes less effective over time, and works less well when given to older patients, especially those over 70. If your patient got the live virus vaccine more than 6 years ago, they may not have any residual protection at all.
- I hear the side effects are pretty bad — could they be worse than shingles? While no doubt the new zoster vaccine causes more side effects than most other vaccines, the clinical trials showed that serious side effects — those leading to death, hospitalization, need for urgent medical care — were no more common in vaccine recipients than in those who got placebo. Educate your patients that they might experience arm pain, fevers, fatigue, and myalgias and that these symptoms could be bad enough to have an impact on their daily activities. (This happened in 17% of study participants.) What this means practically is that I don’t recommend giving the zoster vaccine the day before a major life event, travel, or a demanding job requirement. And no harm taking a dose of acetaminophen or ibuprofen for symptom control.
But let’s go back to Carlos for a moment, and how these side effects he experienced compare to herpes zoster:
And to be clear, Shingrix side effects way milder than having shingles!
Completely agree! My experience — arm pain (check), fatigue (check), myalgias (check), and low-grade fever (check). But it was all over in a day, I promise.
And with the acknowledgment that we ID doctors see cases of zoster on the more severe end of the disease spectrum, we have all seen shingles accompanied by a host of really nasty complications. These include encephalitis, stroke, facial nerve paralysis, corneal involvement, vertigo, bacterial superinfection, and, most commonly, disabling unremitting pain (post-herpetic neuralgia) — pain for which there is often little effective therapy.
So the simple answer to the last question — are the side effects from the vaccine worse than shingles? — my answer is an emphatic no! I still strongly recommend it for my patients, colleagues, and friends of a certain age.
And look, my colleagues agree:
Hey #IDTwitter and #primarycare, doing a piece on the recombinant zoster vaccine (RZV, Shingrix), interested in your experience (clinician or recipient). It's more "reactogenic" than most vaccines, but has this changed your practice? @CarlosdelRio7 https://t.co/MXn40PG8k9
— Paul Sax (@PaulSaxMD) October 13, 2019
Back to the Summer of ’69 (the real one) …
(H/T, as always, to the incomparable Immunization Action Coalition site for clear, helpful information.)


Husband and I both got the first injection the same day. Wow, did our arms hurt for about 5 days. Around Day 3, I accidentally touched my husband’s arm while he was sleeping. He woke up immediately, and literally screamed. (Talk about feeling guilty!) But both of us know that a few days of pain is way better than having shingles. We’re due for injection #2 soon, and we will be there to get it!
I had an 85-year-old patient get shingles 5 or 6 years after getting the ZVL vaccine. He had terrible PHN that I thought was more like CRPS, and has never completely recovered. So older patients who can tolerate the RVZ vaccine should get it!
Any clue why the recommendation for RVZ is for adults 50+, but the recommendation for ZVL was, and remains, 60+ years old? Is that just an artifact of the clinical trial protocols?
Regarding Loretta’s question, because the incidence of shingles is lower at 50-60 than >60, the benefit of vaccinating with ZVL at the lower age would have been much less. Given the short duration of immunity, protection would be wearing off as the risk increases. So although ZVL did work at 50-60, and was approved by the FDA for this age group, the CDC never recommended giving it to this age group. It’s not that unusual for FDA and CDC recommendations to differ. RZV may have a longer duration of protection.
I spoke with a researcher at GSK earlier this year, and he told me the shortage was due to higher-than-expected demand related to the CDC taking the unusual step of recommending RZV over ZVL. He also pointed out that protection is good with a single dose, and it’s OK to give the second dose late (this is true for almost all vaccines), so we don’t need to sweat if a patient has trouble finding dose #2 “on time” due to the shortage.
Another potential use of this vaccine is in children who got immunosuppressed at an early age (typically liver transplants due to biliary atresia) and never got their varicella vaccine. (They also don’t get MMR despite some evidence of safety, which is another story.) I have to wonder if RZV might be a way to protect those patients from VZV, but I am not aware of any evidence. If anybody has done this or heard about it, I would be interested in what is known.
