August 15th, 2013
Fuster to Succeed DeMaria as Editor of JACC
Larry Husten, PHD
The American College of Cardiology (ACC) has announced that Valentin Fuster will be the next editor-in-chief of the Journal of the American College of Cardiology (JACC). Fuster will succeed the current editor, Anthony DeMaria, beginning in 2014.
 “JACC has long been committed to bringing the newest and most innovative research to cardiovascular professionals, and Dr. Fuster brings unmatched prestige and expertise to the role of editor and we trust he will continue and expand on this tradition,” said ACC President John G. Harold, in a press release.
“JACC has long been committed to bringing the newest and most innovative research to cardiovascular professionals, and Dr. Fuster brings unmatched prestige and expertise to the role of editor and we trust he will continue and expand on this tradition,” said ACC President John G. Harold, in a press release.
Fuster has long been one of the most influential figures in cardiology. He is probably best known for his pioneering research demonstrating the concept of “vulnerable plaque,” but he has been involved in many of the major developments in cardiology in recent decades.
Fuster has been the recipient of seemingly innumerable honors and awards. A former president of the American Heart Association, he is the physician-in-chief at The Mount Sinai Medical Center in New York and also serves as the director of the Zena and Michael A. Wiener Cardiovascular Institute and the Marie-Josée and Henry R. Kravis Center for Cardiovascular Health at Mount Sinai. Most recently he was the principal investigator of the influential FREEDOM trial. Fuster was born in Barcelona, Spain in 1943. JACC is published by Elsevier.
August 14th, 2013
Advanced Lipoprotein Analysis: Time for Widespread Implementation?
Behnood Bikdeli, M.D.
Traditional LDL- and HDL-cholesterol measurements fall short of perfect prediction of cardiovascular risk. So, several academic and industry investigators have tried to identify supplementary advanced lipoprotein tests that can, at least in part, detect the “residual risk.” These include not only measurements of apolipoprotein B and A-I subcomponents, but also assays that identify LDL particles and their size. Accordingly, advanced lipoprotein analysis has garnered much attention during the past decade, and clinicians continue to wonder where and when they should request such analyses, if at all.
Results from existing studies vary to some degree (see Parish et al.), but several suggest that LDL particle number (LDL-P) might outperform LDL cholesterol (LDL-C) as a predictor of cardiovascular risk (see Greenland et al. and Otvos et al.). For example, in a substudy of the Multi-Ethnic Study of Atherosclerosis (MESA) cohort, although both LDL-C and LDL-P were associated with risk for incident cardiovascular disease, only LDL-P predicted incident CVD among people with discordant LDL-C and LDL-P. Given that evidence and assuming that advanced lipoprotein analysis would help to identify a larger group of at-risk patients, several insurance companies have agreed to pay for such tests. But does this additional information actually improve clinical outcomes?
Any recently introduced test has its proponents and critics, but the ultimate clinical value of the test’s results depends on the availability of high-quality evidence to guide practice. Some of the new cardiac biomarkers have recently been used as criteria for including patients in cardiovascular trials or for guiding management. Among those, perhaps use of D-dimer in algorithms to diagnose venous thromboembolism is the most well-known example of a widely available biomarker that has supportive evidence from multiple studies.
Advanced lipoprotein testing may ultimately prove helpful for appropriate risk stratification and guidance of therapy to improve outcomes. As a fan of tailored and “personalized” medicine, I would like to see this happen soon. However, for now, there is a dearth of evidence on clinically proven interventions that specifically target the increased risk identified by such advanced techniques. Therefore, conducting high-quality randomized controlled trials might be a prerequisite to widespread use of these tests.
In this era of a focus on real value to patients, I wonder if advocating for tests that have yet to make a difference to our patients is the best approach. Should insurers be paying for these tests? Please share your thoughts with me and with others here on CardioExchange.
