May 1st, 2013
Which Wedge to Believe?
Tariq Ahmad, MD, MPH and James Fang, MD
A 39-year-old African American man with hypertension and diabetes reports a cough, shortness of breath, and increasing lower-extremity edema of 3 weeks’ duration. He denies chest pain, palpitations, and paroxysmal nocturnal dyspnea.
His vital signs are normal except for oxygen saturation of 90% on room air. Physical examination reveals jugular venous distension to the angle of the jaw, a widely split S2, a right ventricular (RV) heave, a right-sided S3, clear lungs, a distended abdomen, and bilateral lower-extremity edema. An electrocardiogram documents sinus tachycardia, nonspecific T-wave changes, and right-axis deviation.
Given the clinical presentation and suspicion for pulmonary hypertension, the patient is hospitalized. A transthoracic echocardiogram reveals normal left-ventricular function, an enlarged right atrium and right ventricle, moderate tricuspid regurgitation, and an estimated RV systolic pressure of 88 mm Hg.
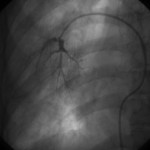
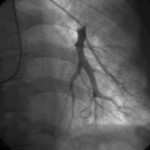
Right-heart catheterization is ordered. It identifies severe pulmonary hypertension (mean pulmonary artery pressure, 95 mm Hg) and markedly variable pulmonary capillary wedge pressures among lung segments, ranging from 12 mm Hg in the right middle lobe to 45 mm Hg in the left lower lobe.
Wedge angiograms reveal a significant delay in venous emptying patterns on one side (see images).
Questions:
1. How do you interpret the large differences in wedge pressures?
2. How do you interpret the wedge angiograms?
3. What additional testing would you perform?
4. What is your differential diagnosis?
Response:
May 8, 2013
1. The most common cause of differential wedge pressures is partial wedging of the catheter. This is a reasonable possibility when there is no suspicion of left-heart disease or when the nature of the waveform suggests it (e.g., something between a true wedge pressure and pulmonary-artery pressure). A proper wedge pressure can be confirmed using wedge oximetry (pressure >95%, or equal to arterial saturation); obtaining left-atrial pressure; measuring simultaneous LV end-diastolic pressure (LVEDP); or, as in this case, performing a wedge angiogram.
If the wedge pressures are accurate, there appears to be variable downstream obstruction to venous drainage. Given that echocardiography shows no obstruction to LV inflow, the obstruction seems to lie in the pulmonary venous system.
2. The wedge angiograms confirm the wedge position in both lungs and also reveal differences in the pulmonary arterial system.
3. At the time of catheterization, I would obtain a simultaneous LVEDP to confirm the difference between that measurement and the pulmonary capillary wedge pressure. Cardiac and chest CT are appropriate for examining the pulmonary venous anatomy, and high-resolution chest CT should be used to assess the lung parenchyma. Pulmonary-function tests usually show a decline in diffusion capacity. Some clinicians would consider a ventilation-perfusion scan, but it may not be able to distinguish pulmonary arterial hypertension from pulmonary veno-occlusive disease. Lung biopsy is a high-risk diagnostic procedure in this clinical setting.
4. Veno-occlusive disease is the primary diagnostic consideration, as it can be associated with parenchymal pulmonary diseases, malignancies/chemotherapy (especially after bone-marrow transplant), hypercoagulable states, and (possibly) toxins or infections. If the patient has undergone catheter ablation for atrial fibrillation or lung transplantation, pulmonary venous stenosis should be considered.
Follow-Up:
May 17, 2013
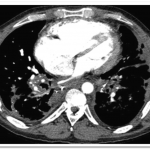
The pulmonary angiograms raised a concern for pulmonary venoocculsive disease, prompting a cardiac MRI that showed evidence of pulmonary vein occlusion (especially L-sided). CT of the chest revealed diffuse peri-bronchovascular bundle thickening with peripheral nodular opacities, as well as multiple hilar and mediastinal calcified lymph nodes—findings most consistent with sarcoidosis (see images below). Biopsy of a mediastinal lymph node showed non-necrotizing granulomatous lymphadenitis, consistent with a diagnosis of sarcoidosis.
