December 11th, 2020
Why Does Diversity Matter in Residency Training?
Holland Kaplan, MD
As residency interview season ramps up, the topic of diversity arises frequently. Residency programs emphasize diversity in the locations at which their trainees practice, the variety of patients their trainees have the opportunity to see and care for, and the characteristics of the residents they matriculate. Diversity is an important characteristic of residency programs for applicants to be aware of and question during their interviews.
Practice settings
At my residency program, we rotate through a county hospital, a Veterans Affairs hospital, a private hospital, and a specialty cancer center. At our county hospital, I have seen and treated patients with disseminated tuberculosis, cerebral malaria, pyogenic liver abscesses, lupus cerebritis, and almost every type of vasculitis I learned about in medical school. I also had the opportunity to learn about the importance of community resources to patients who have very limited resources of their own. At our VA hospital, I had the privilege of taking care of older patients with innumerable decompensated chronic medical conditions, including patients with heart failure, cirrhosis, end-stage renal disease, and chronic obstructive pulmonary disease. I learned what it truly means to be a “fighter,” in multiple senses of  the word. At our private hospital, I cared for profoundly immunosuppressed patients who had received organ transplants or bone marrow transplants in addition to patients on varied types of advanced mechanical circulatory support that I never would have seen at our other hospitals. And finally, at our specialty cancer center I treated patients with both rare and common malignancies in different stages who had the chance to receive experimental treatments only available in limited hospitals in the world. Having experienced this diversity of practice settings, the treatments offered and not offered at each, and the variety of patients I had the opportunity to see, I think having a diverse residency training experience rotating at only one type of hospital would be challenging.
the word. At our private hospital, I cared for profoundly immunosuppressed patients who had received organ transplants or bone marrow transplants in addition to patients on varied types of advanced mechanical circulatory support that I never would have seen at our other hospitals. And finally, at our specialty cancer center I treated patients with both rare and common malignancies in different stages who had the chance to receive experimental treatments only available in limited hospitals in the world. Having experienced this diversity of practice settings, the treatments offered and not offered at each, and the variety of patients I had the opportunity to see, I think having a diverse residency training experience rotating at only one type of hospital would be challenging.
Patients
As physicians, we have the honor of taking care of patients from many different walks of life. We have a professional obligation to provide compassionate care to all of our patients. Open-mindedness is an important trait for a physician, and this trait primarily develops from exposure to a variety of people. I have had the opportunity to care of patients who have, for a variety of reasons, been excluded from the standard medical system. In one day, I have cared for patients who speak only Spanish, Urdu, Farsi, or Vietnamese and are surprised when I go to the effort of calling an interpreter to converse with them instead of trying to use English. I have treated women who have been sexually assaulted multiple times throughout their lives and refuse to be examined by male physicians. And I have cared for a transgender patient who was refused care by her primary care doctor who had used derogatory terms; the patient had developed a fear of seeking out healthcare. Our ability to serve as physicians and advocates for our patients is partially dependent on our ability to empathize with them and their life experiences. Achieving this empathy is much more difficult if you have never taken care of a non-English-speaking patient, a sexually abused patient, or a transgender patient.
Co-workers
Finally, I think having the opportunity to work with co-residents, fellows, and faculty coming from a variety of backgrounds in terms of race, ethnicity, sexual orientation, religion, and abled-ness truly allows one to respect different types of people. Any residency program touting its “diversity” should have that diversity represented not only in the patients who trainees see, but also in the trainees it selects for its program. Your co-residents are the people you grab coffee with after a long call in the ICU, go to the program holiday party with, run ideas by when you are unsure of what to do for a sick patient, and who ultimately will probably become your lifelong friends. Working with colleagues from backgrounds different from your own is the best way to develop a better understanding of and foster respect for our differences.
I feel privileged to have trained at an institution that has diversity in training sites, the medical conditions we see, the types of patients we have the chance to care for, and the backgrounds of the residents with whom I trained. For those applying to residency now, I suggest focusing some of your questions for the residents and program leadership on how they can offer you diverse medical training to enable you to get the most robust training experience for you, both personally and professionally.
What are some other reasons diversity is important in residency training?
November 24th, 2020
“They Don’t Make ‘Em Like They Used To”
Vivek Sant, MD

Dr. Sant is a General Surgery Chief Resident at NYU Langone Health, Bellevue Hospital, and Manhattan VA in New York, NY.
“When I was your age, I walked to school uphill both ways, barefoot in the snow!”
One of my favorite anecdotes from my attendings is about the cardiothoracic ICU experience in the ’80s and ’90s. Reportedly, each resident would arrive on day 1 of the rotation and would remain in the ICU for 30 straight days, being let out for an hour on Sundays — if there was time. I’ve heard it corroborated by so many people, I’m beginning to think that it might actually be true!
While this training model might have had benefits, re: continuity of care, immersive learning, and opportunities for autonomy, it is obviously unreasonable. In recent years, duty-hour regulations have been implemented to protect residents and patients. In 1989, New York state adopted the Bell Commission’s duty-hour restrictions, including the 80-hour work week. In 2003, the ACGME adopted these restrictions across residencies and specialties throughout the U.S.
