An ongoing dialogue on HIV/AIDS, infectious diseases,
December 8th, 2023
Clinician-to-Clinician Advice Is Great for Everyone but Still Horribly Undervalued
 One of the best things about being an ID doctor is that you get to interact with all the medical and surgical specialties. This is one of the most common answers to the question, “Why did you choose to specialize in ID?” and it certainly resonates with me.
One of the best things about being an ID doctor is that you get to interact with all the medical and surgical specialties. This is one of the most common answers to the question, “Why did you choose to specialize in ID?” and it certainly resonates with me.
As a result, we’re frequently in the position of providing clinician-to-clinician advice — which, when done without seeing the patient, was historically called a “curbside” consult. Informally asked, often prefaced with “Can I ask you a quick question,?” these curbsides have pros and cons that I’ve written about on this site numerous times.
It’s a topic near and dear to my heart, so much so that I have an entire talk on this subject that starts with several slides outlining both the benefits and the risks of this practice. And for the hard-liners (see photo above on the right) who never do clinician-to-clinician advice without seeing the patient, trust me there are benefits, some of which I’ve summarized on this slide from my talk:
In a similar theme, around 10 years ago, our hospital system started offering “eConsults,” adapting similar programs from elsewhere. Instead of referring a patient for in-person consultation to a specialist, clinicians could place an order in the medical record, and a specialist would review the question, the data from the patient’s chart, and write a note.
This form of consultation occupies an intermediate place between actually seeing, interviewing, and examining a patient, and the informal “curbside” consults where you give just general advice, undocumented anywhere. Completing the note is expected within 24 hours. Because eConsults are asynchronous, meaning we specialists don’t need to respond immediately, they are far less disruptive than getting paged or called directly.
A huge advantage of this approach over curbsides is that we can review the primary data. In addition, the consulting clinician now has specific advice documented in the chart on how to proceed, which may include ordering additional tests or modifying treatment. In a small proportion of eConsults, we advise that the clinical scenario is too complex to resolve without a formal visit. After all, we can’t put a limit on the complexity of the case — that’s at the discretion of the consulting clinician. When that happens, fortunately, we’ve still been able to weigh in on tests to order ahead of time that will make an in-person visit with us or another specialist more valuable.
How has the program done?
To say eConsults have caught on vastly understates it — they are a huge hit. Imagine if a miraculous Beatles reunion became the opening act for Taylor Swift. To quote one primary care doctor who previously had a solo practice, “It’s by far the best thing about working here.”
You can easily see why they’re so popular. Not only do clinicians get access to nearly the full range of medical and surgical expertise at our academic medical center, often an eConsult can spare their patients the inconvenience and cost of an extra doctor visit. Indeed, published data on our program strongly show that eConsults decrease the volume of formal referrals, while increasing their appropriateness. Evaluations from different centers (here and here) had similar findings. Implied in these data is that care efficiency improves and the total cost to the healthcare system declines (fewer visits = lower costs).
Sounds like these eConsults are a real advance, for patients, clinicians, and payers, a rare win-win-win trifecta — so much so that we proposed expanding the eConsult service to inpatients to deal with the never-ending deluge of curbsides that arise in hospitalized patients.
So far, all sunshine and warm tropical breezes. So, what’s the problem?
No one has figured out how to pay for these things.
In a healthcare system where procedures dominate the payment landscape — the more, the better! — an advance in efficient patient care just can’t get the attention of the payers or the administrators holding the purse strings. Yes, there are billing codes for clinician advice activities without seeing the patient, but the net pay is poor (average 0.5-1 RVU, latest conversion factor $33.06/RVU), and the technical hurdles of getting reimbursement can be tricky to implement. Plus there’s this requirement:
THESE REQUIRE INFORMED PATIENT CONSENT! Since the consulting physician is not seeing the patient, the requesting physician must obtain and document informed consent.
