March 2nd, 2015
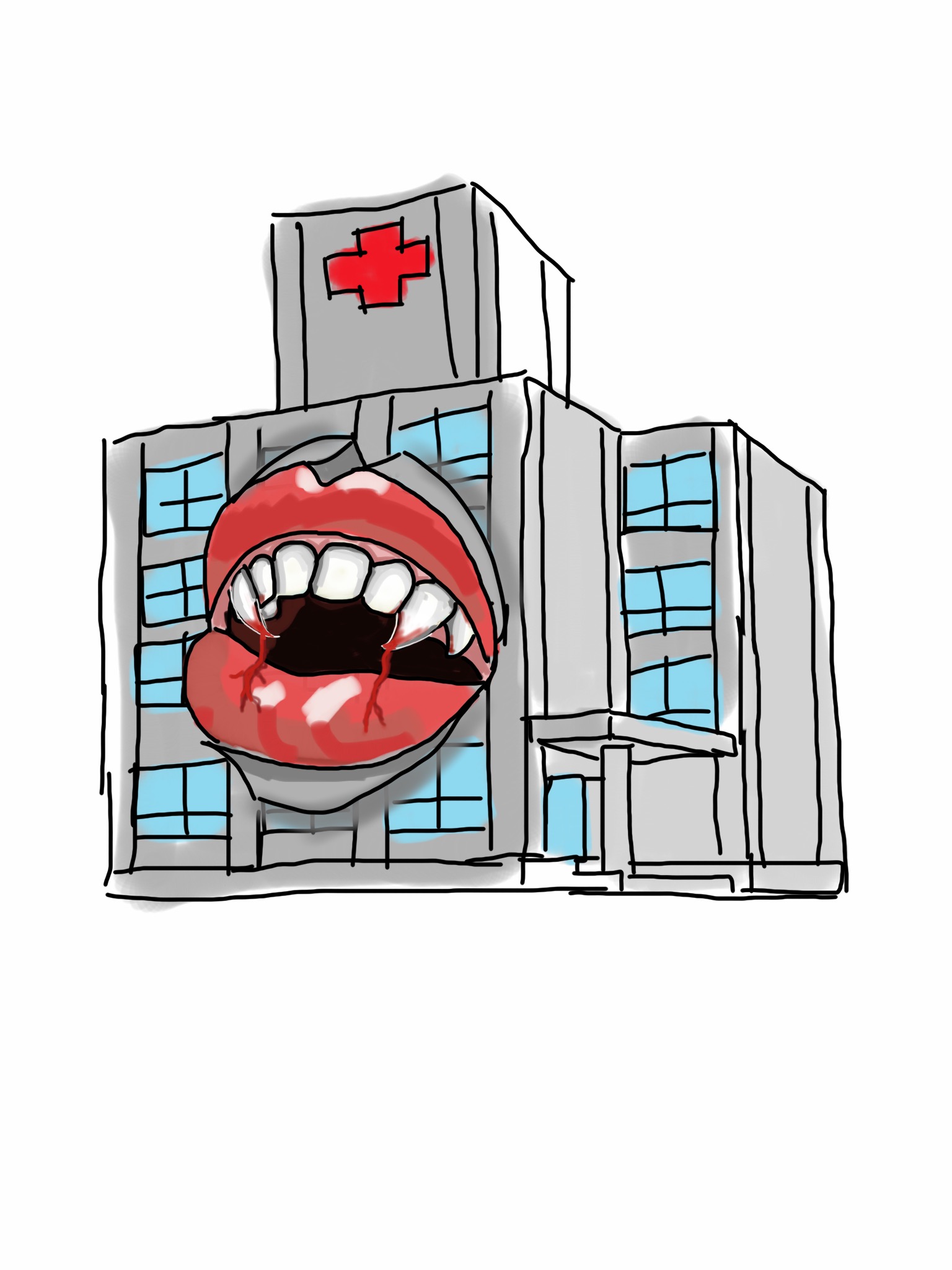
Hospitals, Like Vampires, Want Your Blood
Larry Husten, PHD
Anyone who has been in the hospital, either as a patient or a healthcare provider, is keenly aware that hospitals perform a lot of tests. It has even been suggested that some of those tests may not be necessary. Now a new study published in the Annals of Thoracic Surgery sheds light on just how excessive some of this testing can be.