Today’s training model is kinder. Not surprisingly then, older generations seem to think subsequent generations have lost a certain toughness and ability to handle stress, leading to an overall cultural decline. Interestingly, attendings have rarely been the ones to make me feel lesser for not being forged in the same crucible. Instead, I’ve noticed (and probably contributed to) these expectations of greater toughness and less entitlement from senior residents, and this cascades on down to the interns and medical students.
Fear can hinder learning opportunities
I remember my chiefs and senior residents from my intern year. I was simultaneously in awe of them and terrified of disappointing them. While they sometimes were tough on us, they, in turn, would talk about how much harder their chiefs had been on them! They would laugh among themselves: “Can you imagine if we had asked our chiefs that? Can you imagine if we had presented a consult to our chiefs that way?”
I have learned a tremendous amount from my seniors, and I am grateful for their mentorship. I wonder, though, if I might have learned a lot more with a relationship based less on fear. In the OR recently, I instructed my junior resident, “We’ll place the purse-string sutures, then move on to the Stamms.” “Could we quickly just go over Stamms again?” she replied. I would never have dared to ask my chiefs such a question! (“They’ll think I don’t know… what if they make me feel dumb… they won’t let me place the stitches.”) But I really wish I could have felt uninhibited enough to ask for clarity on a technique! I could have learned so much more. I didn’t think less of the questioner, our attending didn’t seem to mind either, and we ended up sharing a great learning opportunity.
 Culture shift
Culture shift
Ever since my own intern year, I have seen residents collectively judge each new class of interns. “They don’t have the same feeling of responsibility that we did.” “They’re part of the shiftwork generation.” “They complain too much.” “They ask questions without even trying to figure it out themselves.”
My peers and I seem no different than our predecessors in how we view each incoming class. However, I believe we are more understanding of the growing emphasis on work-life balance. This is reflected in how the program’s priorities have changed: We now try to get residents into the OR as much as possible, starting intern year, and there is more focus on wellness and learning. These changes are decidedly positive — we try to get residents home on time whenever possible, we don’t make them sit around idly waiting for their chiefs until 9 pm every day, and we want them to be happier, be more rested, and have more opportunities to learn and operate.
Solution: Clear expectations and greater empathy
As part of this culture shift, residents have a more collegial working relationship: What used to be implied in relationships based on fear is now communicated explicitly in more humane terms: “You should go home on time, but I expect you to complete these tasks and update me before you leave” or “I want you to assess any issues and propose an action plan before you escalate it to me.” Setting clear expectations can take time and might seem harsh, but helps eliminate any misconceptions held by the newer residents. This is invaluable for both resident and patient.
Recently, I talked with one of my attendings about this issue and asked him how he remained patient with all of us residents. He replied, “I worked very hard as an intern, but when I reflect honestly, I know I wasn’t the best intern at all times! I missed out on many major life events of my family and friends. These realizations have made me more understanding of today’s residents.” Such candid self-reflection, humility, and empathy go a long way in helping bridge the gap between instructor and student.
A few months ago, a junior resident called me during the night to clarify something. Such a call would have had one of my former chiefs spluttering, “Why didn’t you call the pharmacist and ask her to help you?” I calmly addressed his questions and hung up. As I was drifting back to sleep, pondering why the resident felt he ought to call me about this issue, I had a brief flash of clarity, “I’m glad he felt comfortable asking me!”
November 19th, 2020
Where DO We Go from Here? Being an Osteopathic Physician in 2020
Stephanie Braunthal, DO
The latter portion of 2020 has brought forth an unfortunate series of comments in the news, on social media, and even in the ad of a fashionable scrub company that called into question the credibility of DOs to practice medicine and surgery and to serve as public health experts. As a proud graduate of an osteopathic medical school and who, as of this past month, is officially an ABIM-certified internist, the attacks are frustrating, but unfortunately not entirely unfamiliar. Many of us, regardless of how specialized we become, at some point over the course of our careers find ourselves explaining or justifying our credentials to patients, peers, and mentors who are less familiar with our degree. While no opinion is universally held within the medical community, some of my MD colleagues admit to previous biases against DOs, which abated as soon as they worked with them as colleagues or taught them as medical students and residents. It is for this reason that increased representation matters, particularly at an unprecedented time when conspiracy theorists will use any means possible to question the integrity of medical professionals.
2020 also marks a momentous milestone in graduate medical education: the completion of the ACGME single accreditation process, a five year endeavor which consolidated the governance of previously osteopathic and allopathic training programs. Osteopathic medical students no longer have to choose between residency matches (the American Osteopathic Association-affiliated programs previously had a separate match), and allopathic candidates can now apply to programs that were previously limited to osteopathic alumni. Training MDs and DOs side-by-side will thus become increasingly common. My hope is that normalizing the heterogeneity of trainees will not only lead to further promotion and publication of osteopathic physicians, it will also engender more subtle nods to our parity. Examples include removing the expectation that DO students need to gratuitously sit for the USMLE in addition to their COMLEX-USA licensing exams, or even evolving expressions such as “MD aware” to include DOs.
 Thank you to everyone reading who rallied to the defense of DOs as we were misrepresented over the past few months. As we approach the 2021 recruitment season, I implore you to take your support a step further. Reflect on whether your institution regularly welcomes residents, fellows, and faculty who graduated from osteopathic medical schools, and if it does not, please consider these candidates for your program. We are competent, compassionate, and ambitious physicians, whose additional training in manipulative medicine gives us a unique perspective on prevention and ways to conservatively augment care. When given the opportunities, we rise to leadership positions and make significant contributions to our fields, mentoring our allopathic and osteopathic contemporaries along the way. So, hire us. The more we are included, the more we all succeed.