Thank you for that explanation, Jonathan!
As a genuine elderly patient with several comorbidities of the cardiovascular and metabolic variety (though I’m in pretty good shape for the shape I’m in) and who HAS HAD SHINGLES — lemme tell ya — YES GET THE VACCINE! SHINGLES IS HELL. Mine had no rash — yes, rashless shingles is a thing — so nobody could diagnose it for three months.
Finally the pain doc to which I was referred figured it out, and by then then it was too late for any but palliative treatment. I had postherpetic neuralgia seemingly forever. As soon as vaccine became available I got vaccinated. When Shingrex came along I was first in line. I can’t even remember if I had side effects from the vaccines, but I’ll never forget the awfulness of shingles.
Trust me — you don’t want to get shingles. GET THE VACCINE!
You mention that the vaccine is not recommended in people under age 50 who have had shingles because recurrent shingles is very rare. However, what if the person has already experienced recurrent shingles?
Recurrent shingles isn’t at all rare.
I’ve had several shingles recurrences and I’m immunosuppressed. My doctors strongly encouraged me to get Shingrix as soon as it was available.
I have a patient in her 60s who is taking Humira – is shingrix safe for her?
It’s probably fine, based on some data that will be presented shortly. Stay tuned!
Paul
I ran across a very good explainer and example of informed decision making a year and a half ago here- https://sciencebasedmedicine.org/should-i-get-the-new-shingles-vaccine/
You acknowledge your support of the vaccine based on selection bias. I very much prefer Dr. Hall’s essay but it exemplifies the potential problems with shared decision making. And I realize I’m off base somewhat, as such is not the express intent of your current comments.
While decision making based on highly selected experience will lead to no net harm in this situation, it certainly can do so in any number of other situations. So I appreciate your candor (and am undoubtedly guilty in other situations), comments to counter your bias might have been appropriate.
Dear Paul,
Thank you for this informative post, as usual! Our group recently submitted an abstract (accepted) to our national rheumatology meetings reporting our experience with administering the recombinant vaccine to over 400 rheumatology patients taking various immunosuppressants including TNF inhibitors, JAK inhibitors, methotrexate, steroids. Our retrospective review showed that the incidence of disease flares was ≤7% and side effects were 13.4%, lower than that observed in the general population. Both flares and side effects were mild, self-limited, and did not require a change in DMARD therapy. I’ve copied the link to the abstract below. Look forward to more formal studies examining safety and efficacy in this population! Thanks.
Elena Massarotti
Brigham and Women’s Hospital
Division of Rheumatology
https://acrabstracts.org/abstract/safety-of-the-zoster-vaccine-recombinant-adjuvanted-in-rheumatoid-arthritis-and-other-systemic-rheumatic-disease-patients-a-single-centers-experience-with-400-patients/
If not contraindicated because of health issues, I recommend taking ibuprofen right before the injection, and continuing ibuprofen as directed for 24 hours. Both based on personal experience and on first principles, NSAIDs may prevent or mitigate the inflammatory symptoms related to the immunization. Tylenol is less effective.
I disagree that the vaccine should not be offered to people who are elderly, frail and have multiple comorbidities. These are the people who are at highest risk of shingles and post herpetic neuralgia. We have an exclusive primary care home based geriatric practice with people with advanced frailty and multiple comorbitdities- average age of 89. We used to see multiple cases of severe shingles in exactly this population even in their 90’s and over 100. It is very difficult to predict life expectancy in this age group and we know that the vaccine provides some protection after the first dose. Since we have been offering RZV to our patients we have only seen 1 case in a vaccinated patient in his 90’s.
I received the vaccine two months ago. I got a fever to 102, extreme fatigue, and mild arm pain. Someone told me that she rubs the injection site vigorously after a vaccine and never gets arm pain, even from tetanus shots. Is that safe?
