An ongoing dialogue on HIV/AIDS, infectious diseases,
October 29th, 2017
Cellulitis, Lyme, VZV, MRSA, TB, Tdap: Great Questions from ID in Primary Care
We’ve just finished our annual course Infectious Diseases in Primary Care, and once again our attendees — all busy clinicians — asked some excellent questions.
Below, a small sample:
- What is the drug of choice for cellulitis in outpatients who are allergic to penicillin? Importantly, this is about cellulitis — not abscesses — which means most are caused by beta strep (group A, B, C, G). If you can find a history of safe use of a cephalosporin, go with that. (Many of us ID doctors prefer cefadroxil to cephalexin, since the former is twice-daily.) If cephalosporins aren’t an option, one commonly cited alternative is clindamycin, though there’s increasing resistance to the latter among certain strep in the community, especially group B. Some would say that TMP/SMX is an option, but I’m not a fan. Levofloxacin is active versus most beta strep, so this also should be considered, even though it never appears in guidelines. The price of linezolid has come down since it went generic, but it’s still expensive, and not always well tolerated. But whatever you choose, remember that more than 95% of people with penicillin allergy aren’t actually allergic — have them get a skin test, and remove that penicillin allergy from their chart! So gratifying to do that.
- How long does the Lyme serology stay positive after treatment? Although Lyme serologies gradually decline in most patients, they can in individual patients persist for years, making follow-up serologies as a “test of cure” a particularly confusing practice — so let’s stop doing it! Importantly, this applies to both IgM and IgG antibody responses, which makes IgM antibodies an unreliable marker of recent infection unless they are correlated with recent-onset symptoms and exposure. Because there are no predictors of who will and will not have persistent Lyme antibodies, most of the time the diagnosis of reinfection relies heavily on clinical presentation. I hope someone out there is working on a reliable PCR or antigen test for Lyme — we really need it!
- One of my patients received the chicken pox vaccine, and now wants to get pregnant. Her varicella serology is negative. Should I revaccinate? Unfortunately, the varicella titers commonly used in clinical practice only reliably check for natural immunity, not vaccine-induced immunity. As a result, they are not recommended as a marker of varicella vaccine efficacy. But the bottom line is that if you have a clear record she received her vaccine, there is no need to revaccinate your patient — or check titers.
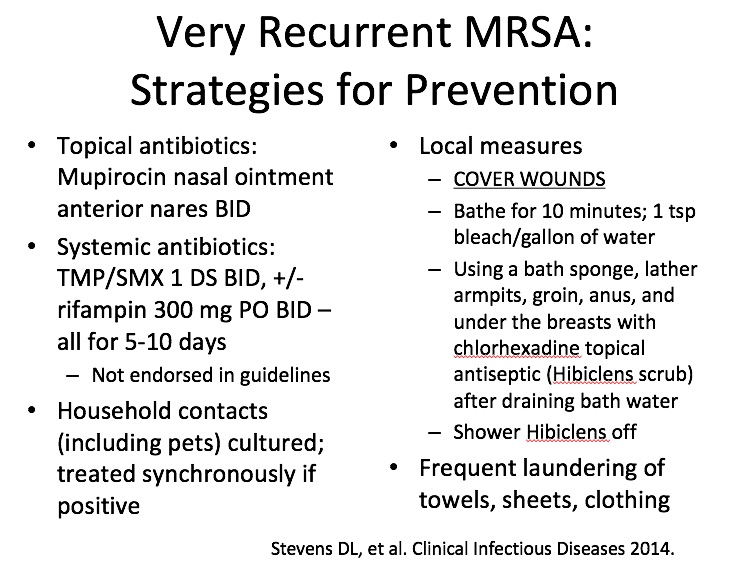 How do you manage recurrent MRSA? Once these poor suffering people find their way to ID doctors, they’ve usually had multiple episodes occurring over months, sometimes even years. So these recommendations aren’t for the people with a few minor boils, or a couple of recurrences. Assuming that underlying conditions such as hidradenitis suppurativa are excluded, we go for the “try everything” approach, summarized at right. To enforce the effort, we pass out this information sheet. An important caveat is that clinical trials haven’t confirmed the efficacy of these strategies, and hence guidelines do not formally endorse them. Good luck!
How do you manage recurrent MRSA? Once these poor suffering people find their way to ID doctors, they’ve usually had multiple episodes occurring over months, sometimes even years. So these recommendations aren’t for the people with a few minor boils, or a couple of recurrences. Assuming that underlying conditions such as hidradenitis suppurativa are excluded, we go for the “try everything” approach, summarized at right. To enforce the effort, we pass out this information sheet. An important caveat is that clinical trials haven’t confirmed the efficacy of these strategies, and hence guidelines do not formally endorse them. Good luck!- If recurrent zoster is so rare, why is the zoster vaccine recommended for people who have had shingles? It’s true that in immunocompetent hosts, recurrent zoster is rare — you can read more about recurrent zoster (both the real thing and fake-outs) in this post. However, a small fraction of people who get shingles remain at risk for another episode, presumably because the first outbreak did not sufficiently boost their antibody responses, or because their immune system is not intact. Furthermore, as anyone who does clinical practice knows, the motivation for zoster immunization is particularly high for people who have experienced a case themselves! While the full details of the ACIP recommendations for the just-approved zoster subunit vaccine are not yet available, presumably they will also recommend this vaccine for patients with a history of zoster, just as they did for the live virus zoster vaccine. Notably, 92 patients with a history of prior physician-diagnosed zoster received the subunit vaccine in a prospective study, with the primary endpoint being antibody responses; encouragingly, 90% of those immunized had a four-fold increase in their VZV titers.