And guess what? If you or another ID doctor ends up having to see the patient and do a consult on the case within a week, that “formal” consult can’t be billed! As a result, hardly anyone uses these codes, at least based on my emailing a variety of ID doctors in academic medical centers, and by the lukewarm responses to an online query.
So if we’re not billing insurance, how do eConsults get supported? Note I’ve used the common euphemism for money — support.
Here, our hospital system pays us for eConsults out of the Physicians’ Organization budget, a finite resource; they set the reimbursement at $50/eConsult when we started, an amount that hasn’t budged despite a substantial increase in the cost of living over the last decade. In addition, they declined our offer to expand eConsults for inpatients, even though we offered to expedite these to make discharges more efficient.
I queried a bunch of other ID doctors in a variety of practice settings about their payment models, and their responses were diverse (and fascinating). Some get paid a set amount, like our program. One does use the “interprofessional consults code” and makes do (unhappily) with the meager payments. Another uses these codes, but augments them to what seem to me to be much more reasonable rates:
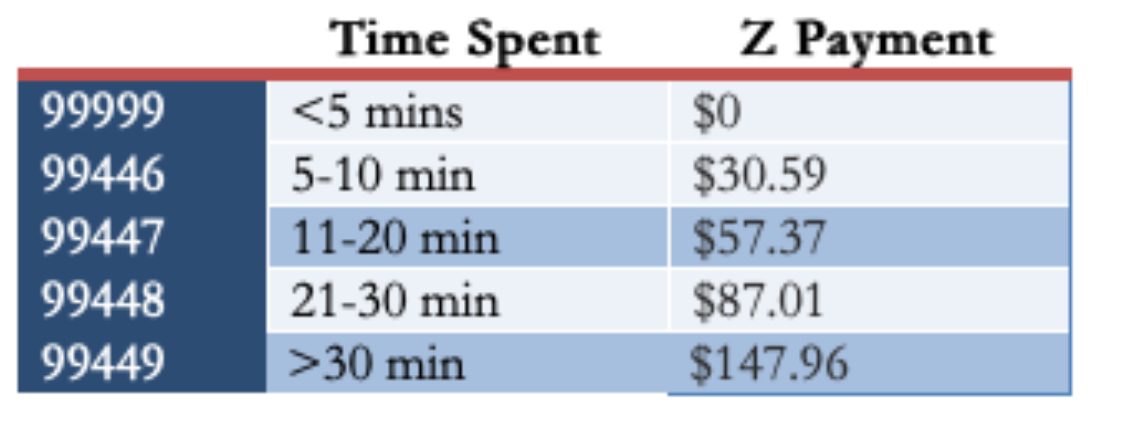
(For the record, in my experience, most eConsults would be in the third or fourth category, occasionally fifth if they involve contacting the consulting clinician or a reference laboratory.)
The ID director at a “closed” healthcare system says they have no specific payment for eConsults, but that they are tied directly to the ID doctor’s job responsibility. He estimated that “all clinician-to-clinician advice for the on-call ID doctor, without direct patient contact, accounts for 3–5 hours/day” — a substantial time commitment! Finally, Dr. Allison Nazinitzky, who does ID locums work, shared with me that one of her telehealth contracts pays her $125 for an “interprofessional consult with note — a flat fee no matter how long.”
(Check out my interview with Dr. Nazinitzky. Her experience finding the true value of ID clinical care is dynamite.)
The medicolegal aspects of eConsults should be factored into any estimation of the value of the program. eConsults may reduce medicolegal risk for the referring clinician, but they substantially increase it for the specialist taking it on. Why? As noted in an excellent review of the legal risks of curbside consults, this is because we are now explicitly reviewing the patient’s chart and providing specific advice:
The closer a physician gets to providing very specific information—what dose to start with, when to draw labs and what other kinds of studies to get, and what to do specifically with a particular patient—the closer that physician is coming to being part of the care team, as opposed to just providing general information.
Despite the boilerplate language we insert at the end of each note indicating the limitations of eConsults, this will serve as little protection if a suit is filed. As part of the care team, our names can be included in any filed suit. And even if we are later dropped because we never saw the patient, the process itself can be long and painful.
