An ongoing dialogue on HIV/AIDS, infectious diseases,
April 30th, 2016
A Ridiculously Long Post: How EHRs Expose Unspoken Hierarchies Within Medicine — Or Maybe Are Just Bad
 I am consulted by a surgeon about a patient with something that might be infectious, might not. A very appropriate referral.
I am consulted by a surgeon about a patient with something that might be infectious, might not. A very appropriate referral.
After seeing the patient and reviewing the history and scans, I decide a CT-guided biopsy is the next step.
The nice radiology fellow tells me “Just place the order in [enter name of EHR here]”. Since this is the first time I’m ordering this test using our new system, the prospect of doing so doesn’t exactly fill me with joy.
Nonetheless, I give it a go. I place the word “biopsy” in the dreaded order search box, hit enter, and cover my eyes, at least metaphorically.
A lengthy list appears, and I select the test closest to the one desired — for some reason it’s called “CT IR MASS ASPIRATION/BIOPSY (NO CATHETER) (Order #152640784)”. The order then requires filling out numerous fields (some of them woefully tiny for anyone past the age of, ahem, failing eye accommodation), clicking several check boxes, and deciphering inscrutable warning messages.
Since the precise diagnosis on this case isn’t yet known, and a precise description of the problem doesn’t come up in the formatted search, I do what everyone does when trying to navigate these complex screens and their finicky criteria.
I fudge it (in other words, make something up). Nevermind that the fudge doesn’t really fit the case — voila, it goes through!
But most importantly, the order for the biopsy includes a free-text box, where I enter the critical micro tests desired, specifically:
- routine and anaerobic culture with gram stain
- fungal culture and smear
- AFB culture and smear
- Nocardia culture and modified acid-fast smear
Note to micro lab: Prioritize pathology and fungal culture/smear if there isn’t enough specimen.
(If that seems overly detailed, trust me — I’ve been doing this ID stuff a long time. You’ve got to give precise directions. Sometimes you might even need to go from being the ID Attending to, as my brilliantly funny colleague Libby Hohmann once put it, the “Transport Attending”. That happens when you both specify the cultures to be done and are the person making sure the specimens arrive at the lab appropriately.)
After completing the order without setting the computer aflame, I feel a little glow of satisfaction — kind of like when you get a tough clue in a crossword puzzle, correctly guess your opponent’s hand in poker, or predict in advance when the runner on first tries to steal second on a 2-1 count.
Or maybe that glow is simply the computer screen reflecting off my face? Because the satisfaction is short-lived — soon after placing the order, I receive this from the radiology fellow:
Dr. Sax, thanks for your biopsy request. In addition to the order, we require you to put in separate orders for each microbiology test before the biopsy. Could you please place these individual orders- i.e. fluid culture, AFB, fungal culture, nocardia, etc and any other micro testing you think would be relevant? These will need to be entered as “Signed and Held” orders.
Brilliant.
Thoughts, emotions, reflections on this unfortunate turn of affairs.
- Why does this make me feel so worried — and frustrated? I envision entering these individual orders as a sure-fire way of heading down a bunch of digital rabbit holes, especially since some of the orders aren’t exactly common. What are the chances that the stain for nocardia would be straightforward? The frustration is amplified of course, by the fact that I already have written exactly what is wanted in the free text box. (That will be the first — but not last — time I mention this.)
- Why do I have to write these extra orders? No doubt for some billing and/or compliance reason, something completely separate from the patient care activity. Even though the desired tests are already clearly entered in the computer (second time mentioned), if they aren’t entered in exactly the right way, in exactly the right place — and by correctly, I mean “according to the rules of this particular EHR to meet whatever criteria are set up by whatever payer” — then they can’t be done because they won’t be paid for. Joy. Note that in our last EHR (we’re on our fourth), this free text order would have been fine.