The adjuvant is really potent. Derivative from the Chilean soap bark tree. I suggest using cautiously in people with autoimmune/ auto inflammatory disease. I’ve seen 2 patients with ASIA (Autoimmune/Autoinflammatory Syndrome Induced by Adjuvants) following RZV. Both referred for Lyme disease because they had rash and myalgias. And remember to take the history of recent immunizations along with the history of recent new meds when patients come in with “allergic” reactions.
I am over 50 and generally healthy. I have Hyperthyroidism which is stable on Methimazole treatment.
I had chicken pox as a child, and a mild case of shingles a number of years ago.
Do I still need to have the vaccine?
Thanks, Dr Bronwyn Daniels
In regard to Shingrix, does anyone have any comments regarding dermatologists who perhaps have taken care of ~500 cases of zoster?
Since former shingles patients, and zostavax recipients were excluded from clinical trials of shingrex, how do we know the vaccine works in such patients? Seems like a leap of faith, with a twist of industry sponsored vigor!
If the first shot of shingrex engendered a robust immunologic response, can this not imply adequate immunologic stimulation, thus disqualifying the need for 2nd dose?
Since patients who previously received zostavax, or who had past history of shingles were excluded from clinical trials evaluating shingrex vaccine, it is a leap of faith to assume shingrix will work as well in these groups. Since this vaccine is fairly new, long derm data is in short supply documenting its true real world efficacy. I already have one patient with shingles one year post shingrex, it serves as a reminder of the less than complete protection afforded by this new vaccine.
I had shingles many years ago, and my chief complaint was itching! I have had several flare-ups. I plan to get both shingles injections. What is your experience with B12 (1cc) + B1 1/2 cc). It has helped many patients avoid PHN.
Miriam Post Menges.
For myself I have this conceit that I will recognize the rash on myself in the 1st or 2cd day and start antiviral Rx stat. And have minimal disease burden. Is this foolish?
Yes. I started treatment on day 2 and still had PHN (moderate, then mild) for close to 3 years.
I thought this vaccine was absolutely contraindicated in people who had received Zostavax vaccine.
Hi Diego Andres, thanks for raising an important point. For patients who received Zostavax, it is absolutely recommended they also get Shingrex. My 70-something parents are adherent but not pleased with this recommendation!
Sarah Williams APRN AAHIVMS
If Shingrix vaccine is given subcutaneously in the triceps area, is it just as effective as if it had been given intramuscularly in the deltoid area?
Dear Sir,
Recently I noticed that the ACIP said that ,”WHILE NOT CONTRAINDICATED SHINGRIX IS NOT RECOMMENDED FOR IMMUNOCOMPROMISED PERSONS.” This statement seems different then the one I just read in your medical narrative. Has there been new info released from the C.D.C/A.C.I.P. regarding immunocompromised individuals.? If so please me know.
Also, what can happen to an individual vaccinated with SHINGRIX while active with shingles?
Sorry about any spelling errors I’m trying to type in the dark.
Thank you
It’s been more than 18 months since first Shingrix shot. Should I still get the second inoculation?
What is the current thinking about giving Shingrix to patients with autoimmune diseases? I have a patient newly diagnosed with myasthenia gravis and am anticipating the need for longterm immunosuppression. While I would like to protect patient from herpes zoster (particulary herpes zoster ophthalmicus because he has one eye), I don’t want to make his autoimmune disease worse. Is Zostavax a better option at this juncture? Shall I give Zostavax and wait a month before immunosppression?
Thanks.
I had the 1st dose of the shingles shot and was absolutely miserable for 4 days as well as having an extremely sore arm. I can live with the pain of the shot but I am thinking about skipping the 2nd follow up dose because of the severe side effects.My question is .. Will I still get protection from the Virus by just taking 1 initial dose and skipping the 2nd injection? Also does the 2nd injection still going to cause the same degree of side effects that the 1st injection caused ?
i had the 1st shot but was moving and forgot the 2nd what do i do
I am 62 years old and received the first shingles shot in 1/27/20. It is now 3/13/20 and my left arm (arm that I received vaccine) has hurt since date of vaccination. Shoulder has hurt around rotator cuff deltoid area, left armpit area, left pectoral area and as of today, left forearm area which is very painful.