Researchers analyzed records from 1,894 patients who had cardiac surgery at the Cleveland Clinic and calculated the frequency and total volume of blood drawn from their subjects. They wrote that they “were astonished by the extent of bloodletting” they discovered.
They reported the patients they studied were subjected to 221,498 laboratory tests, which averaged out to 115 tests per patient. Forty percent of the tests measured arterial or venous blood gas levels, 18% assessed blood coagulation, 14% were for a complete blood count (CBC), and 13% were for metabolic panels.
The cumulative median volume of blood was 454 mL per patient, which “is roughly equivalent to 1 to 2 cans of soda,” said the first author of the paper, Dr. Colleen Koch, who recently left the Cleveland Clinic to become the chair of the department of anesthesiology and critical care medicine at Johns Hopkins. Patients in the highest quartile of volume lost nearly a full liter of blood. The volume of blood drawn was much higher while the patients were in the cardiovascular ICU (332 mL) than when they were on the regular hospital floor (118 mL).
“Bloodletting to such an extent has consequences,” wrote the authors. Hospital-acquired anemia often results in the need for red blood cell transfusions, they note. In an email interview, Dr. Koch noted that higher phlebotomy volume increases the likelihood of hospital-acquired anemia, and patients with hospital-acquired anemia have worse outcomes.
In an invited commentary, Dr. Milo Engoren, an anesthesiologist at the University of Michigan, expressed shock at the finding. His remarks begin with a simple “Wow!” He continues: “we also need to step back and ask, ‘Does this patient need this test?’ Are we getting the test because the answer will change therapy? Or are we getting the test from habit or other inappropriate reason? Avoiding unnecessary blood tests will not only help prevent anemia (and maybe transfusion) but will also save money.”
Commenting on the study, Yale University cardiologist Harlan Krumholz said that the study shows “another facet of how hospitals can be toxic rather than healing. Is there really a need to drain patients of so much blood? Surely, this is an area where we can decrease the harm of being in the hospital.”
Dr. Matthew Sparks, a nephrologist at Duke University, said that this is “a common problem” and “a difficult habit to break.” But, he notes, “the culture needs to be stopped. The cardiovascular ICU however, is a place where things are dynamic and changing quickly. So I am not surprised they draw so many labs. However, when you see the quantified effect it really makes you take a step back and question the harm from so much blood loss.”
February 26th, 2015
Exploring Sex Differences in the Use of Mechanical Circulatory Support for Advanced Heart Failure
Jennifer Cook, MD
The CardioExchange Editors interviewed Jennifer L. Cook, lead author of an article in Circulation: Cardiovascular Quality and Outcomes from the genVAD Working Group. The article reviews the evidence on why fewer women than men receive mechanical circulatory support (with a ventricular assist device) for advanced heart failure.
Editors: Why are there differences in utilization of mechanical support between men and women?
Cook: Although the incidence of heart failure is similar in men and women, women are more likely to die from it. Nevertheless, a common misperception persists that men are at greater risk. Although advanced therapies such as mechanical support are as effective in women as in men, women are less likely to receive mechanical support. In clinical trials investigating mechanical support as a bridge to transplantation, fewer than 30% of patients were women. In trials investigating mechanical support for patients ineligible for heart transplantation, even fewer were women: <20%.
Editors: What can we do to address these differences?
Cook: It has been shown that women with heart failure are more likely to remain under the care of a primary physician instead of being referred for specialized cardiovascular care. The explanation for this pattern is not understood. It is important to raise awareness and emphasize the high risk for heart failure–related mortality among women. Once referred for specialized heart failure care, women face barriers to mechanical support. Investigation among mechanical support patients has not been done; however, in the heart transplant population, it is known that women frequently opt out of advanced surgical therapy. This warrants investigation, as unmet educational and psychosocial needs are likely to exist in this population.
Editors: Tell us about the role of the genVAD group and its long-term goals.
Cook: The genVAD working group came together because several of us believed that questions regarding sex-specific differences in treating patients with advanced heart failure have yet to be answered. The group includes investigators who represent diverse perspectives in advanced heart failure and mechanical support has the following goals: to raise awareness of the high-risk profile in women, to address barriers to consideration of mechanical support, to advance scientific knowledge about sex differences, and ultimately to improve access to care and clinical outcomes among women.
JOIN THE DISCUSSION
Share your perspective on Dr. Cook’s discussion of the work of the genVAD group.