Thank you to everyone reading who rallied to the defense of DOs as we were misrepresented over the past few months. As we approach the 2021 recruitment season, I implore you to take your support a step further. Reflect on whether your institution regularly welcomes residents, fellows, and faculty who graduated from osteopathic medical schools, and if it does not, please consider these candidates for your program. We are competent, compassionate, and ambitious physicians, whose additional training in manipulative medicine gives us a unique perspective on prevention and ways to conservatively augment care. When given the opportunities, we rise to leadership positions and make significant contributions to our fields, mentoring our allopathic and osteopathic contemporaries along the way. So, hire us. The more we are included, the more we all succeed.
November 4th, 2020
The Rise of the Fall
Masood Pasha Syed, MBBS
Having matched into a residency in New England, I was super excited to experience all the seasons. I grew up in tropical countries where we had two seasons — “rainy season” and “not-so-rainy season” — both of them superimposed on reasonably warm temperatures. Three years out of residency and still in New England, I enjoy all the seasons, but fall is most definitely my favorite. The vibrant colors, the earthen smell, the leaves’ different shapes and sizes — I just can’t get enough of it. Apart from how picturesque it can be, fall has also been a time for reflection for me. Every year, the leaves change colors, take on new characteristics, and then fall — only to come back again in the spring. Each year through internship and residency, we take on new responsibilities, many times rising to the occasion but sometimes falling in failure. But what matters for the tree is that its roots are strong enough to make it through the winter. In much the same way, what matters to us is having the perspective and insight to make it through our failures.
Failure in Medicine
I remember the first time my father spoke to me about failure. After graduating from his medical school in India, he had not matched into post-graduation (residency equivalent) for Internal Medicine. Instead, he went directly to serving patients of low socioeconomic backgrounds. A year of service taught him about perseverance and resilience. He then matched into his newfound interest in General Surgery and held on to the lessons learned during his hiatus. He said, “many doors have to close for you to come to the door you are meant to open.” I remember how strange this topic of failure sounded to me — I was raised to chase perfection through my school and college years to get into medical school. Failing did not seem to be an option in the profession I had chosen.
Since then, I have faced my share of failures during my journey of transitioning to the U.S. I firmly believe these have been instrumental in shaping me as a physician and the person I am today. Although we encourage improving patient outcomes by discussing medical errors and mishaps — mortality and morbidity rounds, Schwartz rounds, and quality-improvement initiatives; we rarely encourage physician well-being by discussing personal failures in medicine. Many students meet step score requirements in medical school with flying colors; many match into residencies of their choice. Many residents match into fellowships or jobs of their choice. But what about those who don’t? Also, despite our best efforts, some of our patients do well, and some do not. How can we deal with unfavorable patient outcomes or deaths if we train in a profession that does not normalize failure? Failures in life and in medicine are inevitable. Hence, we need to build a platform to initiate this discussion safely.
 How can we do better?
How can we do better?
Failing to fail results in success. What does this mean? The fear of failure should not stop one from challenging oneself or going out of one’s comfort zone. We are bound to fail at some point in our lives and careers. Hence, one should prepare for failure with contingency plans.
We can begin by encouraging a culture in medicine where we share from our experiences: not just our positive achievements, but also our negative attempts and lessons learned from them. Listening to our mentors speak about their failures can help normalize this process. Perhaps, we can do this in small-group settings where there is one-to-one attention and encouragement. Once we are comfortable doing so, we can think of having a formalized curriculum where our senior physicians share their own personal stories of failures and help bridge the gap by discussing this vital component of our careers. Including failures as a part of our narrative helps build our younger colleagues’ perspective. Failures can be eye-opening experiences that enrich our character and provide us with tools to deal better with uncertainties. In the long term, this will help us be better physicians — explaining the anticipation of positive outcomes to our patients and coping with the negative ones.
I recognize that just talking about this is not a fix for the problem. However, I believe this small step from us can become a giant leap in the right direction for our medical community. I encourage the readers to share their experiences to help take the narrative forward.
October 26th, 2020
Futility as a Cause of Burnout in Residency
Holland Kaplan, MD
At the beginning of my residency training, one of our program leaders defined burnout as “work out of proportion to meaning.” In a sense, I think this also defines futility – performing a disproportionate amount of work compared with the results or meaning you are deriving from the work. The proposed causes of burnout in residency are broad – emotional exhaustion, depersonalization, lack of “resilience,” inordinate workload, sleep deprivation, and lack of time for leisure activities. However, the perception of futility also plays a significant role in burnout for residents. Below, I outline how feelings of futility contributed to my personal periods of burnout during residency.
