December 8th, 2016
Intracranial Aneurysms for the Non-Neurosurgical Provider: Primer Series, Part 3
Bianca Belcher, MPH, PA-C
In part 3 of this primer series, I will discuss a basic overview of monitoring patients who are not undergoing treatment for intracranial aneurysm as well as potential treatment options for those who are. (See part 1 for a summary of natural history studies and part 2 for information on patient risk factors.)
Many times the decision is made not to intervene because the modifiable and/or non-modifiable factors make the risk of intervention greater than the risk of not intervening. In these cases, we continue to follow the patient with imaging. The type of scan, the intervals of imaging, and duration that we follow patients vary based on several factors such as the patient’s age and the size, morphology, and progression of the aneurysm. If monitoring is the appropriate course and if the first image was of good quality, then we will typically see the patient in clinic in 6 months with an MRA or CTA. If an MRA will provide the quality that we need, it is the preferred method of following a patient because there is no radiation. If nothing has changed with the patient’s risk factors and imaging also remains unchanged, we push the next clinic appointment and imaging to one year, then see the patient again in two years. If we observe a change in the aneurysm, we are very likely to offer treatment.
If treatment is the appropriate next step, there are essentially two paths that we discuss with patients: open surgical clipping and endovascular treatment. From the patient’s perspective, there are advantages and disadvantages to both. Within the endovascular path of treatment there are several choices, described below.
Open Surgery: Craniotomy for Clipping
General Advantages:
- With a well-placed clip, the aneurysm is cured.
- Less follow-up imaging is required as compared to endovascular treatment (our team does a postoperative diagnostic angiogram while the patient is still in house to ensure that blood flow to the aneurysm has been cut off and then a follow up CTA in 1-2 years).
General Disadvantages:
- Longer recovery for the patient as compared to endovascular treatment
- Incision line scar (note: the scar is usually hidden in the hairline)
- A bad haircut – This is surgeon specific. Most commonly a small strip of hair is shaved along the incision line, but it could range from no shave to a large strip.
- Mild discomfort postoperatively with facial swelling and when chewing (the temporal muscle is cut in order to gain craniotomy access – most often the temporal muscle heals, but is tender for the first few weeks after surgery)
- Not appropriate for all aneurysms
Endovascular Treatment Options:
General advantages
- Faster recovery time — Generally our patients are discharged on postoperative day 2.
- No large incision
- Minimal postoperative pain
General disadvantages
- Requires more postoperative imaging as compared to clipping – most patients are followed for at least 2 years because if recanalization of the aneurysm occurs, it generally happens in the first 2 years. Imaging occurs at the following intervals post procedure: 6 months, 1 year, and 2 years.
- Not appropriate for all aneurysms
Coiling (+/- Stenting)
Specific Advantages:
- The oldest and probably most common method of endovascular treatment of aneurysms
Specific Disadvantages:
- Not ideal for treating wide-neck aneurysm without additional equipment — If an aneurysm has a wide neck, a stent must be used in addition to the coils. The stent requires the patient to be on dual antiplatelet therapy 5 days prior to the procedure at our institution and approximately 6 weeks postprocedure. This can be problematic for patients already on anticoagulation for cardiac or DVT reasons. Triple agents increase the risk of gastrointestinal bleeding significantly and we try to avoid it in our patients.
- Permanent mass effect — If a patient presents to clinic with cranial nerve symptoms secondary to a large aneurysm pressing on the nerve, adding coils will secure the aneurysm, but it will also likely worsen the nerve deficit.
- Not ideal for treating oddly shaped aneurysm because it is difficult to get the coils in all dimensions
Liquid Embolic Agents
Specific Advantages:
- Due to their fluidity, liquid embolic agents such as Onyx or n-BCA are a good option for oddly shaped aneurysm that may be otherwise difficult technically to coil.
Specific Disadvantages:
- Similar to coiling, liquid embolic causes permanent mass effect.