February 24th, 2015
Increased Risk with NSAIDs Following Myocardial Infarction
Larry Husten, PHD
The cardiovascular safety of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and diclofenac has been the subject of considerable uncertainty and controversy. Now a new study published in JAMA raises specific concerns about the safety of these drugs in the highly vulnerable population of people who have had a recent myocardial infarction.
Using data from several linked national registries, Danish researchers studied over 60,000 people with a first MI, a third of whom received a prescription for an NSAID following discharge. Overall, people who took NSAIDs had double the rate of bleeding events as people not taking the drugs. In particular, people taking standard dual antiplatelet therapy with aspirin and clopidogrel had 3.3 bleeding events per 100 person-years; the addition of an NSAID increased this risk to 7.6 events per 100 person-years. The rate of cardiovascular events (including CV death, recurrent MI, ischemic stroke, or systemic arterial emboli) was also increased by the addition of an NSAID to other drugs.
A significant increase in risk was found for both the selective COX-2 inhibitors rofecoxib and celecoxib and nonselective COX inhibitors like ibuprofen and diclofenac. Further, an increased bleeding risk was found even when NSAIDs were used for just 3 days or fewer.
The authors note that although European and US guidelines and regulatory agencies discourage the use of NSAIDs in people with established heart disease, the use of these drugs in this population remains common and the drugs are often available over-the-counter.
In an accompanying editorial, Charles Campbell and David Moliterno write that the study adds to the available evidence that “while NSAIDs can be helpful and at times necessary medications for satisfactory quality of life, use of these medications among patients with a history of a recent MI is likely to be associated with clinically meaningful bleeding and ischemic risks.” Until PRECISION, a randomized controlled trial testing NSAIDS in people with or at high risk for CV disease is completed, “practitioners would do well to advise patients with cardiovascular disease against all NSAID use (except low-dose aspirin), especially patients with a recent acute coronary syndrome.”
Commenting on the study, Peter Berger said that although “registry analyses like these are associated with confounding that is usually impossible to overcome with any methods of adjustment,” unless there are better data from clinical trials, “the use of NSAIDs should be discouraged unless absolutely necessary.” Sanjay Kaul agreed, noting that this “observational study falls within the range of uncertain reliability,” but that until better evidence becomes available “clinicians should exercise caution in prescribing these drugs” after a recent cardiovascular event.
February 23rd, 2015
Want to Blog for CardioExchange at ACC.15?
Harlan M. Krumholz, MD, SM and John Ryan, MD
CardioExchange editors Harlan Krumholz and John Ryan are looking for members to blog for CardioExchange at the American College of Cardiology’s Annual Scientific Sessions from March 14th through the 16th in San Diego, CA.
If you are interested in blogging, please contact us. We look forward to hearing from you!
February 23rd, 2015
Selections from Richard Lehman’s Literature Review: February 23rd
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
JAMA 17 Feb 2015 Vol 313
Association Between the Use of Fondaparinux vs Low-Molecular-Weight Heparin and Clinical Outcomes in Patients With Non–ST-Segment Elevation Myocardial Infarction (pg. 707): I like it when large observational datasets confirm that what happened in randomized controlled trials actually happens in the hurly-burly of real life practice. The Swedish web system for enhancement and development of evidence based care in heart disease evaluated according to recommended therapies (SWEDEHEART—love it—I shall seek out a swede that is shaped like a heart) registry holds records from 40 616 consecutive patients with NSTEMI who received fondaparinux or low molecular weight heparin between September 1, 2006, through June 30, 2010, with the last follow-up on December 31, 2010. And just as in the OASIS-5 trial, “fondaparinux was associated with lower odds than LMWH of major bleeding events and death both in-hospital and up to 180 days afterward.”
JAMA Intern Med Feb 2015
Treatment With Multiple Blood Pressure Medications, Achieved Blood Pressure, and Mortality in Older Nursing Home Residents (OL): If you revisit John Yudkin’s Ten Commandments, you will see that the last of them reads “Honour thy elderly patient, for although this is where the greatest levels of risk reside, so do the greatest hazards of many treatments.” Here is a study to prove it. A total of 1127 women and men older than 80 years living in nursing homes in France and Italy were recruited, examined, and monitored for 2 years. Among these, people receiving two or more blood pressure lowering drugs and running systolic BPs of 130 and below were 80% more likely to die during the period of the study. Do not dishonour thy elderly patients by poisoning them with pointless and hazardous medication. And remember that people in nursing homes are at greatest risk, because they are constantly fed with medicines that they might otherwise forget to take, or have the good sense to stop taking.
