March 8th, 2019
The Oncology Service
Ashley McMullen, MD
I won’t forget Mr. H’s face that morning, my very first morning on the medical oncology service. I skirted into his room behind my attending as she was called in to see him on the fly. With a slight smile, he sat quietly in the corner of the exam room, a tall black male of average build, alone. His open collar shirt and slacks were both wrinkled, his eyes were sullen, his close cropped hair was thinning diffusely throughout the top of his head. Outside this place, perhaps I would’ve pegged him for a car salesman, just working hard to get through the daily grind. Yet inside these clinic walls, I traced the large T-shaped scar extending from his collarbone down to the midpoint of his sternum. I took note of his soft, raspy voice. I observed how his ashen skin was in agreement with his dangerously low blood pressure. But that’s all I knew of Mr. H right then.
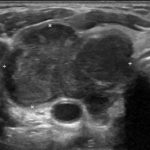
My eyes blinked and my attending was back out of the room. She needed to check on the results of Mr. H’s most recent labs and imaging studies. As she scrolled through his chart at a mind-numbing pace, she summarized the medical history… 42 y/o African American male, presented to the ED 4 weeks ago, found to have a mediastinal mass, diagnosed upon surgical removal to be anaplastic thyroid carcinoma. My First Aid lied to me! According to the text I had painstakingly committed to memory, this type of cancer was supposed to be extremely rare, popping up occasionally in elderly white females — not this middle-aged black man with four kids at home. When my attending got to the radiologist’s report, her head dropped slowly into her hands. The poisons we had dripped through this man’s veins last week had managed to shave off 15 lbs of his body weight, his appetite, his hair… basically, everything but the tumor, which had grown back to 3x its size since the initial surgery.
We’re back in the exam room. Now the attending is sitting down, next to Mr. H, her eyes meeting his eyes directly as she speaks (ironically, a bad sign in a busy specialty clinic). “I’m sorry Mr. H, but the chemo isn’t working. We can try adding radiation to slow the tumor growth, but in all honesty, this is not likely to do much. You should tell your family, and start making arrangements.” Mr. H accepted his fate with inspiring equanimity and quiet resilience. He even thanked my attending for her efforts as he headed towards the infusion center for IV fluids to bolster his decreased blood volume. I can’t help thinking that, that same evening, while I’m at home hovering over medical journals, Mr. H would be surrendering news of his prognosis to the four young children he was trying to protect. What are you supposed to do, when you’ve effectively derailed a man’s life in the course of a 15-minute visit? What’s the next step when you’ve sent a man home to tell his family that, by Christmas morning, he will be lying in a casket?




It’s a good time for your nursing staff to talk with this patient about hospice. There are things to be done to give this man and his family some assistance and comfort at this time.
Hi Dr McMullen , I’m mexican, I’m internist, and I want to thank for your courage ! I know what you were feeling that day !
First off, you did not effictively derail anyone, the cancer did. From there on great questions! Hopefully residence can learn how best to address or transfer the answers well. Good luck.