August 13th, 2013
Observational Study Lends Support to CRT Guidelines
Larry Husten, PHD
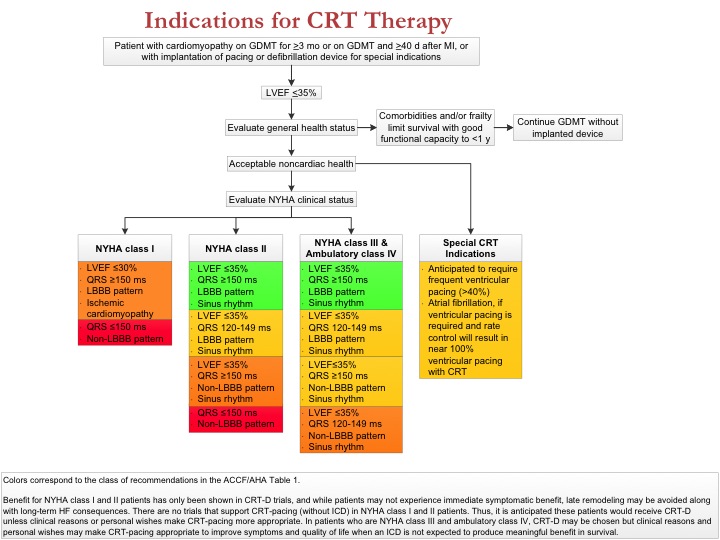
A large observational study published in JAMA suggests that patients with left bundle-branch block (LBBB) and longer QRS duration derive the most benefit from a cardiac resynchronization therapy defibrillator (CRT-D). The findings appear to support current, but often criticized, guidelines from the American College of Cardiology, American Heart Association, and the Heart Rhythm Society, in which a class I recommendation is restricted to patients with LBBB and QRS duration of 150 ms or greater.
Pamela Peterson and colleagues analyzed data from more than 24,000 CRT-D patients who were enrolled in the National Cardiovascular Data Registry’s ICD Registry. For the entire group, all-cause mortality was 9.2% at 1 year and 25.9% at 3 years. Hospital readmission occurred in 10.2% at 30 days and 43.3% at 1 year. Mortality and readmission rates, both before and after adjusting for other risk factors, were significantly higher in the group without LBBB and with QRS duration <150 ms.
In their report, the authors noted that their study did not contain a control group that did not receive CRT therapy and “should not lead to conclusions regarding the benefit of CRT, or the lack thereof, in patients with QRS duration of 120 to 149 ms and without LBBB.” But, they wrote, “the findings that patients with LBBB and QRS duration of 150 ms or greater had the best outcomes after accounting for differences in other measured patient characteristics are concordant with current guideline recommendation classifications.” They concluded that their findings “support the use of QRS morphology and duration to help identify patients who will have the greatest benefit from CRT-D implantation.”
August 12th, 2013
Selections from Richard Lehman’s Literature Review: August 12th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
Lancet 10 Aug 2013 Vol 382
BP Targets in Patients with Recent Lacunar Stroke (pg. 507): “Small subcortical brain infarcts, commonly known as lacunar strokes, comprise about 25% of ischaemic strokes. Most result from disease of the small penetrating arteries.” The SP3 trial looked at the effect of blood pressure lowering to a systolic blood pressure target above or below 130 in this specific type of stroke. There was no significant difference in outcomes. Nonetheless, the authors hold to the principle “the lower the better” because for recurrent stroke and cardiovascular death the trend was towards reduction, and “treatment-related serious adverse events were infrequent.” I can go with this so far, but when you are talking about giving stroke patients lifelong medication on the basis of numbers-needed-to-treat which are incalculably large, even non-serious adverse effects such as tiredness, cough, polyuria and dizziness on getting up are hard to justify. Treat the patient, not the target.