February 23rd, 2015
Study Links Sauna Use to Better Health — In Finland
Larry Husten, PHD
Spending more time in the sauna may lead to a longer and healthier life — at least if you live in Finland, according to a new study published in JAMA Internal Medicine.
Finnish researchers analyzed data from the Kuopio Ischemic Heart Disease Risk Factor Study. The new analysis focused on 2,315 middle-aged men who had 1, 2-3, or 4-7 sauna bathing sessions per week. After 20 years of followup the rate of sudden cardiac death, fatal coronary heart disease, fatal cardiovascular disease, and all-cause mortality was significantly reduced in people who used the sauna more often.
For instance, when compared to men who had one session a week, the risk of sudden cardiac death was reduced by 22% in men with 2-3 sauna sessions each week and 63% lower in men with 4-7 sauna sessions each week. The overall pattern remained significant after adjusting for baseline differences in cardiovascular risk. In addition, the researchers found that longer sauna sessions were more beneficial than shorter sessions.
Franz Messerli thinks the health benefits of sauna bathing are plausible: “To prevent body over-heating during sauna bathing, cutaneous circulation increases drastically; there is maximal vasodilation. The fall in blood pressure is prevented by an increase in cardiac output mediated mostly by an increase in heart rate and by visceral vasoconstriction. Subsequent cooling in ice water, freezing air, or rolling in snow (as is traditional practice in Finland) causes immediate cutaneous vasoconstriction, which leads to a surge in blood pressure. The effects of both excessive heat and cold are mediated by the sympathetic nervous system. As a consequence, regular use of sauna blunts sympathetic stimulation and cardiovascular responses. The vascular tree is becoming progressively conditioned by rapidly alternating vasoconstriction and vasodilation, which may explain some of the cardiovascular benefits of frequent sauna bathing (and subsequent cooling).”
Some earlier studies have pointed to possible harmful effects of saunas. The researchers found no negative effects from increased sauna usage and speculated that may be due to unique features of Finnish saunas — including the combination of dry heat and high temperatures. They also noted that the benefits observed in the male Finnish population may not be applicable to women or in people not accustomed to regular sauna use. In response to a query, lead author of the study, Jari Laukkanen, said that because only 12 men in the study had no regular sauna use the researchers were unable to explore the comparison of sauna use versus no sauna use. “We investigated the dose of sauna,” he said. In addition, because sauna bathing is a lifetime activity in Finland, the study findings may not apply to people who take up sauna in middle age, for instance. “Further studies are needed to confirm our results in different population settings,” the researchers concluded.
The study “makes me wonder if we should all adopt the intensive sauna strategy — or whether that only works in a country like Finland where saunas are a part of life,” said Harlan Krumholz. “Seriously, it opens a lot of questions about whether such behavioral interventions can exert a positive effect on heart health. The first question for those of us in the U.S. is whether sauna versus no sauna is associated with risk reduction, a question they cannot answer in sauna-prevalent Finland.”
One conclusion seems clear to John Ryan: “Finland just seems like a great place to live,” he said. He also pointed out that in the 1970s Finland had the world’s highest rate of death from cardiovascular disease. This has now been reduced by 65% in men, but the role, if any, of sauna bathing in this major shift is unknown.
In an editor’s note, Rita Redberg would seem to agree with Ryan’s assessment of Finland. She writes that “although we do not know why the men who took saunas more frequently had greater longevity (whether it is the time spent in the hot room, the relaxation time, the leisure of a life that allows for more relaxation time, or the camaraderie of the sauna), clearly time spent in the sauna is time well spent.”
February 19th, 2015
Companies Plan To Resume Renal Denervation Trials
Larry Husten, PHD
Medtronic and Boston Scientific have announced plans to start phase 2 clinical trials this year for their updated renal denervation catheters. The once promising new technology is intended to treat hypertension unresponsive to drug therapy. The failure last year of Medtronic’s Symplicity HTN-3, the first large pivotal trial to rigorously test renal denervation, sent manufacturers back to their drawing boards to redesign the devices.