- Why doesn’t someone more expert with the EHR take what I’ve written and enter the orders? Yes, this is passing the buck, but what we want is clearly spelled out in the free text box. (Third time.) It’s highly likely that someone on this care team has the expertise with this EHR to transcribe what I wrote into compliant EHR-ese. Maybe a “Super User”? Maybe a person whose sole job is to make sure orders are compliant with the above regulations? I hereby authorize him/her to make this happen.
- Why does this feel so burdensome compared to writing orders the old way? We doctors don’t mind writing orders when the process is straightforward — hey, look at my “free text” order for the micro tests cited above. (Fourth time.) Piece of cake. I have written orders like this hundreds of times, or alternatively written this exact list in hundreds of consult notes that are then transcribed into orders by others (interns, residents, PAs, NPs). But the process of writing orders has changed — it’s become tremendously nonintuitive — and even worse, it differs dramatically between platforms. You know how good electronic calendars can take your free text that says, “Dinner next Tuesday 7pm with Consuela at El Conejo Guapo restaurant”, and bingo, the dream date at The Handsome Rabbit is entered correctly? Wouldn’t that be a nice EHR feature? Dream on.
Perhaps the most important question hasn’t even been mentioned yet, and it’s this:
Why does it bother me so much?
I know, I know. In the time I spent writing this absurdly long anecdote, I could just suck it up, enter the orders, and get on with life — a bit frustrated, yes, but ready to move on to the next challenges, such as learning how to spell (and pronounce) “Aedes albopictus” and what PCSK9 actually stands for.
But first, some additional musing on this last question — why it’s so annoying — have yielded 3 key answers:
- Concern that the right tests won’t be done despite all the effort. This is the most important issue, after all — we’re all trying to help our patients. Wouldn’t it be terrible if the critical microbiology tests were omitted based on a cumbersome physician order entry system? Even after I clearly wrote the tests in the initial order? (Fifth time.) Or taken to the extreme level (why not, I’ve written this much ) — what if some critical intervention isn’t done because the order isn’t written correctly in the computer. Imagine those CPR scenes from the TV show ER if, instead of verbal orders, George Clooney had to fire up his laptop, put on his reading glasses, and start typing.
- A fear of the endless time sink. What if some of the tests don’t show up in the initial search? What if there’s an option for separate “nocardia culture”, “nocardia stain,” and “nocardia culture and stain” — do I choose the first, second, or third one, or all three? What if they ask if it’s “lab collect” or “clinic collect”, since it’s neither? How does a “Sign and Hold” order (as specified by the radiology fellow — who emphatically is blameless in this) differ from a regular signed order? I see the edge of that rabbit hole, drawing closer …
- The process elicited an uncomfortable reinforcement of the weird hierarchies in medicine. Any chance that this patient’s surgeon is dealing with the same challenges? I asked him, and he knows the EHR can be difficult, but he told me he barely ever interacts with it — he’s got a veritable army of scribes, PAs, residents, and other support staff who enter the information for him, support staff he can justify financially based on how hospitals are paid these days. Hearing he’s exempt from these frustrations elicited the same feeling I get watching the First Class flyers board the flight early. For the vast array of doctors (and essentially 100% of nurses and PAs, let the record show), no such luck. A giant chunk of EHR-generated clerical work has been handed to us in the form of mouse clicks, drop-down menus, and (too small) text fields. And it just feels lousy.
You might be wondering, after this long screed, what I ended up doing with these orders. Someone has to enter them eventually, right?
Guess.
https://youtu.be/rK1iPNeLTAo
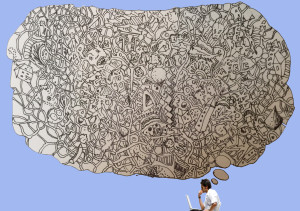
(Picture credit: Anne Sax)


Bravo for an excellent critique. The battle you describe is endemic (or epidemic?).
The next step in your saga occurs when you try to select a billing code for your consult. “Evaluation of unknown but possibly infectious lesion right side of abdomen, initial visit.” Good luck! We have been pushed to making things up to satisfy the innards of the EHR. Of course, the bean-counters who ultimately analyze these inputs will take them as gospel and proceed to generate reports on our performance.
