February 24th, 2017
Deep Brain Stimulation Targeting in Neurosurgery, Part I of III
Bianca Belcher, MPH, PA-C
This three-part series is for providers who lack an intimate level of knowledge and/or experience with deep brain stimulation (DBS) targeting. My goal is to provide a baseline understanding of each target, its indications, contraindications, and adverse side effects that may be observed from imperfect electrode placement and/or imperfect programming.
Specifically, I will discuss the basics regarding the three most frequently used DBS surgical targets for Parkinson’s disease (PD), dystonia, and essential tremor (ET): the ventralis intermedius (Vim) nucleus of the thalamus, globus pallidus internus (GPi), and the subthalamic nucleus (STN).
This first post will focus on the Vim.
I’ll start by briefly describing deep brain stimulation. DBS has become a commonly used and well-known surgical intervention for the treatment of medically refractory movement disorders such as PD, dystonia, and ET. The intervention involves the implantation of unilateral or bilateral electrodes that provide chronic stimulation into the deep brain at one of the aforementioned targets. The electrodes receive power from a battery-powered simulator that is typically implanted in the chest just beneath the skin and a couple of inches below the clavicle. The entire DBS system, including connecting wires, resides under the skin. We aren’t exactly sure of how DBS works, but some think that the mechanism of action is consistent with the blocking of neuronal signals transmitted through the stimulated structure and desynchronization of abnormal oscillations [1, 2].
It is important to note that DBS programming is an art form and requires a team effort. It isn’t something you just turn on and off. It requires a good knowledge of anatomy and the equipment’s capabilities. Although programmers (typically neurologists, neurosurgeons, or PAs and NPs who work in those settings) get better with experience, every patient is a little different, thus requiring finesse and good communication within the DBS team to combat programming troubles. High-volume centers generally have good working relationships between the neurology, neurosurgical, and neuropsychiatry teams for the purpose of achieving the best patient outcomes in the face of these challenges. The neurosurgery team handles the electrode placement and then communicates that placement to the programming team to give them an idea of how to start programming. Aside from proper patient selection, it is helpful to set patient expectations prior to surgical intervention. DBS is not a cure for any disease, though for many, it can significantly improve quality of life by treating their symptoms.
Ventralis Intermedius (Vim)
Where is it located?
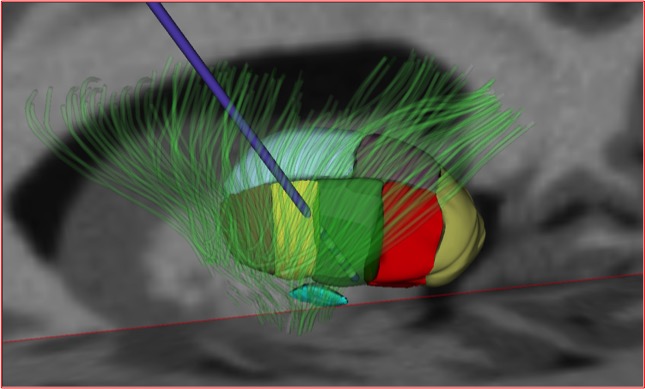
Vim (green). Subthalamic nucleus (turquoise, below VIM). (Reprinted with the permission of Medtronic, Inc. © 2017)
The ventralis intermedius is located on the ventral aspect of the lateral thalamus.
Indication:
- Tremor – Vim stimulation has been shown to be as effective as a thalamotomy but with fewer adverse side effects. Although it has excellent anti-tremor effects, it does not show the same effectiveness on other prominent parkinsonian symptoms such as bradykinesia and rigidity. For this reason, it is most commonly targeted in essential tremor and not Parkinson’s disease.
Contraindication:
- There is no glaring contraindication to the selection of this target; however, as mentioned before, it isn’t the first choice for patients with PD, and since dystonia does not have a tremor component, Vim is not an appropriate choice for dystonia.
Stimulation adverse side effects based on location of electrode in relation to optimal placement [3]:
- Too lateral: With stimulation of the internal capsule, effects consist of muscular contractions and dysarthria.
- Too medial: Potential speech and swallowing issues
- Too posterior: With stimulation of the ventral caudal nucleus, effects consist of persistent paresthesias
- Evoking paresthesias during the programming process is not abnormal in itself, but the patient will habituate – they should not be persistent.
- Too anterior: Suboptimal tremor reduction at typical voltages
- May need higher voltage to attain good control, which requires more frequent battery changes
- Too superior: No effect on tremor
- Too deep: A range of side effects depending on how deep, ranging from no effect on the tremor to ataxia and muscle contractions
In Part II of this series, I will address selection of the globus pallidus internus (GPi) as the DBS target.
References
- Benazzouz A, H.M., Mechanism of action of deep brain stimulation. Neurology, 2000. 55 (12 Supplement 6).
- Ashby P, R.J., Neurophysiologic aspects of deep brain stimulation. Neurology, 2000. 55 (12 Supplemental): p. 17-20.
- DBS Anatomy & Side Effects. A Presentation by Kirk Finnis, PhD. Medtronic.