In the ICU
I grappled for a long time with whether critical care was a good fit for me. I enjoyed the complex physiology, the consistent application of all areas of internal medicine, and the opportunity to help patients and their families through extreme illness and sometimes death. But I noticed as I completed my ICU rotations that I routinely started experiencing burnout and severe emotional exhaustion about 2 weeks into these rotations. Having experienced burnout of various durations in different settings throughout residency, I wondered what the precise cause of my burnout was in the ICU environment. Several years ago, I wrote about an experience I had as a second-year resident in performing CPR on an unfortunate elderly patient with multiple untreatable medical conditions. For this patient, CPR was never going to be helpful. I argued that my patient with severe anemia, heart failure, and metastatic cancer, had he been resuscitated, would still have had severe anemia, heart  failure, and metastatic cancer. A portion of my ICU experiences centered on what I felt were futile efforts at resuscitation of patients who would never benefit from CPR. I reasoned that surgeons have the option to withhold interventions that have a low likelihood of success; why are we in medicine forced to perform a procedure (CPR) that in many instances has a success rate so low that a surgeon would never operate with those same odds? My disgust with performing CPR on patients in which it was futile reached the point that I rushed to run codes for fear of otherwise having to perform chest compressions. I spent many sleepless nights during and after ICU rotations grimacing at the thought of an elder’s osteoporotic ribs snapping beneath my hands like twigs in a futile effort to revive them. This perception of intense futility led me to burnout on all of my ICU rotations and ultimately turned me away from a career in critical care. Thankfully, many satisfying and rewarding aspects of critical care draw residents to this field, including the ability to see fast turnaround in very sick patients and interesting and complex pathophysiology. But the emotional aspects can truly contribute to feelings of futility and burnout.
failure, and metastatic cancer. A portion of my ICU experiences centered on what I felt were futile efforts at resuscitation of patients who would never benefit from CPR. I reasoned that surgeons have the option to withhold interventions that have a low likelihood of success; why are we in medicine forced to perform a procedure (CPR) that in many instances has a success rate so low that a surgeon would never operate with those same odds? My disgust with performing CPR on patients in which it was futile reached the point that I rushed to run codes for fear of otherwise having to perform chest compressions. I spent many sleepless nights during and after ICU rotations grimacing at the thought of an elder’s osteoporotic ribs snapping beneath my hands like twigs in a futile effort to revive them. This perception of intense futility led me to burnout on all of my ICU rotations and ultimately turned me away from a career in critical care. Thankfully, many satisfying and rewarding aspects of critical care draw residents to this field, including the ability to see fast turnaround in very sick patients and interesting and complex pathophysiology. But the emotional aspects can truly contribute to feelings of futility and burnout.
On the inpatient wards and in the clinic
I remember inpatient wards and certain experiences in clinic during intern year being particularly rife with feelings of futility. The emotional distress on the wards and the clinic focused more often on the inability to provide patients with the care I felt they needed and deserved, but were unable to obtain, due to insurance or other systemic limitations. However, in these settings, a unique fuel for these feelings of futility centered less on emotional distress. I remember feeling inundated with endless documentation, phone calls for prior authorization requests, trying to meet unknown requirements to get patients to subspecialty appointments, and struggling to get help from ancillary services like physical therapy and social work to discharge patients to a safe living environment. I recall spending 60 minutes on the phone with an insurance company to ask them to approve an SGLT-2 inhibitor for my clinic patient, only to have them tell me they had to try two other oral diabetes medications first. I remember endless wait times with the appointment scheduling line for our health system, only to be told that the creatinine on the lab from last week was not recent enough for the patient to get a CT scan with contrast; I would need a more recent creatinine value. These experiences are not unique, physicians both in practice and in training report a significant administrative burden in the inpatient and outpatient settings that contribute to burnout. The feelings of futility regarding the time spent on an objective compared to the outcome achieved (or not achieved) was a major cause of burnout for me.
Combating burnout
So, how can residency programs alleviate burnout in their residents? This question is worthy of its own blog post, and I think the answer differs based on the cause of the burnout. However, with futility as a common thread among multiple causes of burnout, I think emphasizing and celebrating the things trainees are doing that are making a difference for their patients is critical. For a resident who just performed 30 minutes of chest compressions on a patient who was never going to survive, it makes a difference to say “Hey, I know those chest compressions were rough, but I think the way you called the code at the end and asked for a moment of silence was really meaningful for the family and for the patient’s memory.” Or for a battle-worn resident who has just gotten off a long call with an insurance company, a supervising physician could make an impact by saying, “I know those calls can be frustrating, but look at the improved glucose control you’ve achieved on this patient since meeting him. We’ll try these other meds first, and next time we’ll know the requirements for this insurance company.” Whether you’re a colleague or a supervisor for a burned-out resident, never underestimate the power of a few encouraging words in the face of feelings of overwhelming futility.
Sources:
Mian A et al. Medical student and resident burnout: A review of causes, effects, and prevention. J Fam Med Disease Prev 2018; 4:1510094. (https://doi.org/10.23937/2469-5793/1510094)
Ishak WW et al. Burnout during residency training: A literature review. J Grad Med Educ 2009 Dec; 1:236. (https://doi.org/10.4300/jgme-d-09-00054.1)
October 16th, 2020
Advancing Patient Safety in the COVID Era and Beyond
Frances Ue, MD, MPH
The U.S. continues to lead the world with almost 8 million COVID-19 cases and rising. The resurgence of coronavirus cases in areas previously unaffected or with cases under control shows how vulnerable our society is to the ravages of this disease and the devastating toll it can take on affected livelihoods and communities. It can feel at times that the progress made in the spring has been lost — but I urge you not to lose hope.