Paul –
I only have one thing to say. Well 2. Make it 3:
1. Can I get an “Amen”?
2. That Libby Hohmann story is one of the best of all time. You should retell it here. Maybe even ask her to reenact it and make a video and post it on some social media platform. Vine, or snap peas, or faceplace, or chirp or whatever they’re called. Kids.
3. We’ve had the same EMR you have for a few more years. You know the saying “It gets better”? You do? Not applicable here.
In solidarity.
I’m honored to get a mention and could not agree more — EHRs push all the work up to the top and makes us robotic data entry clerks. My further thoughts on this same EHR are not printable! Had a humorous interlude with an ophthalmologist this week. As I saw him writing in that mysterious optho code they have, and actually drawing little pictures of my fundi — i.e. WRITING in a medical record …… Me: “Wow, you can still write, you lucky guy!” Ophtho: “Yeah! Not sure how much longer. Those EHRs are crap. I was in engineering at MIT before this and I can’t believe the terrible designs/set ups. I’m fighting as hard as I can to keep our records like this.” We then went on to discuss recertification/MOC — you can imagine where that went! Libby Hohmann
Paul—
Thank you for your excellent example of a human-machine interface that produces inefficiency in its (failed) effort to increase effectiveness.
Each ‘pod’ of experts in the EHR designing process does not know what the other parts need. EHR/IT designers focus on ‘requirements studies’ which specify inputs and outputs. Due to deficiencies in our education and funding/profit priorities, the internal workings –throughput– has less priory.
Throughput-focused EHR designers would recognize that your ‘write-in’ could be interpreted efficiently by — as you said — subject matter experts (SMEs), until an artificial intelligence (AI) ‘smart system’ can be developed that reliably and validly detects proper tests and priorities from text. The designers are not focused on reducing physician time in their system, probably because their design team is focused on conserving their own time resources.
EHR is not the focus of my work but, as a cognitive-social psychologist/epidemiologist medical educator with an undergraduate in human factors engineering, I have sometimes tried to make suggestions to EHR design teams. They have asked me to solve specific medical knowledge problems, but fail to see the broader implications of how users (physicians) interface with their machine in their ‘rush to finish’ projects.
EHR redesign teams need medically-trained human factors specialists who can ‘walk them through’ throughput experiences such as the one you described.
What you describe could easily be addressed by a socio-technical approach to software design. Madhu Reddy has published extensively in this area.
Amen Paul. I’d write more but the EMR already has stolen too much of my time.
Well now I REALLY know what CPOE means! ‘Cumbersome Physician Order Entry’! Brilliant!
Totally agree Dr Sax. The main problem is that the “brains” that put all these EHR on work (not just designers, but hospital managers) do not see patients. Moreover, they do not think about patients, they just think in incomes.
Brilliant post! As always!
EMR is a disaster.
It is less efficient and less proficient.
I estimate that it takes me 10 to 20x as long to do routine tasks at it used to with paper charts. I recently helped cover a colleague’s office who is still on paper charts while he was out getting shoulder surgery. Finishing up paperwork at the end of a day took about 10 minutes or so. At my own EMR using office, it takes 2 to 3 hours.
Critical information is HIDDEN from view, like the number of times a day a patient takes a pill, or the complete instruction. When prescribing medications the allergy list is not visible on the same screen. When ordering labs one cannot simultaneously review what has already been ordered.
I will be taking an early semi-retirement, cutting back to 2 days a week because of the outrageous amount of time it takes at home to push electrons to get caught up with office work and to try to get it right despite the obstacles.
