An ongoing dialogue on HIV/AIDS, infectious diseases,
October 20th, 2016
Back to School: Questions from “ID in Primary Care” — Shared and Answered!
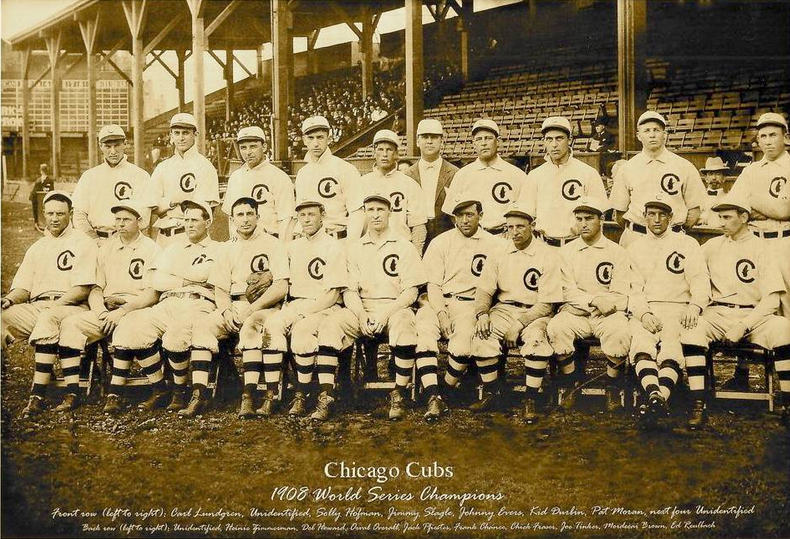 Once again, we’re giving our “Infectious Diseases in Primary Care” post-graduate course in beautiful Boston — where the weather is perfect, the air crisp and clear, and we are all watching with excitement as the few remaining baseball teams and presidential candidates make a mad dash to the end of their respective races.
Once again, we’re giving our “Infectious Diseases in Primary Care” post-graduate course in beautiful Boston — where the weather is perfect, the air crisp and clear, and we are all watching with excitement as the few remaining baseball teams and presidential candidates make a mad dash to the end of their respective races.
(You might have heard something about that.)
As in the past, we get a boatload of excellent questions from our participants, most of whom are highly experienced primary care clinicians. Note that not all of these questions have a definitive answer, so if you have an opinion or want additional clarification, please weigh in!
Off we go:
- One of my patients had a positive tuberculin skin test, but didn’t believe it, so I sent a [insert brand name here for your interferon gamma release assay of choice, which I hate typing]. That came back as negative. The blood test is more accurate, isn’t it?
We get this one every year, so might as well start off with it! The problem here is that there is no “gold standard” for diagnosing latent tuberculosis — it’s easy when they both agree, but sometimes the TST is positive but not the IGRA, sometimes the reverse, and neither test has 100% sensitivity. The main advantage of the IGRA is that it is less prone to false-positive results from either BCG or non-tuberculous mycobacteria. In the case when you have a discordant result, go with the one that you think makes the most sense based on the likelihood of lifetime TB exposure — and don’t forget to use the invaluable Online TST/IGRA Interpreter to help guide your decision! If the stakes are particularly high (e.g., about to get TNF inhibitors), act on the positive result. Read more on this topic here. And to reiterate, typing the brand names of IGRAs is NO FUN AT ALL, but here goes: QuantiFERON-TB Gold In-Tube and T-SPOT.TB. Good grief. - My patient doesn’t want to get the zoster vaccine since she’s afraid of getting a live-virus vaccine. Should I just wait until the inactivated vaccine comes out and then immunize her?
Sure, it’s reasonable to wait. The inactivated zoster vaccine has been tested in multiple prospective clinical trials (for example this recently published study in adults 70 or older), and is highly effective at reducing the risk of zoster, and also quite safe. Currently under FDA review, it will probably also require vetting by the American Committee on Immunization Practices (ACIP) before insurance plans will cover it. The current live-attenuated zoster vaccine is also safe and effective, but since zoster immunization is hardly urgent, if your patient wants to wait, that’s probably the way to go. Hey, I heard the vaccine may carry the nifty brand name “Shingrix”. I make fun of lots of brand names on this site — Fulyzaq, R.I.P. — but got to give credit when the marketers come up with a good one, and “Shingrix” is emphatically one of those. - Do we really need to get a chest X-ray on a young patient with suspected pneumonia? Why not just treat them based on physical findings?
The primary reason to get a CXR is that the optimal antibiotic choice depends on what part of the lung is involved — levofloxacin, for example, is particularly effective in the left lung. (That was a joke. Ha.) Actually, my colleague Mary Montgomery fielded this one, so I’ll let her answer: “It’s important to get a CXR in order to avoid giving unnecessary antibiotics for acute bronchitis, which gets better without them — most are viral. We used to think that any radiation exposure was worse than antibiotics, but as we are learning more about the microbiome and antibiotic resistance the risk equation is changing. The radiation risk from one CXR is equivalent to 10 days of natural background radiation. (For comparison a mammogram is equivalent to 7 weeks of natural background radiation and a PET-CT is equivalent to 8 years!) And every antibiotic dose risks changing the microbiome, causing antibiotic resistance, or leading to C diff.” - How do I choose between the multiple flu vaccines available?