Final diagnosis: Severe pulmonary hypertension and right-heart failure, caused by extrinsic compression of the pulmonary venous structures due to sarcoidosis-related lymphadenopathy
April 30th, 2013
Anticoagulation Update: New Agent for Urgent Anticoagulation Reversal, Pradaxa Label Revised
Larry Husten, PHD
Here are two small but important changes in the anticoagulation field:
FDA approves new product for urgent reversal of anticoagulation. The FDA yesterday approved Kcentra (Prothrombin Complex Concentrate, Human) for the urgent reversal of vitamin K antagonist (VKA) anticoagulation in adults with acute major bleeding. Unlike plasma, which is currently the only available method to reverse anticoagulation, the new product does not require blood group typing and does not need to be thawed, so it can be quickly delivered to patients, the FDA said. Kcentra is manufactured by CSL Behring.
The Kcentra label will include a boxed warning about the risk of blood clots. The FDA says that patients who take Kcentra “should be monitored for signs and symptoms of thromboembolic events, as both fatal and non-fatal arterial and venous thromboembolic complications have been reported in clinical trials and post marketing surveillance.”
The FDA said that Kcentra is derived from the pooled plasma of healthy donors and is processed “in a way to minimize the risk of transmitting viral and other diseases.”
Pradaxa label gains boxed warning. The label for dabigatran (Pradaxa, Boehringer Ingelheim) will now contain a boxed warning advising patients that discontinuing treatment increases the risk of stroke. Previously the label contained similar information but it had not been highlighted. The Pradaxa label also now includes thrombocytopenia in the postmarketing experience section and includes more details from the pivotal RE-LY trial.
April 29th, 2013
Selections from Richard Lehman’s Literature Review: April 29th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint selections from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
JAMA 24 Apr 2013 Vol 309
Association of Perioperative β-Blockade with Mortality and CV Morbidity Following Major Noncardiac Surgery (pg. 1704): A great big retrospective study finds that taking a beta-blocker is associated with a small reduction in post-operative mortality and major cardiac events in some subclasses of patient undergoing non-vascular surgery. Alarm bells: how tightly were these groups pre-specified? How watertight was the propensity scoring and matching? The NNT to prevent one post-op death was 241: this could be massaged down by factoring in cardiac risk factors, to about 18 for the highest risk patients—but questions remain. The comparison was not between patients given beta-blockers short term for the peri-surgical period, but with people mostly taking them long-term. And high-risk patients undergoing vascular surgery showed no benefit. It doesn’t really add up: this is why we always need to do prospective randomized trials to decide the merits of treatment, rather than processing big bagfuls of old data.
NEJM 25 Apr 2013 Vol 368
Intestinal Microbial Metabolism of Phosphatidylcholine and CV Risk (pg. 1575): Trimethylamine-N-oxide (TMAO) is the new enemy within. We make it in our bowels, I am sorry to have to report, by microbial metabolism of the choline moiety in dietary phosphatidylcholine (lecithin). The fault lies with our microbiome, because as this study demonstrates, if you kill off the bacterial flora with metronidazole and ciprofloxacin, production of TMAO stops totally. The second part of the study goes on to associate TMAO levels with atherosclerosis, proving to its own satisfaction that if you produce shitloads (I use the word in its technical sense) of TMAO then you get major adverse cardiovascular events, independent of other known risk factors. I am naturally inclined to pooh-pooh this idea, but to do so would involve going into a level of detail that neither you nor I could quite face. There is lecithin in the kinds of food that cardiologists traditionally dislike—eggs, red meat, liver and pork—but there is also plenty in fish and most plants. I have just eaten a bagful of whelks—probably lots of lecithin there too, but you won’t stop me so easily. After all, “Lecithin may help to prevent the buildup of fats in the body and protect against cardiovascular disease by lowering cholesterol,” says the Nutritional Supplements Health Guide website.
Biventricular Pacing for Atrioventricular Block and Systolic Dysfunction (pg. 1585): I keep a safe distance from interventional cardiologists, but hope that when my turn comes they will know what they are doing. If I had systolic heart failure, I would most definitely not want a cardioverter-defibrillator, but if I had atrioventricular block I would want to have whatever kind of pacing gave me the most benefit. In this life-shortening condition, I would place a high value on symptomatic improvement. Unfortunately, this Medtronic-funded trial of right ventricular pacing versus biventricular pacing did not measure quality of life at all: it went for the usual mixture of hard end-points (death, admission for IV treatment) and a surrogate—an end-systolic volume increase of 15%. Biventricular pacing proved superior on those counts, and we also know from other studies that it improves symptoms, so that’s what I’d go for if I had grade 1-3 systolic HF. My aim would be to live better and then die suddenly: so yes to BVP, and no, no, no to that ICD.