I had the great luck of designing my own EHR, about 13 years ago. It handles 700,000 urgent care patients a year, and 300,00 procedure and primary care practice patients a year. Because I was both user and designer, the moment an issue came up, I fixed it. I can only base my success on the comments of the users, but they are greatly pleased. I do use automation where possible to fill in checkboxes and drop-downs when I can. Interfaces are integrated so you can look at old and new x-rays, next to lab results on the same screen. It was only by listening to the staff that we developed such a system. I am truly sorry for the experiences you are having but I think part of it is because of the result of having non-physicians lead the development. Also, the driving force behind such systems is to get the next version out ASAP (and thus charge for the upgrade). Also, the turn around time for bug fixes and add-ons is significant, where I could do the same, sometimes in hours. Having your OWN IT department do the development may be the only practical solution. Major EMR companies should design modules that provide given functionality. But local IT in hospitals should do the assembly work. IMHO
You know what M.D. and D.O. mean —
M.D. = Medical Documenter
D.O. = Documenter of Osteopathy
It’s a brave new world!
Dr Sax,
Great insights that speak to what all of us find. Regarding the hierarchy, you’re right that the surgeon doesn’t use the EHR to that level or detail, but what level of responsibility does he take when the lackeys mess up the order entry, or the lab transport, or the processing? Some surgeons might, but many would blame said lackey. That’s why we do it ourselves, because we know that it will be mishandled if we don’t, and because we care about getting it right, frustrated as we get.
Paul, you have expressed so many of my frustrations, I won’t reiterate them here. Suffice it to say that while EHRs have some good points, by and large they are dreadful. And I mean “dreadful” in the full sense of the word. We need EHRs designed by and for the people who actually work with them day-in and day-out. Us. This topic is so depressing, I think I will go watch ZDoggMD’s “EHR State of Mind”. http://zdoggmd.com/ehr-state-of-mind/ (Thanks for turning me on to ZDoggMD, by the way. I show a couple of his videos in my classes.)
“Imagine those CPR scenes from the TV show ER if, instead of verbal orders, George Clooney had to fire up his laptop, put on his reading glasses, and start typing.”
A few years back I was on a unit and a patient appeared to be having a seizure. The resident tells the nurse “I need 1 mg of Ativan, STAT.” To which, the nurse replied “Doctor, you have to place the order in the computer first.”
EHR mentality is not only cumbersome and annoying, it’s going to kill someone.
I have used an EMR for 15 years but just helped convert the practice to one of the well-known massive EMRs associated with a large hospital system. An EMR should do work for the clinician, making their documentation clearer, better organized and readily available. Instead, the modern massive EMR seems to be designed so the physician is working for the EMR. They are badly designed with no understanding of clinical practice or physician patterns of thinking or clinical process. All of the major EMRs need to be rethought and rewritten. They program developers clearly have no concept of how providers give care.
Paul,
Could not have said it better. Most
EMR’s are what Nancy Pelosi said of the Accountable Care Act, ie we have to pass it to see what is in it.
A succinct description of a bowel movement.
The problem of EMR’s is not only technical but logical. A fixed set of instructions can not equal the function of the human brain. For those with neurocognitive bend, the interaction of computer and man in the case of EMR’s is just plain nuts.
The information overload problem is massive. The cognitive dissociation problem boggles any mind.
Yet EMR’s proceed to be introduced, with the obvious expectation that the human interacting with the computer will do the compensating for the major flaws in design and execution.
This will only change with a major movement. Not sure when that will happen but will be happy for the revolution in clinical medicine to happen
Agreed.
Followers of this blog might be interested in reading Nicholas Carr’s book, “The Shallows: What the internet is doing to our brains.” He argues persuasively that the structure of the software we use (including EHR software) conditions our brains to follow certain pathways of reasoning. We are being unconsciously conditioned to think “inside the box” rather than to think critically.
Bad.
Maybe we can start it here!
I just refuse to use the EHR in my Institution and continue doing the traditional hand-written-in-paper medical notes as many of my colleagues do. The problem is if we are not all in the same page we have a fragmented clinical chart (that e have with the EHR anyways). We no longer have a linear history of our patients, but a disjointed collection of medical orders, tick-boxes, lists and some free texts here and there. The understanding of the history of patients (and our capacity to integrate diagnosis with this material) suffers enormously.