So what’s the solution? I say include these advice services as part of what constitutes the job of a clinical ID doctor — give us appropriate RVU or full-time equivalent (FTE) credit for it — and make it commensurate with the time, value, and medicolegal risk associated with the service.
And if that doesn’t happen, let’s do what Dr. Andrew Pavia recommends, in my response to the query about whether he uses the interprofessional consults codes:
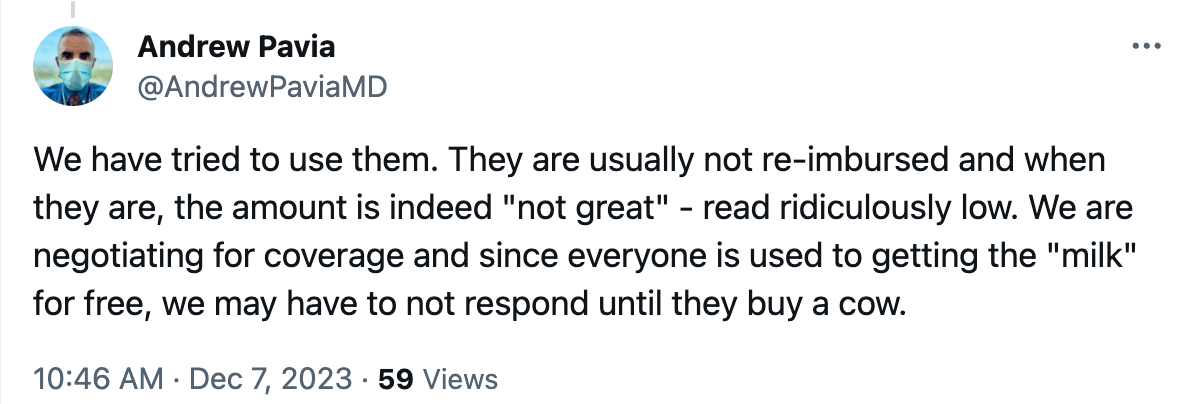
In other words, stop doing eConsults until they’re properly supported. Seems like a good plan!


I don’t think the current healthcare climate would make this any easier at all. With ongoing cut in per RVU reimbursement, climbing insurance denial rate (https://www.pbs.org/newshour/health/analysis-health-insurance-claim-denials-are-on-the-rise-to-the-detriment-of-patients), I’m somewhat pessimistic that CMS would give special boost for this type of service. Commercial insurance will just follow suit. To inflate this rate and supplement the payment, the hospital will need to have extra money; while many healthcare corporates these days are running on negative margin. Healthcare policy experts please let me know if this is not true!
We ALL need to stop this and other free services! Perhaps the IDSA should pursue ‘organizing’ us — unionizing — to achieve the bargaining power we lack. We are all too collegial to do this on our own.
Speaking as a patient, I can assure you this service is worth more to us than what you’re being paid. If the alternative is an in-person or video visit with a specialist, co-pays alone can be $50 or more, and if we have a large deductible, it’s an even bigger out-of-pocket cost. And that doesn’t factor in time, parking, etc.
“No one has figured out how to pay for these things.” hitting the nail on the head Paul. When one looks back on a long career of providing “free” information to colleagues (and also hours of phone consultation time with HIV patients and family) – I later in my tenure had the “lawyers to this by the minute” epiphany. Why can’t we do this as doctors? My wife’s response – you would never want to be a lawyer”. Maybe like other things (single-payer system), the next generation will figure this out from an ethical and equitable perspective.