The COVID-19 pandemic exposes the weaknesses of our underfunded public health system and the challenges within our national leadership structure, both of which are needed to provide a coordinated response in this crisis. It also highlights the importance of our patient safety colleagues who continue to lead and innovate to ensure safe patient care. One such colleague is my dear friend, Dr. Liana Zucco. She is a Canadian British-trained anesthesiologist and a healthcare quality and safety fellow at the Beth Israel Deaconess Medical Center (BIDMC). I had the pleasure of interviewing her for this post.
(Interview transcript edited for length.)
Frances Ue: Tell us about yourself and what it’s been like being in the U.S. as a Canadian British-trained doctor?
Liana Zucco: I’ll first start by saying that I usually have to explain my origin, because when I say I’m a Canadian-born British-trained anaesthetic or anesthesiologist, everyone asks me what my accent is. There’s a lot of explaining, and everyone loves the story, they really do. And I find that I just keep on telling people about my life and about the journey that I’ve been on. It actually really makes me reflect on growing up and being a student in Toronto, moving to the U.K. for training, and now coming to the U.S. My experience moving from Canada to the U.K. was with my husband, and it became our adventure together. Whereas, this one is solo and trying to juggle a long-distance marriage comes with its own challenges.
It’s been very friendly coming to Boston and the BIDMC. From the anesthesia point of view, I am delighted that the drugs are the same and work the same way; the medicine is the same; the surgeries are the same. That’s really nice and comforting. Obviously the entire healthcare system is different. I thought that by being trained in the U.K. and constantly rotating from hospital to hospital, I was really good at adjusting, but this has been a whole different adjustment. It’s different adjusting to a whole new healthcare system.
FUe: Tell us about your experiences as a woman in medicine and anesthesia.
LZ: Similar to in the U.S., the anesthesia consultant (or attending physician) workforce in the U.K. is predominantly male (68%, Royal College of Anaesthesia, 2018). I certainly do feel that at many institutions, leadership roles are still male-dominated, but more and more, women are being promoted into these roles. Women need to see more women in leadership roles if they too are going to take them on.
I have been fortunate to have trained alongside many women and at times, female majority teams. There are days when I’m in the OR where I’m surrounded by female surgeons, female nurses, female anesthesiologists, and we certainly give each other a high five. And it’s really nice.
I think it’s important to have encouragement and support from the moment you enter medical school — making people aware that these specialties, like anesthesia, exist. And getting people involved and excited by it. It needs to be tackled early.
FUe: What makes you most excited about quality and safety?
LZ: I love the fact that, for most providers, especially junior providers, it is a ground-up movement. People get so frustrated working on the shop floor — they see problems, and they have no idea how to fix them, and they feel that they can’t. There are mechanisms in place for people to improve things from the ground up.
Quality improvement is looking at how organizations can not just be efficient but is actually examining why we should be doing x, y, and z, because it’s not just efficient but also benefits the patient and is safer. Good-quality care is safe care. And the moment that people recognize that is the most exciting. I am part of a specialty where that is literally the forefront — before you do anything else, it is safety first. In the U.K., I became the lead for quality improvement for DAPS (Doctors Advancing Patient Safety), and we published a how-to for junior doctors and started a program teaching quality improvement. That excites me the most — teaching people how to do quality improvement work. My heart just explodes with excitement.
It’s all different levels. Senior management get involved in one aspect, then interns get involved on another level. It’s not just doctors, it’s nurses, it’s super multidisciplinary. There’s a patient engagement aspect of it. It encompasses almost all of healthcare. And when I speak to patients on a daily basis, and they ask what my fellowship is in, they get excited when they hear that a fellowship exists in quality and safety.
FUe: Could you speak about your role during the COVID-19 pandemic?

An initiative to improve communication in the operating room with scrub caps made by Theatre Caps
LZ: As one of the quality and safety fellows within the department of anesthesia, we were tasked with figuring out how to minimize healthcare worker (HCW) infection. Specifically, how to minimize the risk of transmission and risk of viral exposure to HCWs who may be exposed during aerosol generating procedures. We knew from the Toronto SARS-CoV outbreak in 2002 that the majority of HCWs who became infected were intensivists, anesthesiologists, and nurses who were involved in aerosol-generating procedures, particularly in intubation and extubation.
It was our job to re-evaluate the entire workflow of a COVID-19-positive patient coming into the operating room, and we published these recommendations for the Anesthesia Patient Safety Foundation. We considered how to change the workflow, what measures we would change to enhance our infection control, and how to train the staff to follow these new guidelines. We created cognitive aids like checklists to be used in the operating room and trained staff through an in-situ simulation method which is in the actual work environment, to pick up the real hazards that exist and the real gaps in care. And every step of the way, we thought about how to minimize infection.
Our team disseminated the information that we developed, constantly made iterative changes to amend them if needed, and filled the gaps in our care, re-evaluation, training, etc. We started this about 1 month prior to the first COVID-19 case coming to our operating room. We trained over 400 providers in the perioperative department — nurses, surgical teams, surgeons, anesthesia residents, and others, and then we pulled in anesthesia providers from the community hospitals to do the same training. We did about 12 sessions a day for about 3 weeks. And then, that was it, and we just had to hope that it worked! And now we are measuring the impact of that, and we can safely say that not a single anesthesiologist became infected.