Lets all refuse to use these, Viva la revolución!
In Sax we trust! Great post.
AMEN! Doctors should be free to work as efficiently as possible and entering orders in a user unfriendly EMR is a huge waste of doctors’ time which could be better used spending time with patients.
Why don’t we simply dispell all the IT and behavioral babble and admit that the major and almost only reason for the existence of the EHR is to serve as a billing and upcoding mechanism. If not then why are we not seeing serious peer reviewed publications showing that the EHR actually improves patient care?
Dr Sax somewhat humorously describes the “benefits” of another “improvement” in the practice of medicine. EMRs, like ICD 10, add nothing to the quality of patient care and only burden the practitioners. Among others, they are major reasons why I and many other physicians, sorry to say, have made an exodus from the practice of medicine. Automated in the important ways, but no EMR for me, and with the mandate for ICD 10, I exited.
What are you doing instead? I want to exit too!
Note: I have not seen a single comment in support of EMR/EHR.
When is someone with authority going to accept this is a disaster and expedite transition to a reasonable alternative approach?
The alternative disposition is the aging Luddites are merely going to be supplanted by naive neophytes transfixed by glowing screens. The collective memory of an efficient approach will gradually retire and be replaced by the mediocritocracy..
I’ll take a contrarian approach: Overall, I think the EHR is a good thing. Or at least, it can be. We have ready access to data any time, almost anywhere. We essentially never have to see a patient without the information available in their record, and we don’t spend time trying to track down missing charts (and “films.”) Order sets and reminders encourage the use of best practices, instead of relying on memory. It has enabled us to do much more useful antimicrobial stewardship than before. Communication among clinicians (and even between hospitals) is greatly facilitated. I no longer have to photocopy my inpatient notes so that I will remember what happened in the hospital when I see the patient in clinic three weeks later, because I can see the entire inpatient chart in clinic. The chart is even searchable.
So what’s the problem? The current generation of EHRs mostly stink. They are fantastic buckets of information with mostly poor user interfaces. The data are displayed in a suboptimal manner, decision support is lacking, and far too much time is spent navigating and “satisfying” the system when putting data in. Note bloat, cut-and-paste, and other problems have converted notes from illegible and incomplete to legible, comprehensive, gigantic, and often devoid of clinical meaning or utility. Finally, because they are at their heart billing systems, the unit of information is the visit – good for billing but perhaps not the optimal way to follow complex patients over time.
Imagine what your EHR would look like if Steve Jobs had designed it. It’s got a long way to go. As frustrating as it can be, I do not want to go back to the paper chart, and I am hopeful that some day, the EHR will realize its potential to improve care. I am less hopeful that this will occur during my career.
Hi Jon,
Many good points there. I agree there are many things about EHR that are better — as a data retrieval tool, it’s vastly superior to paper charts. But that was the case with our hospital’s first EHR, which was implemented in 1986! There’s been some progress since then (radiology images, in particular), but a whole lot of regression (and pain) as well.
Paul
Hi Paul,
I am a big fan of you and your blogs. I agree that EMR can be very time consuming but EMR has definitely made life of ID physicians easy. I don’t have to go through tons of pages to find hidden micro result and another pile to look for sensitivity! I can clink and get report of all medications that patient has received (or not received). As with technology, you have to make it better by using it. Even my very old partners now love it (they almost threaten to leave when they heard new EMR is coming to our place). Most of the EMR has order sets. You spend time making them once (or copying from colleagues and modifying) and then checking what you want to order every time rather than doing it individually. It does eliminate the factor-Oh I forgot to order that test!!
Since March 2015 I had been using the same EHR as Paul’s. Note the “had”. Partially as a result of that experience I decided at age 72 to call it quits on direct clinical care. Some egregious problems:
1. “You have two choices. Document incorrectly or not at all.” This was the response of the IT team when, at the beginning of the 2015-2016 flu immunization season, the dropdown menu for flu shot did not include preservative-free quad inactivated vaccine — which happened to be the very vaccine in use throughout the system which the EHR served. My solution: On a yellow note pad enter all the shots I’d administered and then, when the correct vaccine finally made it to the menu, retroactively enter it for all the immunized patients. And hope no one administered a second vaccine in the meantime.