My response is going to be terribly depressing (but read the bottom, where the optimism is!)–we are a cognitive specialty–and without a specific procedure other than “the conversation”–most of what we do is a deeper dive into multivariable analysis–which for so many cases of MDRO organisms means tracking the inexorable trajectory of patients’ functional decline leading to more (futile) medical interventions and more “infections” (A whole other story–antimicrobial stewardship being a euphemism which obscures the real need for medical care stewardship–I mean–trach/peg in dementia–??–big $$$ but a total wasteful inhumane disingenuous fraud)–but back to being a cognitive specialty–maybe we all need to work with the AI business and allow ourselves to be replaced by impersonal AI–then if there is an adverse outcome, the “institution” that subscribes to the AI is responsible. The input into the AI will be the devil in the details–the long story that we ID docs diligently put together.
But that said–I am a real fan of econsults, given the time. They are often a great opportunity to research a clinical question and read the literature–I am enjoying my “second” (non-HIV) career in ID!
We collaborate with our colleagues via econsult to educate them and thereby elevate everyone’s competence. It is so valuable, is is so efficient, it promotes so much collegiality among disciplines–hospitals need to recognize this, and they should pay for it in the form of our salary with discretionary time to answer questions–albeit in the EMR. I often offer to see the patient after the consult when I am in much better position to discuss what is often a hard to answer question.
so, yes to econsults
and maybe yes to getting involved with AI with capability of interrogating the reams of data from multiple sources that inform our decisions–might actually be a great way to learn!
Thanks very much Paul for this discussion. The low reimbursement has been such an issue! Here are UW, its made it very difficult to convince ID faculty to spend time fielding eConsults. Until someone figures out how to pay for these at a reasonable rate, or reimburse specialists adequately for their time spent on them, its going to be tough to sustain the programs, despite all the benefits.
Thanks, Brian — 100% agree. Your experience is similar to many of the people I’ve contacted (and to ours).
-Paul
I am in private practice but work in a university community teaching hospital . I let people epic chat me . If it is a simple question I can answer I answer it . If I think I need to see the patient I tell them I need to see the patient and I see the patient .
I was brought up that we are supposed to do what’s best for the patients . I like to answer questions . And when I need a question answered I have no problem getting it answered or the patents seen . Collegiality.
Hi Paul- Since 2017, I have been running a WhatsApp service providing ID advice to doctors in South Africa who don’t have ID docs to consult face-to-face. (As there are <50 ID docs in SA it's most of them.) No money is involved, it all runs on good will from the ID community and so far has proved a hit. I understand that very large scale services require money but a lot can be done with good will.
I do not believe that “nobody has figure how to reimburse this”. On the contrary, “they” know we save money to the “system” doing this, “they” just want to pay little or ideally nothing. In fact “they” figure initially that 50 back was Ok, but then “they” kept it flat, because they can get away with this.
The only thing “they” have not figured yet is how to make us work for free, and believe me ” they” have tried hard.
Dear Paul, thank you for your thoughtful comments.
As above, it may be time to unionize ID. ‘They’ may finally value cognitive services more.
Patient POV: PLEASE, you esteemed specialists caring for me, DO consult with one another! I have recently been trapped in what in baseball would be called a “pickle,” wherein postsurgically I wo anduld regularly bleed, because of being on both Eliquis and Plavix, thus not allowing the surgical site to heal (let’s not go into the effects of spontnaneous bleeding, blood loss, plunging H&H) but of course NO physician will say to a patient “don’t take your blood thinners.” The surgeon and the cardiologist ping-ponged the decision between them via me; I was left managing an intractable problem on my own. Finally an astute nurse in the anticoag clinic initiated a convo between the two specialists aand my PCP, to give me a decision. When there are no good options, don’t let the patient just fall through the cracks.
And yes, these lovely physicians probably did not get paid for the time they spent on this consult. Thank you to all for the Good Will.
I work for value based primary care and econsults are a vital part of my job. I do several a week. We use Sitka which is a wonderful platform. I have no idea what the consulting physicians are re-imbursed, but my company highly encourages them as the cost of in person consult is so much higher. Value based care is where it is at!
My flu shot at the CVS. Pharmacy paid $40 for injection of prefilled needle into my deltoid by Vaccine “Technician”.
0.5-1 RVU for e-consult for using the code and even the $50 that the hospital pays within their system remarkably under values this needed service.