JAMA Intern Med 22 Apr 2013 Vol 173
HIV Infection and the Risk for MI (pg. 614): Living with human immunodeficiency virus doubles your chance of having a myocardial infarction, according to this Veteran’s cohort study. It sound like everyone on antiretroviral treatment should be taking a statin.
Dietary and Supplemental Calcium Intake and CV Disease Mortality (pg. 639): The debate about dietary calcium intake and cardiovascular disease continues. This study examines the relation in a whopping cohort of 388 229 men and women aged 50 to 71 years from the National Institutes of Health–AARP Diet and Health Study. The chalk-eating men seem to get more CVD whereas the women don’t.
Bias in Associations of Emerging Biomarkers With CV Disease (pg. 664): There are far too many cardiovascular risk factors. Most of the studies are bad. Even when they are of reasonable quality, they tend to be of doubtful clinical significance. This paper written under the supervision of that invaluable sceptic, John Ioannidis, concludes that “Selective reporting biases may be common in the evidence on emerging cardiovascular biomarkers. Most of the proposed associations of these biomarkers may be inflated.”
April 28th, 2013
Stories from a Heart Transplant Pioneer: Blogging from ISHLT 2013
William Kent Cornwell, MD
William K. Cornwell III, M.D., is blogging for CardioExchange from the International Society for Heart and Lung Transplantation (ISHLT)’s Annual Meeting in Montreal.
This year, the International Society for Heart and Lung Transplantation (ISHLT) has given the Pioneer in Transplantation award to Dr. Jack Copeland. During his address, Dr. Copeland led us on an interesting walk through the history of heart transplantation. One of the highlights of his speech was a story from 1972, when transplant surgeons were actually accused of murder after harvesting organs from a patient. Only after proving that the donor had suffered brain death were they found not guilty. Another interesting story involved a surgeon who harvested an organ, and then got a flat tire while driving the heart back to the hospital and had to change his own tire before implanting the heart into the recipient. Lastly, Dr. Copeland reminisced about the first transplant he performed in Arizona, on a patient named Dutch Tarr. Though Tarr was eligible for Medicare, his claim for the procedure was denied. Tarr successfully sued Medicare for reimbursement of the procedure. The case led to the National Heart Transplantation Study, with the objective of determining whether heart transplant was cost-effective, necessary, and reasonable. This study paved the way for all future heart transplants to be reimbursable procedures. Dr. Copeland has had a wonderful career, and it was great to listen to a man who is etched in the history books — truly, a living legend.
April 26th, 2013
Conflicting Results from Two Trials of Cardiac Resynchronization Therapy
Larry Husten, PHD
Two new trials have ended up reporting conflicting results regarding the expansion of the indication for cardiac resynchronization therapy (CRT) for patients without a wide QRS interval. The positive results of the smaller trial seem likely to be undermined by the early stopping of the much larger trial.
The first trial, NARROW-CRT, published in Circulation: Arrhythmia and Electrophysiology, concluded that CRT “improved clinical status in some patients with ischemic cardiomyopathy, mild-to-moderate symptoms, narrow QRS duration, and mechanical dyssynchrony on echocardiography.” The second trial, EchoCRT, which was testing CRT in heart failure (HF) patients with narrow QRS, was terminated early due to futility.
In NARROW-CRT, Carmine Muto and colleagues randomized 120 ischemic HF patients with echo evidence of dyssynchrony and a QRS < 120 ms to either a CRT device or a dual chamber ICD. At one year improvement in the clinical composite score — the primary endpoint — had occurred in 41% of the CRT patients versus 16% of the ICD patients (p=0.004). The investigators reported a trend in favor of CRT for the secondary endpoint of HF hospitalization and HF death (p=0.077) and a significant benefit for another secondary endpoint — HF hospitalization, HF death, and spontaneous ventricular fibrillation.
The positive finding of NARROW-CRT appears not to have been supported by the early termination of the much larger EchoCRT. The trial, sponsored by Biotronik, was recently halted due to futility. (Although patients and investigators have been informed of the early stopping, no public announcement by the company or the sponsor has been made to date.) The trial had been designed to evaluate the effect of CRT on morbidity and mortality in HF patients with a narrow QRS (< 130 ms) and with echo evidence of dyssynchrony. Results of the trial are expected to be presented at a medical meeting in the near future.
Although the full results of the trial are not yet known, it appears unlikely that they will support an expanded FDA indication for CRT or that another large trial will be performed in this population. However, several trials are now exploring expanded use of CRTs in other areas. The publication in the New England Journal of Medicine earlier this week of the BLOCK HF trial may lead to an indication for CRT in patients with heart block and LV dysfunction. Other trials include the recently initiated MIRACLE EF trial, which is looking at CRT as a primary treatment in HF patients with LBBB and mild LV dysfunction, and the ongoing PROMPT trial, which is evaluating LV or biventricular pacing as a treatment to prevent adverse myocardial remodeling early after myocardial infarction.