2. Initially, asymptomatic HIV infection did not appear on ICD10 dropdown menu. Solution: Pull out iPhone and ask Siri. Voila: Z21. Try it!
3. Current problem: About ten patients at our hospital have had QNS blood draws for HIV viral load testing. Why? Our lavender top tubes are tiny, so four tubes are needed. At other hospitals in our system, larger tubes are used, so phlebotomists at all sites are instructed to draw one tube. Our pathologists are tearing out their hair (which luckily they can afford better than can I), because so far no way has been found to customize blood draws. We try to give special instructions, which are not always heeded. And patients continue to be called back for re-draws.
4. From my wife, a nurse at my hospital: How does a nurse find STAT orders? By entering about 15 keystrokes and then trying to perceive which orders are faintly highlighted in color on a screen with miniscule print and myriad lines.
As pointed out by Wachter in “The Digital Doctor”, the idea of a uniform and readily available medical record is great. But from the point of view of safety, avoidance of errors, work flow, logical thinking — the current systems stink. But what can you expect for $1.2 billion, the cost of our hospital system’s program? Without divulging the name of our system, permit me to share my mnemonic: Expensive Program for Inferior Care.
Now we doctors do not work for ourselves or patients ,……….! rather we work for insurance companies and to prevent law suits.
We only do lengthy documentation, without any sense and do stuff insurance companies want us to do. There is no room for our individual thoughts.
I feel sorry that medical profession is hacked by the money making making insurance companies.
A patient was recently discharged from the hospital to my home health agency. The physician discharge summary, dictated via EHR, was incomprehensible. It mad no sense whatsoever; no punctuation, same word repeated multiple times, etc. example: “treated for staff lock aria with tropical oink mint”. We get these from time to time and I often wonder how they’d hold up in court. I’m still not sure what happened to my poor patient’s aria.
Amen. Bravo!!!
Why couldn’t the primary team enter the orders? You were the consultant, no?
I was recently completing a physical exam section on a new EMR. I was shocked to find text boxes for me to enter exam findings on:
-“hematological system”
-“endocrinological system”
-“urinary system”
Surely- no physician was involved with designing this absurd form. Either that, or i missed class that day in med school when they discussed the “hematologic system” exam.
Excellent blog post and I heartily concur. EHR is one of the main reasons I left inpatient care after 30 years. I found I no longer interacted with either the patients or the doctors: all the RNs did was input data. Contrary to promises, EHR did NOT save time and did not reduce duplication of entries. The RN mentioned above who would not give the Ativan 1mg IVP stat because the order wasn’t in the computer was out of line; verbal orders are allowed in emergency situations. But I take the doctor’s point and agree. I am thankful I never had to record a code in an EHR. I cannot imagine the difficulty such a complex situation would engender. I also did some chart auditing for med-mal attorneys in my time. Paper charts and handwriting issues were problematic, to be sure, but they paled in comparison to the mess of a printed out EHR. Clearly something must be done, but what? And how?
Until recently the UK NHS has been largely spared the torture of billing-oriented EHR systems.
You may appreciate this article regarding the deployment of such a system at a major research hospital last year.
http://www.computing.co.uk/ctg/news/2427100/addenbrookes-hospital-gbp200m-it-system-proves-an-epic-fail
Wow–that looks like a mess. But I have to say it’s ALL a mess. The hospitals want accurate documentation (as do clinicians) and I do think that IT wants that too. The three groups don’t seem to understand one another, and it doesn’t help that they all have different priorities. Admin wants low costs and complete records. Clinicians want speed, convenience and complete records that include ad hoc incidents (which happen daily). IT wants smooth operations, adequate bandwidth and storage and standardization of data. Not all of these are compatible. (and all or any of them may want other stuff; I am not an expert on any of it!).