Now that the first surge is over, we are modifying all of these new standard operating procedures all over again to be ‘COVID-19 capable’ for the moment we know that a COVID-19 case is present. How do we go back to business as usual but be ready for a COVID-19 case? We had a COVID case the other day, and it was so delightful to hear the circulating nurses say, ‘yes, we need to do everything on the checklist and I have a copy here; we can’t start until we have a huddle.’ These are all things that we implemented, and it was so delightful that I didn’t even have to bring it up.
FUe: Where do you see your career headed?
LZ: My short term plans after this fellowship is done is returning to the U.K. to finish my anesthesia clinical fellowship (known as an advanced training module). In that time, I see myself trying to figure out how to combine a quality and safety fellowship and all the knowledge and experience I have gained, into a full-time working anesthesia career. I really thought I was a die-hard clinician and never wanted to spend a single day outside of the operating room or outside intensive care. However, this fellowship has really taught me that I actually really like a combination of both. I like the combination of having a non-clinical leadership role that has an immediate impact on clinical practice.
FUe: What words of advice do you have for residents who want to get involved in quality and safety research?
LZ: Quality improvement and safety research can be done efficiently, over a short period of time, and you will see the change happening in front of you — you will see improvement, or more efficiency, or a change in practice. It’s so rewarding. Do the online modules from the Institute for Healthcare Improvement to gain knowledge on the topic. Speak to your department because you will need a mentor for it, someone who believes what you believe and wants to change things in the same manner that you do. I have come to appreciate two phenomenal mentors — the director and supervisor of the fellowship, Dr. Krishna Ramachandran, and the director of the Master’s program, Dr. Anjala Tess.
FUe: Lastly, what do you miss the most about the U.K.?
LZ: I actually do miss the people. It’s really the people that make a place your home. I also miss having a role outside of the operating room from a professional perspective. Anesthesia covers everything in the U.K. — you cover intubations in the emergency department, you go on transfers from one hospital to another with an intubated patient. So you really feel like you have a family, not just at your own hospital, but in the entire region and city. I am a Southeast London trainee in the U.K., so I’ve worked at four different hospitals in the Southeast London region, and everybody does that and rotates around. So you feel like you have this enormous family from a professional perspective. From a personal perspective, I miss everything about London. I mean, what’s not to love?
Would love to hear from residents interested in quality and safety. What are your ideas to improve patient safety? Tweet at me, @TheFrancesUe or comment below.
October 7th, 2020
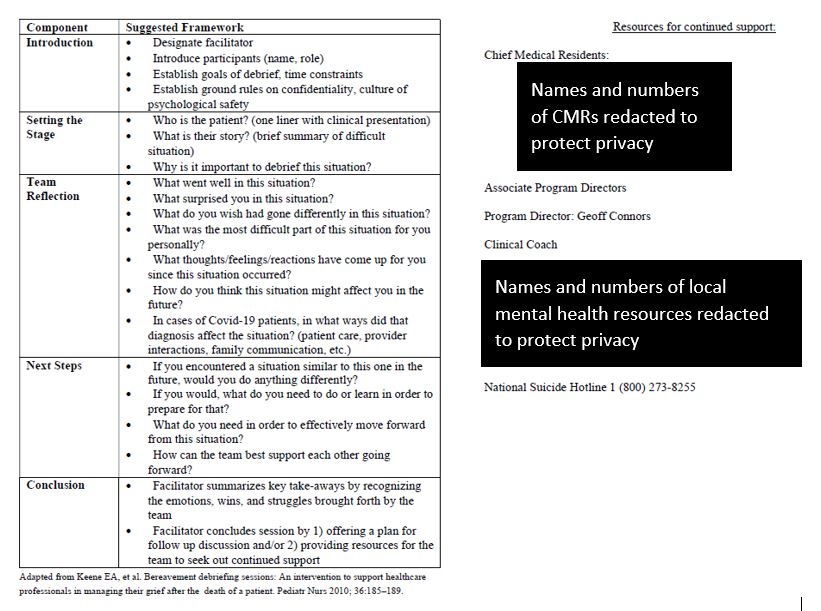
“We Did Everything We Could.”
Vivek Sant, MD

Dr. Sant is a General Surgery Chief Resident at NYU Langone Health, Bellevue Hospital, and Manhattan VA in New York, NY.
Can we do better when delivering bad news in trauma?
On a recent trauma call, we had a busy night, culminating in a horrific motorcycle trauma that came in early in the morning. The patient had devastating injuries and ended up dying. The detectives finally tracked down the patient’s family. I cleaned myself up, put on my white coat, and had the family sit down in a private conference room. I entered with my trauma attending and a consulting specialist and we sat down with them. I told them their loved one had been involved in a terrible accident, and asked them what they knew so far. I filled them in on the rest of the situation, explaining that we’d done a lot of work to try to save him, but the injuries had been too much, and he had died. We spent as much time as we could answering their questions and being with them as they processed the horrible news, and finally took them to see him. Naturally, they were devastated; I will never forget the wail of sorrow from his widow. While I have delivered bad news before, this experience felt different and far more difficult, emotionally.
