January 22nd, 2020
The ACGME Needs to Mandate Parental Leave
Eric Bressman, MD
Dr. Bressman is a Chief Resident in Internal Medicine at Icahn School of Medicine at Mount Sinai in New York, NY
My wife and I had a baby a few months ago. Or, more accurately, she birthed a child while I sat in the corner contemplating the miracle of reproductive physiology in a vasovagal fugue. In the months leading up to and following that wondrous moment, we found ourselves navigating the labyrinthine complexity of parental leave in graduate medical education.
To start with the positive, we are both residents in the same program and felt nothing but support from our own administration. We had advocates who helped us get an optimal amount of leave under the constraints of what the ACGME will allow.
But therein lies the problem. The ACGME and the various specialty boards (under the umbrella of the ABMS) are particularly restrictive when it comes to the amount of time off a resident can take in a given year and are largely silent on the topic of parental leave. This leaves the door open for wide variation in policies across institutions (e.g., Pediatrics 2013; 131:387 and Plast Reconstr Surg 2017; 139:245).
The Basics
The Family and Medical Leave Act of 1993 (FMLA) is a federal law that allows eligible employees to take 12 weeks of unpaid leave after having or adopting a child. Eligibility includes having worked for the employer for at least 12 months, which means that interns are not covered. A handful of states have expanded on FMLA and mandate a certain amount of paid leave.
The ACGME requires that institutions provide written information about the hospital’s parental leave policy on the day of the interview and as part of the residency contract, and that this policy be compliant with local laws. That’s it.
At the same time, specialty boards set limits on the amount of time off residents can take in a given year, generally on the order of 4 to 5 weeks, inclusive of vacation time. Program directors can retroactively petition for a limited extension of this leave if they feel the resident has achieved necessary competencies despite the additional absence.
This all amounts to something pretty far from a parental leave policy, and instead results in a whole lot of confusion as to what residents are actually allowed to do (JAMA 2018; 320:2372).
The Imperative
There are clear parallels between the issue of parental leave and the limits on resident duty hours. While the Bell Commission grew out of patient safety concerns, the subsequent duty hour reforms eventually were viewed through the lens of resident wellness. Parental leave needs to be considered in light of both of these concerns, with the added consideration of infant health and wellbeing. New mothers endure the physical toll of pregnancy, labor, and recovery, and both parents suffer from chronic sleep deprivation on par with any 24-hour call. To assume that these factors don’t impact clinical performance is at best naïve and at worst negligent.
The associated stress is a tremendous driver of burnout, which disproportionately affects women in medicine. Nearly 40% of surgical trainees, for example, reported that they considered leaving residency during or after pregnancy for a host of reasons, including dissatisfaction with leave options (JAMA Surg 2018; 153:644). Many women simply choose to postpone childbearing until after their training years, largely driven by perceived threats to their career paths (Acad Med 2010; 85:640). When women do become pregnant during residency, they can experience higher rates of certain pregnancy complications (Obstet Gynecol 2003; 102:948), including pre-eclampsia, preterm labor, and fetal growth restriction (N Engl J Med 1990; 323:1040).
On top of all of this, there are concerns for fetal and infant wellbeing. As physicians, we are taught the importance of parent-child bonding in the first months of life, but the combination of limited leave and long work hours leaves little room for this among our own trainees.
Solutions
For starters, the ACGME should mandate a minimum amount of guaranteed parental leave, plain and simple. As noted, the void left by not having a policy begets confusion and, in some cases, allows for dangerous working conditions.
There are two common counterarguments to legislating guaranteed leave:
- The first is the impact on training, and progress toward independent practice. Anyone who has hit the interview trail knows there is reasonable variation in how residents spend their time at different institutions. Not every rotation is handpicked for its singular educational value, and that’s OK. We are both learners and employees. Instead of blindly setting limits on time away, the ACGME and specialty boards should set specific target exposures and milestones. As long as these are attained, leave should not impede someone’s progress through training.
- The second counterargument pertains to the unfair burden placed on co-residents. Residency scheduling is a zero-sum game; one person’s leave is another person’s call. The solution is either to employ physician extenders who can fill gaps or offer overtime pay to residents who are called on to do extra work. The former was done de facto when duty hour restrictions were implemented, and the latter would, for many, turn an undue burden into a welcome opportunity.
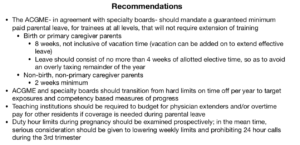
Many more arguments, pro and con, can be parsed out here, but I will leave these for another time, and instead will summarize a few recommendations, some of which are my own, others of which have been suggested elsewhere (J Grad Med Educ 2019; 11:362; click the image below).
Conclusion
The US lags behind many other countries in providing benefits for new parents. The medical community has penned multiple position papers calling on congress to rectify this disparity (e.g., ACP: Ann Intern Med 2018; 168:874). Legislative action may be beyond our control, but at the very least, we can lead by example. It’s time we get our own house in order, and there’s no better place to start than the most vulnerable among us.



“Or, more accurately, she birthed a child while I sat in the corner contemplating the miracle of reproductive physiology in a vasovagal fugue.” Hilarious line.
Being from Canada where there is a guaranteed 1 year maternity leave with partial salary, it has always astounded me how restrictive parental leave is in the United States. And complicating the matter, parental leave during residency training. Thanks for bringing attention to this important issue and congratulations on your new baby!
Cheers,
Frances
Thank you, Dr. Bressman, for submitting this piece. I agree wholeheartedly with the need for mandated, and protected, leave for residents when having children. It’s an issue for all of the reasons you stated but I actually ran into another issue when arranging my maternity leave during residency. I was attempting to take as much time off without extending my training while following the rules set forth by all the governing bodies involved; in my case this was ACGME, ABFM, and my employing institution. The plan I presented broke no rule or regulation for any of those governing bodies. However, because there is no standardization on this matter my program director was able to simply say, “No.” We argued the various points back and forth for months and did not settle on a compromise (to my dismay) until only a couple of weeks before I delivered. Ultimately, I got less time off and I had to extend my training by two weeks.
We truly need to have protected time, even during our training, because we are all still people who have lives outside of medicine that must go on. We should not be deprived the rights and privileges that all parents should have with their newborn. So again, I thank you for addressing such an important topic.
Amen! My son was born at 35 weeks the last day of intern year, as a result I had 0 vacation days for second year as the Nevada rules stipulated all my vacation days had to be used for maternity leave. It was an excellent set up for burnout. And, parental leave consisted of only 5 weeks off to stay “on track” as that was the total of my sick+vacation leave for the year. Returning from maternity leave with 0 sick and vacation days for the remainder of the year made second year absolutely terrible.
This is so important! In medicine we need to find better ways to support ourselves and our families without worrying about being judged (or punished) for taking time off or worrying about over-burdening our colleagues.
Thank you for this well thought out and articulated article. I wholeheartedly agree with and support efforts to standardize parental leave among medical residents. The phrase “physician extenders” did make me cringe, however, as I assume this refers to NPs and PAs. The accepted terminology is Advance Practice Providers (APPs) as many NPs legally practice autonomously and are not extending a physician’s ability but rather complementing it with their own.