Choosing among the current flu vaccine options is like trying to choose a breakfast cereal in a large US supermarket — there’s simply too much choice, and that’s without the live intranasal vaccine this year. Regular dose, high dose, trivalent, quadravalent, adjuvanted, eggless, mercury-free — pretty soon they’ll be offering them with free WiFi and a breakfast buffet. The ACIP won’t put their money down on any single vaccine brand, essentially saying “Get any of them — they all work.” Note the latest entry to this dizzying array of options — a recombinant egg-free quadravalent vaccine. I suspect the various Guidelines Committees are awaiting more definitive efficacy data, especially on the high-dose vs regular dose option — until then, we a study showing somewhat better response rate to the high-dose vaccine in the elderly. Some think this is enough to use the high-dose in the elderly, others don’t. - I heard the flu season last year didn’t peak until March — is that because we’re vaccinating people earlier in the year, and their antibody protection wears off in late winter?
While there is evidence that antibody titers decrease over time after influenza immunization, this is not the reason the season peaked in March last year. Flu season peaks change year to year, usually falling somewhere in the northern hemisphere between December and March. As to why it varies like this, only the people who can predict the severity of the upcoming flu season can tell you. (Big secret: They don’t know that either.) - I saw someone in my office recently who told me he was on a plane for 3 hours next to man who was coughing the whole time. He’s worried he might have been exposed to TB. How long should I wait before testing him?
You should test him now, to establish a baseline — especially if you don’t have a prior negative one on file. Since it takes 2-8 weeks to generate an immune response to TB after exposure — and it’s the immune response we’re measuring with both the TST and the IGRAs — guidelines suggest waiting 8-10 weeks after exposure for the second test. Remember that converting from negative to positive has a greater urgency for preventive treatment, as the risk for active disease is much greater in the first few years after acquiring TB. And while most people who are coughing a lot on planes do not have tuberculosis, I’m going to propose that airlines have the equivalent of negative air flow rooms for their coughing passengers. Can’t be too sure, right? - I take care of patients in a capitated healthcare system, and we’re grappling what to do about hepatitis C treatment. It’s just so expensive!
If you agree that curing HCV before there’s significant liver fibrosis, cirrhosis, hepatic decompensation, cancer makes sense — and of course you do, it’s medically irrefutable — then we have to prescribe these treatments for our patients. The good news is that the cost is way down from the crazy “SIM-SOF” days of 2014, when curing a single patient of HCV could easily cost > $100,000. There are now numerous options for therapy, in particular for genotype 1, all of them more than 95% effective and many consisting of just one pill a day for 12 weeks. This wide range of choices has had the expected effect on pricing, with deep discounting off of “average wholesale price” now the expectation for all insured patients, whether their coverage is private or government payer. So if you haven’t looked into it for a while, you’ll likely be pleasantly surprised — estimates of current cost/cure are roughly $20-40,000/patient, depending on the regimen and the payer. Still a lot of money, but think of what we’re getting in return! - Can you please continue to put fun videos on your blog?
Gladly. Meanwhile, if you have some questions appropriate for this course, post them in the comments section below, we’ll do our best to answer. And next year’s course looks like it will be October 25-27.
[youtube https://www.youtube.com/watch?v=K_7k3fnxPq0]
(Hat tip to Joe Posnanski for the video.)


Thanks for the outtakes. Was about to ask “Are you sure no animals were harmed in making this video?”
Steel-lined bike shorts?
Indeed. OUCH!
Great conference and awesome blog. Thanks, Paul!
Excellent post, as always Dr. Sax. I would like to add, if i may, that a Chest X-Ray also gives important information (e.g ruling out a pleural effusion that might get unnoticed on physical examination; also the type of pneumonic infiltrates can give us a hint if there´s an atypical bacteria causing it).
Also, I would like to ask about a case scenario: Pregnant HIV + woman at week 36 of gestation, on cART, VL below 20 copies/ml. According to an analysis from the French Perinatal Cohort (ANRS-EPF), IV-AZT was not significantly associated with a lower risk of mother to child transmission. So, my question is, in real practice do you still prescribe IV-AZT in this scenario? Thanks in advence
Cheers from Argentina!
Testing a person for TB just because he’s been sitting next to a person who coughed a lot? Are you really serious? And chest Xrays in young patients who are suspected of pneumonia? And levofloxacine for a chest infection in a young person, (even if the left lung might is a joke): you’re not really prescribing that, are you? No wonder there’s so much Cdiff floating around in the States and the costs of Healthcare are rising out of control.