The SPIKES methodology
Delivering bad news to patients is difficult; but with a methodology and practice, it can be made less difficult. The SPIKES methodology was developed by physicians at the MD Anderson Cancer Center in Houston (Oncologist 2000; 5:302), for delivering bad news to oncology patients. Optimizing the following parameters helped improve their patients’ experience:
- Setting – ensure a private, quiet place; sit down, invite other family members, avoid external interruptions
- Perception – assess the patient’s baseline understanding of the situation before diving into an explanation
- Invitation – provide initial information and offer the option of hearing further details
- Knowledge – warn that bad news is coming, give information in small chunks, and avoid jargon
- Empathy – address the emotional response with empathy
- Strategy – summarize concrete next steps
 In retrospect, we had addressed most of these issues as recommended. However, unlike the oncology setting in which this framework was created, or even the surgical context I am used to, the emergent trauma setting presented several unique challenges:
In retrospect, we had addressed most of these issues as recommended. However, unlike the oncology setting in which this framework was created, or even the surgical context I am used to, the emergent trauma setting presented several unique challenges:
- No previously established rapport – in trauma, providers do not have an earlier visit to establish a bond with the patient or their family; in contrast, rapport in oncology is built over time, and a connection is formed with patients preoperatively, prior to elective surgery.
- Traumatic injury is unexpected – a family member’s death is rarely on the family’s radar since trauma is unexpected. In oncology, patients have been considering their own mortality, and in elective surgery, families know their loved ones are being hospitalized for an operation.
- Patients are younger – trauma patients often are younger, where the loss is more unexpected and perceived to be more unfair.
- Fewer resources for grief support – traumas often present on nights and weekends, when the hospital is not as fully staffed with chaplains, social workers, and grief counselors who would otherwise be instrumental in supporting the bereaved family.
- No control of the narrative – various professionals work together to identify and contact family of trauma patients; they may not have training in delivering bad news or accurate updates on the patient’s status. So families sometimes arrive at the hospital without the appropriate foreshadowing of the complete situation and are shocked by the news.
We might feel discouraged that some of these aspects are immutable. We can’t control trauma patient demographics nor the unexpected nature of trauma. However, with training and funding, we can better steer the narrative and improve resourcing. And on an individual level, we can soften the blow through a deeper understanding of the specific nature of their pain (“No one should die so young”) when talking with families.
Resilience in the face of delivering bad news
Delivering bad news is tough. Delivering bad news in trauma is tougher still. And this takes a toll on healthcare providers as well. Thirty minutes after we talked to our patient’s family, wails of sorrow still ringing in our ears, we headed to the OR to take out another patient’s appendix. New patient, fresh game face, another battle to fight — with the same sense of purpose and urgency.
What strategies do you use for delivering bad news in the emergent trauma setting?
September 29th, 2020
Below Hospital Deck
Stephanie Braunthal, DO
There is debate about which of the many medically themed TV shows best depicts our lives in medicine. Is it the conundrums of House? The interpersonal drama of Grey’s Anatomy? The camaraderie and antics of Scrubs? While each of these capture unique problem solving, empathy, relationships, and burdens that accompany being a physician, I had yet to find a show that accurately reflected the day-to-day reality of being a resident. That is, until I discovered the Below Deck series on Bravo. Now, I know this seems silly. Below Deck? A reality show about the crew of super yachts that charter wealthy guests on luxury nautical vacations? Although the show does not feature a single doctor, save the occasional guest or local physician summoned to evaluate a deckhand’s injury, I find that, rather than constantly noting how inaccurate scenes are to real life (like I do with medical dramas), I instead draw parallels between the scenarios on the boat to those in the hospital. The show highlights struggles within a hierarchical work environment, discussions about duty-hour restrictions, occupational safety concerns, fast-formed friendships, and the occasional romances that strike as crews on each season work together to repeatedly achieve high-stakes outcomes. Starting to sound familiar? It certainly did to me.
The cast of each Below Deck series consists of a captain, first mate, engineer, chef, and two teams of deckhands and stewards. The latter each have an experienced lead (“bosun” on deck, “chief stew” interiorly), a moderately experienced second rank, and an inexperienced third rank. Structural comparisons are obvious. Residency programs have directors, program leadership, support staff, and chief residents who direct and oversee operations and the growth of the trainees. The residents themselves work in the hospital as pairs or trios, with a senior overseeing at least one intern. In the same way that crew members shuffle from yacht to yacht, residents rotate from service to service. While some characters recur, each season generally follows a new crew that has never worked together. Our residents similarly assume a role with universal responsibilities based on their postgraduate year (PGY) level, which makes transitioning between diverse rotations relatively seamless. Medicine is not hospitality, but it is nevertheless a service profession. While residents are not required to prepare elaborate meals or frivolous theme parties, their creativity is constantly pushed to the limits, expanding their differential diagnoses and navigating seemingly insurmountable obstacles to get patients the care they need. Both professions rely on the success of the group to not only ensure the safety of human lives, but also for career-promotion opportunities, which in the case of Below Deck is thousands of dollars worth of tips.
 The more episodes of Below Deck I watch, the more predictable the drama becomes: guests don’t like the food, the captain is disappointed in the crew, someone doesn’t answer the walkie-talkie, the chief and her stews aren’t getting along, and so on. Dissatisfaction, unmet expectations, and miscommunications are also common sources of tension in the hospital, particularly on teaching services where everyone has different degrees of experience. As they progress in training, the most successful residents not only learn to resolve conflict, they also develop strategies to avoid it. These include taking the time at the beginning of the rotation to define roles and expectations with the intern and attending, team communication, proactively reevaluating team goals, and regularly delivering feedback. Incidentally, when the Below Deck crews employ these tactics, they navigate the gratuitous requests of their clients and the unexpected perils of open seas with relative ease.