Earlier this week Medtronic disclosed in its quarterly report that it planned to soon submit to the FDA its application for an investigational device exemption (IDE) for its next-generation renal denervation device. The spiral-shaped device has multiple electrodes and is designed to achieve more comprehensive ablation of the renal arteries. The company is seeking FDA approval to proceed with a phase II trial.
In its quarterly report Boston Scientific said it plans to begin enrolling patients in the first half of this year in a phase II trial, called REDUCE-HTN REINFORCE, testing its Vessix platform. The company has not yet released details of the protocol but said the FDA has approved the protocol.
February 19th, 2015
A Close Examination of Recent Studies of Endovascular Treatment for Acute Ischemic Stroke
Rory J Spiegel, MD
CardioExchange welcomes this guest post from Dr. Rory Spiegel, who is a third-year and chief Emergency Medicine resident at Newark Beth Israel Medical Center. This piece originally appeared on his blog, EM Nerd.
For those whose beliefs are already firmly in favor of endovascular therapy for acute ischemic stroke, the publication of the MR CLEAN trial earlier this year and, more recently, the EXTEND-IA and ESCAPE trials only serve as a big fat, “I TOLD YOU SO!” For the perpetual disbelievers, each of these trials possesses enough flaws to discredit their findings. For the appropriately skeptical among us, though these trials initially appear to discredit our well-meaning rants, on closer examination they are far more validating.
Earlier this year the publication of a large, well done, RCT examining the use of endovascular treatment for acute ischemic stroke threatened to drastically change the acute management of CVA as we know it. And though this trial was given a most unfortunate name (MR CLEAN), it marked the first time endovascular therapy has demonstrated any clinically relevant benefit. We have discussed this trial in depth in two previous posts over at my blog and once here at CardioExchange. While MR CLEAN’s results were promising, there were many reasons why they should be viewed with a healthy dose of skepticism. Before we commit to a resource-heavy intervention like that of endovascular therapy, more studies validating these findings are required. Since the publication of MR CLEAN, two active trials were stopped early for benefit, seeming to be the very validation for which we asked. The results of both of these studies, EXTEND-IA and ESCAPE, were recently published in the NEJM.
The first trial, Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra-Arterial (EXTEND-IA) trial, by Campbell et al, is a multi-center RCT that examines the efficacy of endovascular treatment in patients with CVA whose symptoms began within 4.5 hours of randomization. Like MR CLEAN, this trial was a stunning success. In fact, its results far outpaced the, by comparison, paltry benefits found in MR CLEAN. EXTEND-IA was stopped early after enrolling 70 patients for overwhelming benefit. The rate of significant improvement after three days (reduction in NIHSS > 8) was 80% vs. 37% in the endovascular group and control group, respectively. Likewise, the rate of favorable outcome at 90 days (mRS of 0-2) was 71% vs. 40%, respectively, boasting an absolute difference of 31%.
The second and far more statistically robust trial is the Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trial, published by Goyal et al. In this trial, authors examined patients up to 12 hours after symptom onset (though the large majority of the patients enrolled were evaluated within three hours of symptom onset). Like EXTEND-IA, the ESCAPE trial was an overwhelming success. Authors randomized 316 patients to either standard care or standard care plus endovascular therapy. Like EXTEND-IA, the authors found overwhelming benefits of the endovascular therapy. The rate of functional independence at 90 days (mRS of 0-2) was 53.0% vs. 29.3% in favor of the endovascular arm, with authors noting a 33.7% absolute increase in positive outcomes in patients who received endovascular therapy. For the first time in the history of reperfusion therapies for acute ischemic stroke, a clinically significant mortality benefit was demonstrated. Ninety-day mortality was 10.4% in the endovascular group compared to 19.0% in the control group. Not to mention the surprisingly low rate of intracranial hemorrhage, (3.6% vs. 2.7%).
Neither trial is definitive in its own right. The EXTEND-IA cohort only examined the efficacy of endovascular therapy in 70 patients. This trial originally planned to enroll 100 patients, but after an interim analysis demonstrated such impressive results, the trial was stopped prematurely. Frustratingly, this premature investigation of the sealed data was not performed because of a pre-planned interim analysis, but rather the data were explored because of the publication of MR CLEAN. Though the remaining 30 patients would have most likely not altered the results, we cannot view this poorly powered trial as anything more than hypothesis building. In isolation, EXTEND-IA can only offer a guideline for the future of endovascular management in acute ischemic stroke. Even the authors themselves conceded this point in the statistical analysis plan they published in January 2014, in which they clearly defined EXTEND-IA as a phase II trial. A definition that is conveniently left out of the formal publication in the NEJM, an oversight possibly induced by the unexpected magnitude of their success, causing well-deserved delusions of grandeur.