April 25th, 2013
Another Cleveland Clinic Study Links TMAO to Atherosclerosis
Larry Husten, PHD
A new study from the Cleveland Clinic research group headed by Stanley Hazen offers more evidence in support of the hypothesis that TMAO (trimethylamine-N-oxide) may play a role in the development of heart disease. The new research, published in the New England Journal of Medicine, follows closely on a related study published recently in Nature Medicine that received broad public attention.
The Nature Medicine paper demonstrated that digestive tract bacteria metabolize carnitine into TMAO, which had previously been linked to atherosclerosis in animals. The new research in NEJM focuses on another pathway that leads to TMAO production and provides for the first time a credible association between TMAO and cardiovascular disease in humans.
In the first phase of the new study, the researchers gave a precursor of TMAO, lecithin, to a group of healthy volunteers both before and after receiving antibiotics. Without antibiotics, the lecithin was metabolized to TMAO. But when the intestinal bacteria were suppressed by the antibiotics, TMAO production was significantly reduced.
In the second phase, the researchers measured fasting plasma TMAO levels in 4007 patients undergoing coronary angiography. After 3 years of follow-up, people in the highest quartile of TMAO had more than twice the risk for having a major adverse cardiovascular event than people in the lowest quartile (HR 2.54, CI 1.96-3.28, p<0.001). This association was independent of traditional risk factors.
In an accompanying editorial, Joseph Loscalzo praises the research but notes that “much remains to be done to determine the precise role of TMAO in atherothrombogenesis — whether it has a direct effect on pathogenesis, is an epiphenomenal biomarker, or is a precursor to a more direct effector.” In any case, Loscalzo is supportive of a significant role for gut bacteria: “Atherosclerosis,” he writes, “has long been recognized to be partially driven by inflammation, and the gut metagenome appears to contribute to this inflammatory milieu.”
April 24th, 2013
Quinidine In Ireland: Rarely Needed, Hard To Find
Gerard J Fahy, MD, Niamh O'Hanlon, BPharm MSc Grad Dip Risk Mgmt Cert Pharm Prac and John Ryan, MD
Recently in the Journal of the American College of Cardiology Viskin et al published the results of a survey looking at the worldwide availability of quinidine. They found that the drug — the only effective oral antiarrhythmic in Brugada syndrome and idiopathic ventricular fibrillation — is readily available in only 19 countries and is unavailable or requires special procedures to obtain it in 99 countries. One country where quinidine is unavailable is Ireland. CardioExchange’s John Ryan asked Dr. Gerry Fahy, a cardiac electrophysiologist from Cork University Hospital, and Niamh O’Hanlon, a pharmacist at St. Vincent’s University Hospital, to discuss their experiences with quinidine in Ireland.
Fahy: Quinidine is rarely used in Ireland. For the past two years I have had only one patient on quinidine because of Brugada syndrome and a history of polymorphic VT and atrial fibrillation. Brugada syndrome appears to be rare in Ireland. My patient lives in West Cork but is originally from Sri Lanka.
Although quinidine is not marketed in Ireland it can be acquired from suppliers in the United Kingdom within 24 hours. On the rare occasions that it has been needed at short notice, such as for a patient with electrical storm, we have acquired it without undue delay from other hospital pharmacies who happened to have a supply. I think it is important to have a reliable supply available at short notice for the occasional patient who may need it. I will be contacting our hospital pharmacy to ensure that we will have a supply at all times. In the past ten years we have several times had a similar problem with the supply of isoproterenol.
O’Hanlon: We are able to obtain an unlicensed source for oral quinidine sulfate 200mg for inpatient use at our hospital though there may be some delay. Kinidin durules (quinidine bisulphate 250mg modified release preparation), which in the past was available, has been discontinued. The Irish Medicines Board does not list a licensed quinidine preparation.
Community pharmacists are able to order quinidine sulfate 200mg, but because it is unlicensed it is not directly reimbursable, so there would be an additional cost to the patient, although some patients may be eligible for reimbursement due to hardship.
It should be noted that there is a real Sound Alike Look Alike Drug (SALAD) issue with quinidine, which can be confused with quinine tablets (quinidine is an isomer of quinine). Quinine is prescribed in primary care for the relief of night cramps and is available as 200mg and 300mg quinine sulphate/sulfate oral preparations.