The more episodes of Below Deck I watch, the more predictable the drama becomes: guests don’t like the food, the captain is disappointed in the crew, someone doesn’t answer the walkie-talkie, the chief and her stews aren’t getting along, and so on. Dissatisfaction, unmet expectations, and miscommunications are also common sources of tension in the hospital, particularly on teaching services where everyone has different degrees of experience. As they progress in training, the most successful residents not only learn to resolve conflict, they also develop strategies to avoid it. These include taking the time at the beginning of the rotation to define roles and expectations with the intern and attending, team communication, proactively reevaluating team goals, and regularly delivering feedback. Incidentally, when the Below Deck crews employ these tactics, they navigate the gratuitous requests of their clients and the unexpected perils of open seas with relative ease.
While it might seem like I have been a fan since its inception, I only started watching Below Deck a couple of months ago as a frivolous escape from boards studying, chief responsibilities, and the serious realities of our world during the past year. I did not anticipate that the show would provoke so much introspection, nor did I realize how valuable it has been as a means of communicating my experiences during residency and chief year to my friends and family outside of medicine. Next time someone asks what it’s like to be a resident, I’ll simply say, “It’s like working below hospital deck.”
September 17th, 2020
What’s in a Number?
Sneha Shah, MD
Does your doctor’s age matter?
If I had $100 for every time I walked into a patient’s room, introduced myself as the doctor, and was immediately asked, “Hey, how old are you?” I might be able to retire right now — at the age of 28. Of course, I am exaggerating, and yet this question echoes for me and my baby-faced colleagues constantly.
Whether it’s simple curiosity or blatant reverse-ageism, I find this question erodes trust before it is built. I haven’t yet found an agreeable way to bypass it; I usually just state my age, before quickly moving on. Rarely, some congratulate me on my accomplishments given “such a young age.” But these felicitations are like writing in the sand, which quickly wash away in the waves of emotions I begin to feel the moment they ask me that question.
Why this question hits too close to home
Even though I am the oldest child in my extended family, my traditional Indian (specifically Gujarati) family considers me to be a kid. I keep hitting milestones — 16 to start driving, 18 to start voting, 21 to drink alcohol, 25 to rent a car — but I am still seated at the kids’ table at home. During holidays or celebrations, I often feel left out. Too old to play with the kids and too young to gain entry into adult conversations. I attempt to walk up to a group of aunties and uncles hunched over in a hushed conversation — abridging their conversation, they turn toward me and ask, “Aren’t you getting too old to not be married?” So, I am officially too young and too old at the same time.
I commiserate being in age-limbo with my brother, who shares similar sentiments. Nonetheless, there is a deep hurt that comes with never feeling trustworthy enough to hear family secrets. And, as I learned on my psychiatry rotation as a third-year student, I am using the mature coping mechanism of suppression to hide that hurt.
Similarly, I start to feel untrustworthy during patient encounters where my age is brought up — no matter how knowledgeably or confidently I began that interaction.
When your competency is questioned
As new physicians, we are required to start making decisions and to start practicing medicine. Even residents who haven’t had my cultural experiences know the feeling of doubting oneself for even minor decisions. We hold the precious privilege of caring for someone’s life, and mistakes can be grave. Knowing this, we double and triple check our work. Despite this, patients and colleagues continue to question us. When we are interns, they want the opinions of our seniors. When we are seniors, they want the opinions of our attendings. Even as an attending (my first time as a chief resident), a patient’s wife asked whether there was “someone above me” who could confirm my clinical judgment.
Unlike our patients, members of our interdisciplinary team might not blatantly ask our age, but there are undercurrents of skepticism. For example, nurses will look surreptitiously toward the critical care fellow lurking behind the senior resident who is running a code before acting on the resident’s requests. Pharmacists will congratulate interns for finally placing that antibiotic order correctly. We fall victim to the experienced physicians’ “back in my day” comments.
How we can grow together
There are times when I simply want to reference this article (BMJ 2017 May 16; 357:j1797) about physician age and patient outcomes — no difference! But, I choose to remember that 3 years of residency barely surpasses the 10,000-hour rule popularized by Malcolm Gladwell. And I am thankful for the talented and experienced healthcare providers that surround me. Countless times, an ICU nurse has whispered in my ear about which pressor to start. Pharmacists have alerted me on near-misses and helped me write the correct medication order. Nurse care managers took the time to explain the difference between Medicaid and Medicare. And, experienced physicians have taught me how to hold a patient’s hand and be a guide through the toughest time in his or her life. But, currently, we lack robust evidence about how physician age affects patient outcomes. Thus, we, “young physicians,” will continue to double-check our work, and those around us will wonder if we have done so.
Illuminating the lengthy path it takes to become a physician, a colleague jokingly replies, when asked the age question,
“Let’s see… 4 years of college, 4 years of medical school, and 3 years of residency, so I’m at least 11 years old.”
I pose the following question for our readers: How often, when boarding a plane, do we demand that the cockpit doors be opened so we can inquire about the pilots’ age? We don’t. We trust that they have enough knowledge and experience to competently fly hundreds of people to their destination. Isn’t it time we afford the same trust to all of our physicians, regardless of their age?