ESCAPE, though far more statistically hardy than EXTEND-IA, is still a rather small cohort, and suffers from the same unfortunate biases. Originally intending to enroll 500 patients, the authors called for an early stoppage prior to their planned interim analysis, again because of the results of MR CLEAN. Although the sample size of 316 patients lends a stronger validity than the 70 patients examined in the EXTEND-IA cohort, the early stoppage prevents us from confidently assessing the true effect size this treatment may provide. Interestingly, when implementing this unplanned analysis, the authors utilized a dichotomous outcome comparing the mRS scale of patients alive and independent (mRS of 0-2) at 90 days rather than the ordinal analysis they had originally chosen and utilized as their primary outcome when performing the power calculation. The ordinal scale has recently gained favor as an outcome measure in stroke trials because of its ability to augment the p-value and turn otherwise negative trials into statistical successes. Conversely, it is almost impossible to determine the clinical relevance of the odds ratio it produces. Given the impressive benefits of both trials, the small statistical augmentations offered by ordinal analysis are irrelevant. As such, the authors of both trials favored the more traditional dichotomous outcome. The 33.7% absolute difference measured by the dichotomous scale in the ESCAPE trial appears far more impressive than an odds ratio of 2.6 offered by ordinal analysis.
When viewed in series with MR CLEAN it is hard to deny the efficacy of endovascular therapy. With the overwhelming success of both EXTEND-IA and ESCAPE, the MR CLEAN data appear almost lacking. In the MR CLEAN cohort, patients randomized to receive endovascular therapy had a 14% absolute benefit over those in the control group. It is safe to say neither group did all that well, with the amount of patients alive and independent at 90 days reported as 33% and 19%, respectively. The EXTEND-IA and ESCAPE cohorts, however, did exponentially better (71% vs. 41% and 53.0% vs. 29.3%, respectively). Are we truly looking at the same patients as were examined in MR CLEAN or do the EXTEND-IA and ESCAPE cohorts represent a completely different population?
It should come as no surprise that both the EXTEND-IA and ESCAPE cohorts included vastly different patients than those enrolled in MR CLEAN. In MR CLEAN, to be eligible for inclusion patients were required to have an occlusion of distal intracranial carotid artery or middle cerebral artery (M1, M2) or anterior cerebral artery (A1) as identified by CT angiography, magnetic resonance angiography, or digital subtraction angiography. Both EXTEND-IA and ESCAPE had far stricter inclusion restrictions. Patients who were enrolled in the EXTEND-IA cohort needed to demonstrate an ischemic penumbra on perfusion imaging with a small infarcted core. Though slightly different criteria were utilized, like EXTEND-IA, the ESCAPE cohort used CT angiographic imaging to identify patients with small infarcted cores and large areas of salvageable tissue. These inclusion criteria significantly narrowed the subset of stroke patients examined. These differences in patient selection are not only responsible for the almost unbelievable efficacy demonstrated in both of the EXTEND-IA and ESCAPE trials, they mark the first time that imaging criteria was successfully used to identify a cohort of stoke patients who may benefit from reperfusion therapy.
There has been a long history of failure in the use of perfusion imaging for the management of acute ischemic stroke. Early studies investigating the use of diffusion weighted MRI to identify potentially salvageable ischemic brain failed to show benefit (1, 2, 3, 4, 5). These failures may, in part, be due to the industry bias of only enrolling patients presenting >3 hours after onset in the hopes of extending their FDA-approved treatment window and, more importantly, their profits. Though each of these trials showed promising rates of reperfusion, the consistently high rates of intracranial hemorrhage overshadowed the minimal benefits. The MR RESCUE trial, published in NEJM in February 2013, was the first to utilize this technology to identify potential candidates for endovascular therapy. Again, this trial failed to demonstrate that patients with ischemic penumbrae benefited from revascularization. However, this may have been due more to the trial’s flawed design than the technology’s deficiencies. The authors of MR RESCUE only enrolled patients after initial IV tPA failure. In contrast to these historical failures, both the EXTEND-IA and ESCAPE cohorts, unencumbered by fears of disproving tPA’s early successes, aggressively pursued reperfusion therapy after salvageable tissue was identified on CT imaging. In doing so, these trials have, for the first time, identified the population that will preferentially benefit from reperfusion therapy.