Effectiveness of Intermittent Pneumatic Compression in Reduction of Risk of DVT in Patients Who have had a Stroke (pg. 516): CLOTS 3 is the acronym of a trial of intermittent pneumatic compression to reduce DVT on patients immobilized by stroke. If you try really hard you can extract these letters from “Clots in Legs Or sTockings after Stroke.” Going by initials, that should really be CILOSAS; but enough of acronyms, which provide innocent fun for researchers in the hope that they will help readers remember the trial. Preventing DVT after severe stroke is probably worthwhile, and these inflating stockings do reduce venous clots by about a third. The median age of the patients was 76, and a lot of them died: 33 fewer in the intervention group, which was not statistically significant given the large size of this UK trial.
BMJ 10 Aug 2013 Vol 347
Effect of Telephone Health Coaching on Hospital Use and Associated Costs: “2698 patients (were) recruited from local general practices before 2009 with heart failure, coronary heart disease, diabetes, or chronic obstructive pulmonary disease; and a history of inpatient or outpatient hospital use.” They were then individually randomized to usual care or “telephone health coaching (which) involved a personalised care plan and a series of outbound calls usually scheduled monthly.” The aim was to reduce hospital admissions. The result was to increase them. Since then, the most popular research idea seems to be to hand out iPads for education and monitoring to reduce admissions for chronic disease. Will this have any effect? Yes, I think it will increase disease awareness, anxiety, and iPad ownership.
August 11th, 2013
Radiation Exposure in the Cath Lab: A Radioactive Topic?
Reza Fazel, MD, MSc
In 2009, I published an article in the NEJM with my friend and mentor, Brahmajee Nallamothu, and several other colleagues. It documented rates of radiation exposure from medical imaging. As I worked on the paper, I learned that many clinicians, including radiologists, consider their training in this area to be inadequate, focusing more on technical intricacies than on identifying which patients are at greatest risk for exposure from ionizing radiation and on strategies to minimize that risk. Cardiovascular imaging, in particular, is responsible for a significant proportion of all medical radiation exposure, yet cardiologists are taught very little about it. So I have become interested in increasing awareness of radiation safety among clinicians in general and cardiologists specifically, especially interventionalists (I am about to start an interventional cardiology fellowship).
The good news is that awareness of radiation exposure from cardiac CT and nuclear imaging has increased in the past few years. The bad news is that the topic remains much less visible for fluoroscopic procedures. Until recently, the only available U.S. benchmark data for radiation doses in interventional cardiology procedures were derived from a Nationwide Evaluation of X-ray Trends (NEXT) survey, a study with a relatively small sample size (n=2407) that did not account for procedure complexity.
Our group has now used data from the CathPCI Registry to define determinants of fluoroscopy time for invasive cardiac angiography (ICA) and percutaneous coronary intervention (PCI). This study, published in Catheterization and Cardiovascular Interventions, describes the distributions of fluoroscopy times for ICA and PCI in more than 3 million procedures. Here are our key findings of interest to clinicians:
1. We described distributions of fluoroscopy time for each ICA and PCI — and also evaluated the incremental fluoroscopy time associated with important patient, procedure, operator, and hospital characteristics. This work finally gives catheterization labs a benchmark to assess how they are performing relative to a national, complexity-adjusted average.
2. Most of the variation in fluoroscopy time was related to “fixed” patient- and procedure-related factors. This sets a floor for how much improvement we can expect from quality efforts. However, about 20% of this variation was related to potentially modifiable operator and hospital-level factors. Not surprisingly, operator volume was inversely associated with fluoroscopy time for both ICA and PCI, as was being at a university hospital. These factors present some challenges, given the essential need to minimize patient harm while training the next generation of interventional cardiologists.
3. My interactions with fellow invasive cardiologists suggest to me that relatively few of them are familiar with the preferred dose metrics for fluoroscopic radiation exposure: (A) total air kerma at the reference point (a measure of peak skin dose); and (B) air kerma-area product (a measure of total radiation exposure and risk to the patient). It is not surprising, then, that interventionalists don’t routinely track these metrics during procedures, even though all fluoroscopy machines manufactured since 2006 display them in real time (to comply with FDA regulations). It is our hope that this paper will encourage operators to learn more about these metrics and to start routinely monitoring them during procedures.
