May 12th, 2020
Our Public Hospital Leads Massachusetts in Caring for Coronavirus Patients
Frances Ue, MD, MPH
Cambridge Health Alliance (CHA), where I work, is a small hospital system serving the north Boston-metro area across two campuses in Cambridge and Everett but, despite its modest scale, it has arguably become the center of Massachusetts’ fight against COVID-19. This is no small feat, given that Massachusetts has the third largest number of coronavirus patients in the U.S.

Coordinating the delivery of 10,000 N95 masks from @MADmasks2020 and Harvard Business school alumni in China & Singapore! Myself with Eugene (transitional year intern).
As of April 28, 2020, according to the statewide COVID-19 inpatient update, CHA has the greatest proportion of hospital beds and resources devoted to suspected and confirmed COVID-19 patients — 85% of our general medicine beds and 88% of our critical care beds. As a result, we greatly outrank similar-sized counterparts and even many hospitals with greater capacity. While we have been able to transfer very sick patients to tertiary care hospitals, it is alarming how disproportionately this virus is affecting the poorest and most vulnerable patients — patients for whom CHA is a lifeline.
Our capacity has more than doubled since the start of this pandemic more than 8 weeks ago, with additional medicine and critical care spaces. These spaces hardly resemble life in the hospital before COVID-19, with dedicated areas on each floor for donning and doffing personal protective equipment (PPE). Each provider is covered from head-to-toe with a face shield, scrub cap, goggles, N95 mask, Tyvek suit, nitrile gloves, and shoe covers. With only eyes visible, it is a miracle that I can recognize all our new colleagues that we welcome to the inpatient medicine teams — from primary care, family medicine, psychiatry, podiatry, and surgery. In this fight against coronavirus, we have collaborated to maximize our resources to meet the needs of all patients.
My role as Chief resident has greatly evolved during this pandemic, that role is addressed in this Academic Medicine article by our colleagues at the Beth Israel Deaconess Medical Center: Five Questions for Residency Leadership in the Time of COVID-19. There are, however, additional challenges faced by residency leadership in small community hospital settings. CHA is unique, as it is one of the few major publicly funded, safety-net healthcare systems in Massachusetts and serves as the main care provider for some of the most diverse patient groups.
Challenges have included:
1. Delivering just and culturally appropriate care to patients
More than half of our patients identify as racial or ethnic minorities and receive their care in another language, and during this COVID-19 pandemic, that percentage has continued to rise. Similar to other contagious diseases, like HIV/AIDS, coronavirus highlights health disparities of race, class, and socioeconomic status.
- A JAMA article about New York COVID-19 cases shows that the Bronx has the highest number of COVID-19 hospitalizations and deaths per 100,000 compared with other more affluent boroughs. Notably, the Bronx also has “the highest proportion of racial/ ethnic minorities, the most persons living in poverty, and the lowest levels of educational attainment.”
- Similarly, in Massachusetts, the current center of the epidemic is in Chelsea, with the highest rate of infection at about 1,890 cases per 100,000 residents, which is nearly four times the statewide rate. Chelsea is a densely populated, working class suburb bordering Boston. 68% of residents are Latino, and 19% earn below the poverty line; which is 2 times the rate in Boston-Cambridge and 1.5 times the rate in all of Massachusetts.
CHA has become a hotspot, with our Everett campus as the closest hospital to Chelsea, an 8-minute drive away. Alongside this influx in patients, there are increased demands on interpretation and dealing with the trauma felt by these communities. Vonessa Costa, director of multicultural affairs and patient services, highlights our response in this New York Times article on April 17th 2020.
2. Providing meaningful mental health support for residents
With the ongoing high acuity and volume of cases in Massachusetts and at CHA, we have started to see symptoms of distress in many of our resident physicians — recurrent nightmares about patients, anxiety, grief, and difficulty processing the death of loved ones and patients. Caring for critically ill patients is challenging during the best of times. Caring for critically ill COVID-19 patients during an evolving pandemic has taken a significant emotional and psychological toll. In response, we have partnered with psychiatry to provide a space for trainees to reflect on their caregiver trauma.
How do we provide support, while also acknowledging the ongoing trauma that our resident physicians are experiencing? Our goal for these sessions is to provide a supportive and reflective space; identify coping and self-care strategies; provide psychoeducation about crisis, stress, and trauma reactions; and identify further resources for help. Our psychiatry colleagues have been instrumental in these sessions.
3. Building community and hope
Some initiatives have included:
- Sharing ‘stories of hope’ from the frontlines at our virtual residency meetings. These include successful extubations, discharges from the hospital, and reunions with family.
- Songs and videos of successful discharges. (Here Comes The Sun by The Beatles plays at our hospital.)
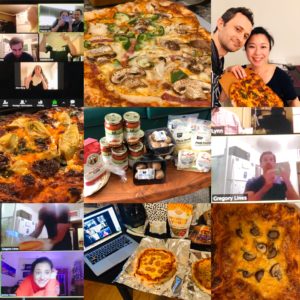
- Team bonding activities, like virtual pizza making night and trivia.
- Advocating for ourselves and our patients #GetUsPPE.
- Engaging in scholarship, like analyzing our patient outcomes related to IV fluid use and collaborating on evidence-based grand rounds.
As the COVID-19 cases start to plateau, we anticipate our patient population will continue to be disproportionately affected. For many, CHA provides a safety-net to the failings of our fragmented medical system. We are an essential resource for those who have nowhere else to go.
We might be small in size, but we are expansive in capacity and innovation. I want to give credit where credit is due. Pound for pound, I am proud that CHA and our frontline resident physicians are leading the state in caring for coronavirus patients.
Please share your perspective on caring for coronavirus patients! I would especially love to hear from others at public hospitals across the country. Leave a comment or tweet at me, @UeFrances.
Special thank you to Martin Kaminski for his contribution to this article.
Categories: About Residency
Tags: Chief Resident, community, Coronavirus, COVID-19, Pandemic, resident experience, social justice
You can follow any responses to this entry through the RSS 2.0 feed. Both comments and pings are currently closed.
2 Responses to “Our Public Hospital Leads Massachusetts in Caring for Coronavirus Patients”

2021-2022 Chief Resident Panel
Abdullah Al-abcha, MD
Mikita Arora, MD
Madiha Khan, DO
Khalid A. Shalaby, MBBCh
Brandon Temte, DO
Resident chiefs in hospital, internal, and family medicine
Learn more about Insights on Residency Training.
-
 NEJM Journal Watch – Recent General Medicine Articles
NEJM Journal Watch – Recent General Medicine Articles-
Tag Cloud
- Academic year advocacy aging art of medicine attending burnout Career Chief Resident Christmas communication community Coronavirus COVID-19 diabetes end-of-life care evidence-based medicine family medicine healthy choices Internal Medicine international medicine job interviews medical education medical students mentors oncology Pandemic patient care pediatrics Physician grief reflections Residency residency interview resident autonomy resident blog resident burnout resident experience resident wellness social justice student experience teaching technology thanks Ultrasound vaccinations wellness









Great article! Inspiring to hear the creativity and commitment with which CHA has responded!
Thank you for commenting and reading! I am so touched that this article has reached members of the CHA community far and wide. With your lifetime of experience at CHA in various roles, I wonder how some of these stories of innovation and growth compare to your experiences establishing departments and programs in the 1970s.
Cheers,
Frances