At the risk of sounding optimistic, both EXTEND-IA and ESCAPE are impressively positive trials. Although small and methodologically flawed, with likely exaggerated effect sizes, when viewed in concert with MR CLEAN, these trials present endovascular therapy in a promising light. For some time now legitimate cries for more data regarding tPA’s safety and efficacy in acute ischemic stroke management have been disregarded and marginalized. The almost fanatical acceptance was based around the success of a single small cohort of patients treated in under 3 hours after symptoms onset. Despite the many methodogical flaws possessed by the NINDS trial, its results were never duplicated because of the pharmaceutical industry’s fear of losing the tenuous ground they had gained. Although there are significant harms associated with the administration of tPA, the literature has consistently suggested that there is a subset of patients who will benefit from its administration. Rather than working to identify this narrow population, we have witnessed an industry-driven effort to expand the indications for reperfusion therapy.
EXTEND-IA and ESCAPE have identified potential cohorts of patients who will likely benefit from reperfusion therapy. If these results can be confirmed, no longer will we be forced to use the blunt tool of perceived time from symptom onset to determine which patients are eligible for treatment. These trials should inspire us to not only explore the successful utilization of endovascular therapy, but also re-examine the harmful practice of thrombolytic therapy that we currently employ.
Additional Sources Cited:
February 16th, 2015
Cardiovascular Risk Calculators Overestimate
Larry Husten, PHD
Calculating cardiovascular risk has become a central and highly controversial component of cardiovascular guidelines. Now a study in the Annals of Internal Medicine finds that most of the commonly employed tools seriously overestimate the risk of people today.
Researchers used data from 4,227 people enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) between 2000 and 2002 to assess the predictive accuracy of the new AHA/ACC atherosclerotic cardiovascular disease (ASCVD) tool and four alternative risk scores: FRS-CHD, the ATP-III-FRS-CHD, the Reynolds Risk Score (RRS), and the FRS-CVD.
They found that four out of the five scores overestimated risk for men by as little as 37% and by as much as 154% and for women by as little as 8% and as much as 67%. The RRS (Reynolds Risk Score) overestimated risk in men by 9% but underestimated risk in women by 21%.
Current AHA-ACC guidelines recommend that statin therapy should be considered for adults with a 10-year risk greater than 7.5%. But the researchers found that the actual event rate was only 3% in men and 5.1% in women among people with an AHA-ACC-ASCVD risk score of 7.5%-10%. Additional analyses found that this discrepancy was not explained by higher than expected use of aspirin, statins, or blood pressure drugs.
The authors noted that the cohorts used to develop the risk scores are “decades old” and quite different from “the more modern MESA cohort.” The implications of the findings are not just academic. “Overestimation of risk,” the authors write, “would likely result in increased use of preventive medications, potentially exposing some patients to the unnecessary risks of these drugs. In particular, aspirin use in primary prevention is known to be a delicate balance between cardiovascular risk reduction and increased incidence of bleeding.” In addition, they note, “overestimation of risk has implications for public health planning with accompanying financial ramifications for a heavily burdened health care system.”
In an accompanying editorial, Paul Ridker and Nancy Cook write that the study “serves as a crucial test of external validation and demands the attention of both clinicians and policymakers.”
Speaking on behalf of the AHA, David Goff pointed out two significant reasons that may explain in part why the AHA risk calculator overestimates events in the MESA cohort. First is the inclusion of data from the lower-risk Chinese-American and Hispanic-American participants. These data had been excluded from the AHA’s analysis and, for this reason, the new guidelines include a caution about using the calculator in this population. Second, said Goff, the AHA equations are meant to be used in untreated people but over 80% of the MESA cohort received some sort of preventive treatment during the study period. Although the Annals investigators sought to correct for this, Goff said that it is extremely difficult to fully take into account the downstream effect of treatment.
Finally, Goff emphasized that although “there’s been a lot of attention paid to just exactly how well these equations work” we shouldn’t “lose sight of our goal” of reducing the burden of cardiovascular disease. “It’s really important not to let the perfect become the enemy of the good,” he said.