I would like to invite fellow clinicians, especially interventional cardiologists and medical physicists, to read the paper and share their thoughts. In particular, we provide a table of techniques (reproduced below) that have been recommended by regulatory authorities. I’m curious to hear how often you observe these techniques being used in daily practice. I’ve come to realize that radiation exposure is a “silent danger” that is difficult for individual clinicians to quantify and address on their own.
TABLE
| Fluoroscopic Dose-Rate Management Techniques* |
*adapted from NCRP-168 and ICRP Draft Report for Consultation on Patient and Staff Radiological Protection in Cardiology |
August 9th, 2013
The Guidelines are Dead. Long Live the Guidelines.
Larry Husten, PHD
Following the recent surprising announcement that the National Heart, Lung, and Blood Institute would no longer issue guidelines, leaders of the American Heart Association (AHA) and the American College of Cardiology (ACC) have now announced that are “officially assuming the joint governance, management and public distribution” of the enormously influential cardiovascular prevention guidelines, including the much-delayed and much-anticipated hypertension and cholesterol guidelines (formerly known as JNC 8 and ATP IV). The ACC and AHA will also assume responsibility for guidelines on cardiovascular risk assessment, cardiovascular lifestyle interventions, and obesity.
In an editorial published in Circulation and the Journal of the American College of Cardiology, leaders of the NHLBI, AHA, and ACC provide a little more information on how the new model will work. One important announcement, that “all chairs and members of the current writing panels have been invited to continue to work together with the ACC and AHA to finalize the guidelines,” might indicate that the hypertension and cholesterol guidelines could see the light of day in the not-too-far-distant future. In June, the NHLBI’s Michael Lauer expressed confidence that these guidelines would appear in less than a year, but the AHA said that no timeline had yet been established.
More generally, the editorial states that the joint ACC/AHA Task Force on Practice Guidelines “will provide oversight and staff support, with NHLBI supporting further systematic evidence review as needed.” In addition, other “stakeholder organizations” who had been involved in the NHLBI’s efforts “will also be engaged” in the new process, according to the editorial.
Prior to the NHLBI announcement in June, the fate of the hypertension and cholesterol guidelines, both of which had been delayed for many years, had been the subject of widespread rumor, frustration, and criticism. In the statement published in June on the NHLBI website, NHLBI director Garry Gibbons wrote that “the landscape for guidelines development has changed dramatically. More effective strategies and clinical evidence are available to clinicians and patients.” He cited two reports from the Institute of Medicine (IOM) “that established new ‘best practice’ standards for generating systematic evidence reviews and developing clinical practice guidelines. The reports underscore that these are two distinct, yet related, activities that require careful intersection and coordination.”
Some observers also believe that the backlash against the U.S. Preventive Services Task Force’s mammography guidelines prompted the NIH and public officials to avoid making controversial recommendations.
August 7th, 2013
FDA Panel Recommends Approval of New Pulmonary Hypertension Drug
Larry Husten, PHD
The FDA’s Cardiovascular and Renal Drugs Advisory Committee recommended approval for Bayer’s new pulmonary hypertension drug, riociguat. The committee voted 11-0 in favor of approving the drug for two forms of pulmonary hypertension: pulmonary arterial hypertension (PAH) and chronic thromboembolic pulmonary hypertension (CTPH).
Bayer proposed an initial dose of 1 mg three times daily and a maximum dose of 2.5 mg three times daily. Due to concerns about hypotension, FDA reviewers initially recommended that the drug not be approved at the 2.5-mg dose and instead recommended a starting dose of 0.5 mg. Ultimately, the panel decided to grant as many options as possible to physicians and recommended a starting dose of 0.5 mg and a maximum dose of 2.5 mg.