- Generally not the first choice to treat uncomplicated aneurysm
Pipeline Flow Diversion Stent
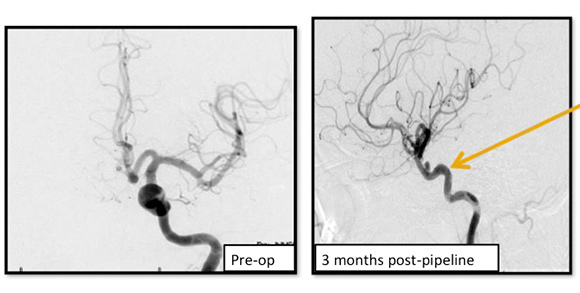
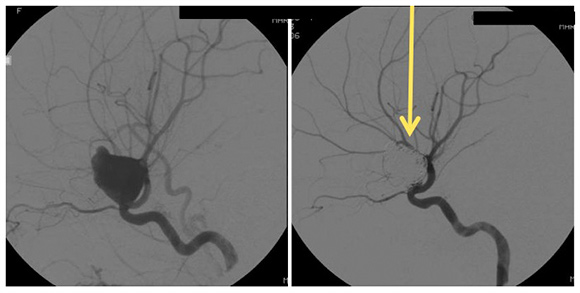
Image shows the remodeling of parent ICA vessel before and after pipeline placement. Arrow points to where the aneurysm used to be.
A braided cylindrical mesh stent designed to divert flow to blind pouches.
Specific Advantages:
- Unlike coiling and liquid embolic agents, the pipeline flow diversion stent is laid across the neck of the aneurysm and does not require intra-aneurysm catheter work.
- Also, unlike the two previous options, the pipeline flow diversion stent causes stagnation of blood within the aneurysm, causing it to shrink, scar down, and remodel the vessel around the stent. This removes the issue of mass effect.
Specific Disadvantages:
- Pipeline also requires patients to be on dual antiplatelet therapy — clopidogrel (Plavix) 75 mg and aspirin 325 mg — for 5 days prior to the procedure and 6 months postprocedure. This makes it a difficult treatment choice for patients with ruptured aneurysms and those already on anticoagulants, as mentioned above.
WEB (in clinical trial)
The WEB is a globular intrasaccular device made of nitinol mesh that combines theory behind coiling and pipeline flow diversion.
Specific Advantages:
- Faster than coiling because it is a single deployment
- Does not require dual antiplatelet therapy as per the group running the trial (the Sequent)
- Due to the unique design that combines flow diversion, it can be used with aneurysms that may be oddly shaped (which, as mentioned above, was a disadvantage of coiling alone).
Specific Disadvantages:
- Not FDA approved, nor is it available in the U.S market except under clinical trial guidelines (the WEB has been available in Europe for 6 years)
- Permanent mass effect
Conclusion
If a patient needs aneurysm treatment, he or she has several options, though not every type of treatment is an option for every patient. Patient factors such as age and comorbidities and aneurysm factors such as size, location, and morphology may limit options. It is worth mentioning that when referring patients for aneurysm treatment, you should consider sending them to: 1) a neurosurgeon trained in both open and endovascular techniques, or: 2) two providers – a neurosurgeon traditionally trained in only open techniques and a second provider trained in endovascular techniques. This ensures that your patient has options. Some aneurysms could be treated with relatively low risk in either an open or endovascular fashion, but if they only see a provider that does one but not both, you may be limiting your patient’s options without realizing it.
A special thank you to my team for some of the images utilized in this posting: Dr. Ali Aziz-Sultan, Chief of Vascular and Endovascular Neurosurgery – Brigham & Women’s Hospital, Dr. Nirav Patel, Cerebrovascular & Skull-Base Neurosurgeon – Brigham & Women’s Hospital
Disclosure: I was a sub-investigator under Dr. Ali Aziz-Sultan at Brigham & Women’s Hospital on Sequent Medical’s WEB trial. The trial has concluded and I did not/will not receive any personal compensation for the clinical trial.




Perfect
NICE summary. Sweet and to the point.
Appreciate the feedback. Thanks for reading!
Best, Bianca
Ms. Bianca, you’ve done a wonderful job for any family practitioner to get clear, concise information quickly! It’s so easy to read and understand I’m going to recommend your articles to many others not in the medical field.
Job well done!
I hope your next set of articles will be on guiding the primary care physician in acquiring help from the various types of therapies for the SAH pt. SAH survivors are rare and once out of hospital and back home, perhaps to more rural areas, seems like PCPs just don’t have the knowledge to get the pt the help needed, and there’s all the restrictions the pt is under. Not in anyway saying the PCP is not good, just that with no experience, there’s a lot of caution and in the end, seems like pts who aren’t in big cities with medical universities fall through the cracks in getting assistance from OT, PT, Speech…
Elaine,
Thank you for the wonderful feedback and suggestion for future article. I will surely add post-SAH patient care for PCPs to my topic list. Thank you again.
Best,
Bianca