 In TB screening, do you have a preference for using either an IGRA or a skin test? In general, the IGRA (interferon gamma release assay) is better — less operator dependent, no second visit required, no false positives from BCG. While the IGRA is more expensive, its advantages over tuberculin skin testing were acknowledged in the latest guidelines, which stated that the IGRA is generally preferred when available. See the summary table at right (click on image to see it larger).
In TB screening, do you have a preference for using either an IGRA or a skin test? In general, the IGRA (interferon gamma release assay) is better — less operator dependent, no second visit required, no false positives from BCG. While the IGRA is more expensive, its advantages over tuberculin skin testing were acknowledged in the latest guidelines, which stated that the IGRA is generally preferred when available. See the summary table at right (click on image to see it larger).- I take care of a nurse who got Tdap last year, and was recently exposed to pertussis. Should she get preventive antibiotics? It would be great if we knew the degree of pertussis protection afforded by the Tdap vaccine after a direct exposure, but unfortunately those data are limited; in addition, secondary cases of pertussis have occurred within households even when immunizations are up to date. As such, it’s recommended that most healthcare workers receive antibiotic prophylaxis after exposure to a case, as they may come in close contact with people at high risk of severe illness from pertussis.
- You ID doctors seem pretty smart. Where do you get all this information? Don’t be fooled by our apparent omniscience; it’s an illusion we create to compensate for the fact that we don’t do invasive procedures. Mostly, we just know where to look stuff up.
- What’s made you laugh out loud recently? How about this recent CDC report?
Q: Waiter, what's this bat doing in my salad?
A: Sleeping?https://t.co/RK8aJLFLwK via @CDCgov— Paul Sax (@PaulSaxMD) October 27, 2017
I know, I know — we have a peculiar sense of humor in this field of ours.



Excellent answers as usual. These are questions I get all the time, too! I did want to comment on three:
For cellulitis, some current EHRs allow you to quickly identify antibiotics given in the past and alphabetize them. Conveniently, all cephalosporins start with c, so you can get that med history really fast. I am trying to train our docs to do this. But if the patient’s alleged reaction is not severe, I would use a cephalosporin even if they’ve never had one before. In real-world practice, the risk of doing this is very low (this is published), especially when you compare it to the high adverse event rate with clindamycin (also published) compared to other antibiotics.
For varicella vaccination, they need to have two doses for full immunity. Initially, a single dose was used, so there may be some folks out there who never got their second dose. The exact same principle applies to MMR – if they’ve had two doses, no serology is needed (yet it is often demanded).
Finally, Paul, I think you should not mess with the illusion. We need our nerdy mystique!
Thank you for these great ID Clinical Pearls, Paul. They are always so helpful. What are your thoughts on doxycycline for recurrent MRSA?
P.S. I own a French anti-TB postcard from roughly the same era as the poster(?) shown above. The postcard extols the virtues of sunlight and fresh air for killing the TB “microbe affreux” (awful microbe, as near as I can translate).
Doxycycline would also be a good choice for recurrent MRSA. The dermatologists sometimes use minocycline, but I find it has too many side effects.
Paul
Very informative, thanks
Can you comment on your approach to the indeterminate igra result?
Reasonable to supplement with a tuberculin skin test. As with all things related to TB screening, clinical judgment (likelihood of infection based on epidemiology, likelihood of progression if infected) is important!
Paul
No doxycycline for cellulitis?
Doxycycline has unreliable activity for beta strep, so not a drug of choice. It does have very reliable anti-staph activity, however.
Paul
Dear Dr. Sax,
I greatly enjoy your blog. However, I was confused by the TB table which appeared to show a TST of > 15 mm as unlikely to be TB and a TST of > 5 mm as likely to be TB or did I misread the table. When I was doing university student health, we used to do the IGRA for many of our foreign students. This eliminated the problem with BCG vaccine but also decreased the likelihood of misreading the TST.
This table refers to your clinical suspicion of TB and/or the likelihood of progressing, and the thresholds for skin test interpretation. We use 15 mm for the lowest risk on both these categories, and 5 mm for the highest.
Hope this clears things up!
Paul
Thanks for a really informative post. I have a couple of follow up questions on cellulitis.