The panel meeting was largely devoted to two clinical trials, CHEST-1 and PATENT-1, whose findings were recently published in the New England Journal of Medicine. Both trials showed that patients taking riociguat had a modest improvement in their ability to walk.
CardioExchange’s John Ryan, an expert on pulmonary hypertension, sent the following comment:
The issue will be where PAH specialists feel this agent fits in their therapeutic options. It remains to be seen whether riociguat will become first line therapy and replace oral medicines that PAH doctors are familiar with, namely PDE5 Inhibitors and endothelin receptor antagonists, or if it will be additive on top of these agents. In PATENT-1, 50% of the patients were not taking other agents, so how they interact with each other is largely unknown.
August 6th, 2013
George W. Bush Gets Stent After Annual Examination
Larry Husten, PHD
Former U.S. President George W. Bush received a stent today at Texas Health Presbyterian Hospital. Here is the statement from Bush’s office:
During President George W. Bush’s annual physical examination at the Cooper Clinic in Dallas yesterday, a blockage was discovered in an artery in his heart. At the recommendation of his doctors, President Bush agreed to have a stent placed to open the blockage. The procedure was performed successfully this morning, without complication, at Texas Health Presbyterian Hospital. President Bush is in high spirits, eager to return home tomorrow and resume his normal schedule on Thursday. He is grateful to the skilled medical professionals who have cared for him. He thanks his family, friends, and fellow citizens for their prayers and well wishes. And he encourages us all to get our regular check-ups.
A Bush spokesman told USA Today that Bush had not had symptoms before the examination but that “the stent was necessary. His annual physical includes a stress test. EKG changes during the stress test yesterday prompted a CT angiogram, which confirmed a blockage that required opening.”
August 5th, 2013
Putting the 2013 Heart Failure Guidelines Into Practice
Clyde Yancy, MD, Harlan M. Krumholz, MD, SM and John Ryan, MD
CardioExchange’s Harlan Krumholz and John Ryan interview Clyde W. Yancy, lead member of the ACCF/AHA task force that wrote the 2013 guidelines for management of heart failure.
Krumholz and Ryan: What is the biggest challenge to implementing the heart failure guidelines for every patient with heart failure?
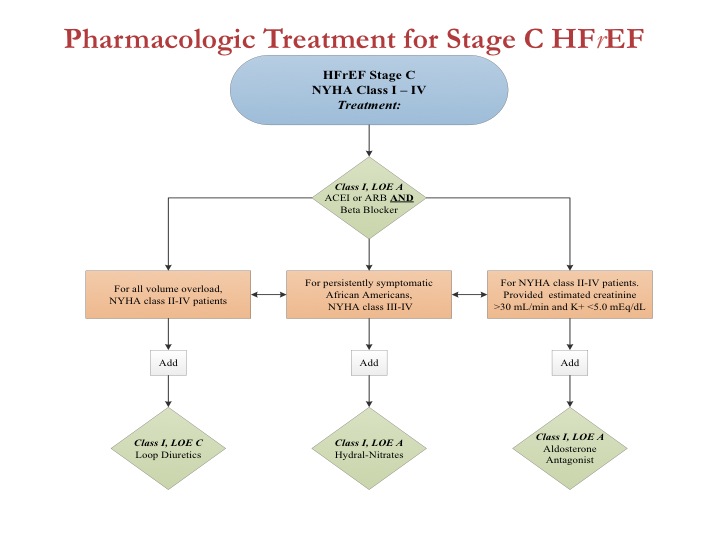
Yancy: The biggest challenge is no longer in establishing “proof.” The database we now have is robust, and the work that we and others have done make a compelling argument that guideline adherence works. Thus, the biggest challenge is operational — namely, how to make the information easier to deploy and access. The parent committee’s strategy is the concept of GDMT, or guideline-directed medical therapy. The goal is to use simple algorithms to clarify the best application of evidence-based, guideline-directed therapy for patients with cardiovascular disease, according to appropriate indications.
Figure 1 from the heart failure guidelines, shown here, is the linchpin of this effort. In a single graphic, we represent the best application of medical therapies for patients with heart failure and reduced left ventricular ejection fraction (HFrEF).
Click here to download PowerPoint slide
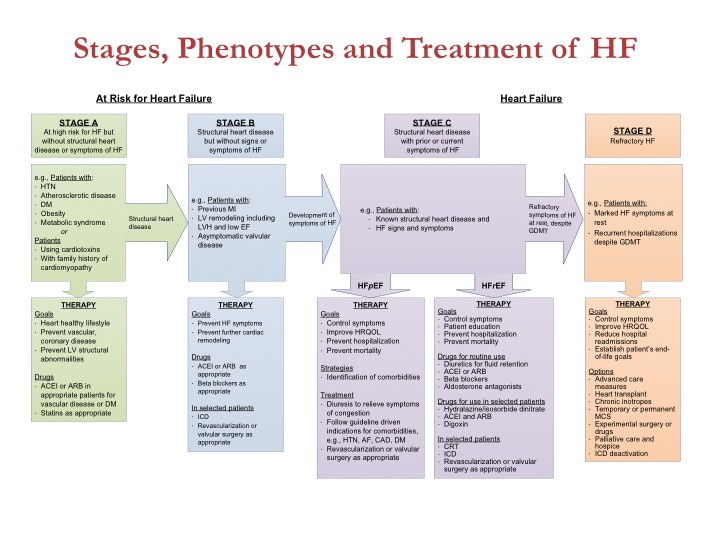
In addition, we have a similar graphic for device therapy and an expanded emphasis on HF with preserved left ventricular EF (HFpEF), including specific applicable guideline statements. If the deployment of GDMT works as intended, we will move closer to broad implementation of best therapies for HF.
Click here to download PowerPoint slide
Click here to download PowerPoint slide
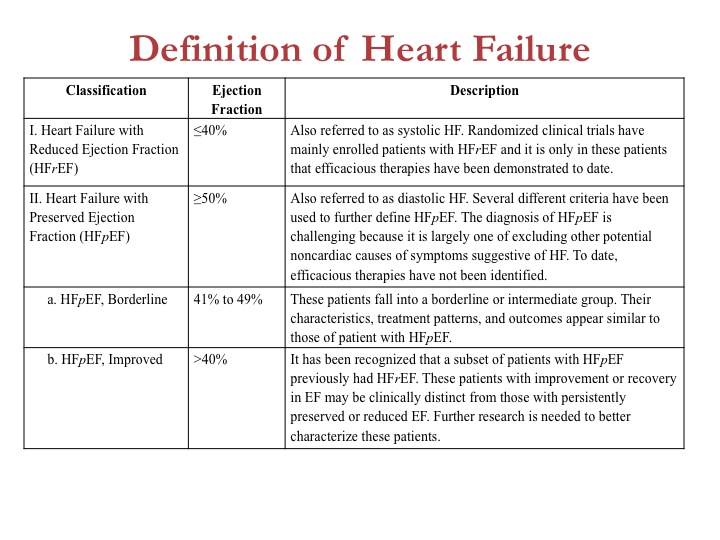
Krumholz and Ryan: Heart failure with preserved LVEF is now defined in categories: HFpEF (EF >50%); HFpEF, borderline (EF 41–49%); and HFpEF, improved (EF >40%). How often should patients undergo an echocardiogram to identify their HFpEF or HFrEF category? And should patients be managed according to their current EF or their worst historical EF?
Yancy: Great questions. We consider it important to identify the increasing number of patients formerly with HFrEF who have recovered sufficiently to now have an EF >40%. This group has not been well studied, but a good guideline document answers some questions and raises others. We hope that by defining these cohorts of HFpEF, we will spur investigators to study each subgroup.