– I was always taught that Group A strep was ‘always’ penicillin sensitive (with the caveat that other organisms in the area could produce a beta-lactamase rendering the penicillin Ineffective); is that correct, and are Group C and Group G streptococcus ‘always’ penicillin susceptible as well, or do they have mechanisms for becoming resistant?
– In the UK we generally use flucloxacillin first line for cellulitis. Based on the Norwegian study do you think that just penicillin (oral penicillin V, intravenous benzyl penicillin) should be used first line option for uncomplicated cellulitis, rather that something like cloxacillin that has Staph coverage too?
– I didn’t see mention of macrolides; in the UK these are generally the first choice in penicillin allergic patients with skin infection – I’d be grateful on thoughts?
1) Yes, beta strep spp generally maintain beta lactam sensitivity.
2) Some cellulitis is staph, so I would continue using flucloxacillin (which for some reason isn’t available in USA).
3) Strep resistance to macrolides is widespread in USA.
Paul
I am trying to subscribe to this blog
On the right, see “Subscribe to HIV and ID Observations via Email”, enter your email address, and click “Subscribe”.
Paul
Why are you not a fan of TMP-SMX? Is it because s aureus coverage is not necessary for run-of-the-mill cellulitis? If so, why clinda but not bactrim?
Or do you believe it posseses inferior antistreptococcal activity than the other agents? Again, if so, why clinda but not bactrim?
Or are you turned off by the side effect/adverse event profile? In which case, especially considering the rise of community acquired c diff, why clinda but not bactrim?
I also was puzzled by this.
TMP-SMX is used for skin infections since it has reliable anti-Staph activity. Whether it’s also a strep drug remains a matter of debate.
Paul
When the cellulitis is significant and my host immunocomprismed (I am an HIV specialist), I tend to treat with cephalexin and Bactrim together. Is this reasonable or am I over-treating?
Sir.. What is the role of IGRA in a country like India, where TB is so prevelant?
It is particularly useful in diagnosing latent TB in those with BCG immunization.
Paul
You said to one of the question that the pregnant woman did not need have her varicella titers checked after being vaccinated for chicken pox.
On the other hand, apparently writing in favor of the subunit vaccine, the prospective study you mention checked that very response of titer elevation in responders. I know science is not always straight forward and I’m often made to shut up by my patients who somehow convince me when they don’t want a vaccine.
This vaccine titer response science to PROVE one’s point… is it a different strategy than NOT checking titers in clinic situation… I know it doesn’t prove anything but I’m sure I’d do the same thing confidently and the patient probably won’t have chicken pox during per pregnancy.
Any comment on this?
Thank you.
https://www.ncbi.nlm.nih.gov/m/pubmed/25785967/
I would not use TMP/SMX if the stakes are high (facial or hand cellulitis) but this trial convinced to me to use it in lieu of clinda.
Thanks for citing that study, which is important. However, virtually every study of cellulitis and/or soft tissue infection finds around an 80-85% response rate (including placebo-controlled studies), which makes me think most patients would get better on their own regardless of what antibiotic is selected.
I agree that for severe cellulitis, TMP/SMX is not a good choice.
Paul
I’ve read that staph also hides out in the umbilicus and anus in addition to the nose, what do you think?
Dr. Sax,
Your commentary on the new zoster vaccine is very helpful.
Can you offer any comments on this scenario:
56 y.o. female with selective IgA deficiency. Out of an abundance of caution, has recently been avoiding all live virus vaccines. History of childhood chicken pox, although parents entertainingly recall that she had “only a few pox,” whereas siblings had more typical disease. Episode of herpes zoster at age 55 with “2 small lesions (silver dollar size) appearing simultaneously on abdomen and back, one just to left of belly button and one to left of spine. If one poked a stick through horizontally from front to back, the lesions would line up.” No pain but “maddeningly itchy” for about 10 weeks, with itch persisting long after lesions healed.
Patient has some hesitancy around vaccines. Severe fatigue and distressing neurologic symptoms (weakness, numbness, paresthesias) followed adult vaccinations with Hep B and MMR in her 40s. Also, patient apparently received live polio vaccine as a child (sIgA deficiency status was not known during childhood; nor when she received adult MMR; was discovered around age 50). The history of live polio vaccine administration was of some concern to her neurologist. As mentioned, although aware that only one or two live virus vaccines (BCG, yellow fever) are discouraged in sIgA deficiency, patient has been avoiding all live virus vaccines out of an abundance of caution; hence she opted not to receive the shingles vaccine in the past.
Link to 2012 AAAAI guidance which I found interesting:
http://www.aaaai.org/ask-the-expert/administration-live-viral-vaccine
This patient is asking about the new zoster vaccine. Should she consider it? Is a patient with sIgA deficiency more likely than anyone else to experience recurrent herpes zoster? Thoughts on safety, efficacy of this new zoster vaccine in sIgA deficiency?
Thanks in advance.
Hi,
Can’t comment on a particular case (especially one so complex), but the vaccine has been tested in immunosuppressed patients. Remember, it’s not a live virus vaccine, it’s a subunit vaccine.
Paul