Click here to download PowerPoint slide
Can we stop or reduce GDMT in patients who have recovered their ventricular function? If a device needs a generator change but the EF is now >35%, is the change still necessary? We don’t know the answers to those questions, but without making this distinction we would never pursue the answers. For now, as we say in Texas, “Dance with the horse that brought you to the party.” In other words, we don’t advise switching a regimen that appears to have promoted an improvement in ventricular function. And only check ventricular function when the clinical status has changed or an intervention intended to affect LV performance has been initiated.
Krumholz and Ryan: You acknowledge the increasing cost of treating patients with HF. How do you propose those costs be controlled, especially as use of mechanical circulatory support (LVADs) expands?
Yancy: So this is the tough question. As a guiding principle, the ACCF/AHA guidelines are written without regard to cost. That is less of a copout and more an acknowledgment that our database is surprisingly rudimentary regarding cost-effectiveness. We know more about the cost-effectiveness of LVADs than we do for sodium restriction or parenteral diuretics. But we do have a fairly strong gestalt sense that quality care, as driven by our guidelines, is cost-effective care, given that we put primacy on the preservation of life.
Your question specifically mentions LVADs. At present, they are not cost-effective, but the numbers have dropped from >$800,000 to <$150,000 per QALY. That is still not considered cost-effective, but the progress has been monumental. The more important point, however, is that even with the current use of about 1500 LVADs per year, this is an infinitesimally small fraction of the overall HF cost bucket. If LVADs went away altogether, we would still spend billions of dollars on heart failure. Accounting for what we can do elsewhere with more-appropriate use of hospital resources and true disease prevention, the best application of medical and device therapy will matter much more than the isolated use of LVADs.
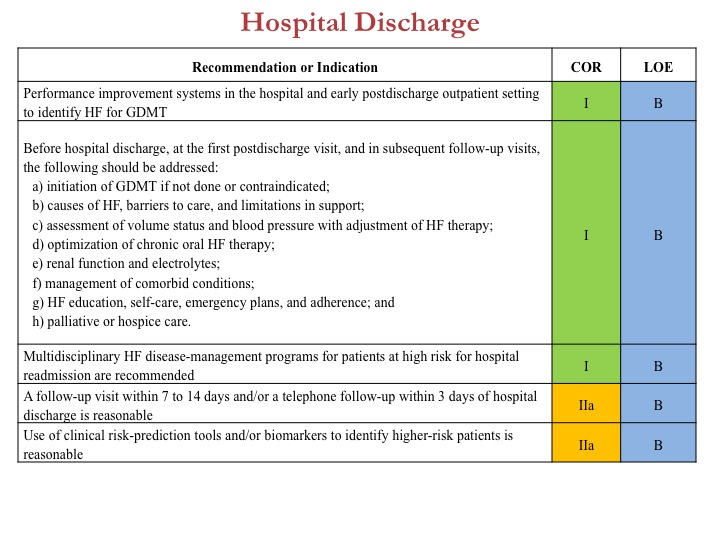
Case in point would be best deployment of evidence-based strategies to reduce readmission after heat failure hospitalizations. Taken together, these new guidelines are intended to present an updated evidence-based approach that will optimize best outcomes in heart failure, identify residual questions in heart failure, and strive for best quality.
Click here to download PowerPoint slide
To review all the content, tables, and figures from the new ACCF/AHA 2013 heart failure guidelines, click here.
JOIN THE DISCUSSION
Share your observations about the new heart failure guidelines and Dr. Yancy’s reflections on them.
August 5th, 2013
Poll: What Would You Recommend?
Richard A. Lange, MD, MBA
Your 69-year-old female patient with low-level exertional angina is referred for coronary angiography that reveals three-vessel CAD. After a lengthy discussion, the “heart team” (involving an interventional cardiologist and a cardiac surgeon) determines that CABG is the best revascularization option for this patient. A carotid Doppler study, conducted in preparation for CABG, reveals 80% stenosis of the right common carotid artery, although the patient has never had a TIA or neurologic symptoms.
Sorry, there are no polls available at the moment.