April 24th, 2013
Adiposity and Natriuretic Peptides: Where Does the Fat Go?
Ian Neeland, MD
In a study recently published online by JACC, investigators assess the association between natriuretic peptide levels and body-fat distribution. Ian Neeland, the lead author of the study, responds to John Ryan’s questions.
THE STUDY
The researchers used data from the Dallas Heart Study to conduct a cross-sectional analysis of BNP and NT-proBNP levels and various measures of body fat and adiposity (e.g., BMI, total body fat, lean mass, lower-body fat, visceral and subcutaneous fat, and liver fat) in 2619 participants without clinical heart failure. Both NT-proBNP and BNP levels were inversely associated with visceral fat and liver fat and positively associated with lower-body fat.
THE AUTHOR RESPONDS
Ryan: Why did you do this study?
Neeland: I’m interested in the relationship between body-fat distribution and cardiovascular health, especially with regard to obesity. Although it is fairly well established now that increased adipose tissue may have adverse cardiac effects, the scientific community is just starting to recognize that this is a bidirectional process — the heart can also exert effects on adipose tissue through secretion of natriuretic peptides. In animals, BNP can stimulate lipolysis, leading to dissolution of fat stores, and can also alter body-fat distribution. Since this work has not yet been translated to humans, we wanted to investigate the relationship between BNP and NT-proBNP levels and fat distribution (assessed by MRI and DEXA imaging) in adults without heart failure. We found that higher natriuretic peptide levels (still within the physiologic range) were associated with less visceral and liver fat (both linked to cardiometabolic disease) and with more lower-body subcutaneous fat, which is a “healthy” fat depot. This suggested to us that natriuretic peptides secreted by the heart may exert beneficial effects on fat metabolism in humans.
Ryan: In your study, a low BNP was associated with increased visceral adiposity. What is the proposed mechanism behind this?
Neeland: Visceral fat is probably much more sensitive than lower-body subcutaneous fat to the lipolytic effects of BNP. When BNP is relatively deficient (such as in obesity), visceral fat may begin to accumulate. This could cause both increased clearance of BNP from the bloodstream and lipotoxicity-induced suppression of BNP synthesis and release from the heart. Chronically low levels of BNP would then result in more visceral fat accumulation, and the cycle could go on and on.
Ryan: You have previously shown that excess adiposity in the lower body is associated with a lower prevalence of metabolic risk factors. Do you think that the interaction of BNP with fat plays a prognostic role in this association?
Neeland: The link between greater amounts of lower-body fat and metabolic health is an exciting area of research right now. It’s long been recognized that women have higher BNP levels than men. Women also have more lower-body fat and less visceral fat than men. It’s plausible that higher natriuretic peptide levels in women could positively influence fat distribution into the lower-body compartment rather than the abdomen, which may explain some of the difference in cardiovascular prognosis between the sexes.
Ryan: If a patient in overt heart failure who is also obese is found to have a low BNP, should we be screening for metabolic syndrome or diabetes?
Neeland: Although it’s certainly intriguing to speculate that low BNP levels in patients with obesity and heart failure reflect underlying metabolic disease, our study does not address the heart-failure population. BNP related to heart failure may be a totally different animal than physiologic BNP. In fact, patients with advanced heart failure with very high BNP levels tend to be lipodystrophic, with abnormal adipose tissue biology resulting in muscle and fat wasting, and don’t demonstrate favorable adiposity profiles at all.
Ryan: What therapeutic potential might energe from this work on BNP and fat distribution?
Neeland: First, if natriuretic peptides truly alter fat distribution in humans, we could potentially treat abdominal obesity by increasing BNP levels. Levels can be increased by administering recombinant BNP, stimulating BNP synthesis, or inhibiting the catabolism and clearance of BNP. This approach has failed to improve heart-failure outcomes in the past (e.g., omapatrilat and nesiritide) but may still hold promise for obesity. Also, our study may partially explain the beneficial effects of physical activity in treating the metabolic syndrome, since exercise both enhances natriuretic peptide release and preferentially reduces visceral fat mass.
April 24th, 2013
BLOCK HF: CRT Superior to Conventional Pacing in Heart Failure Patients with AV Block
Larry Husten, PHD
Patients with atrioventricular (AV) block generally receive right ventricular (RV) pacing; cardiac resynchronization therapy (CRT) has been restricted to patients with a low ejection fraction and a wide QRS duration. However, RV pacing may worsen LV dysfunction in AV block patients with low ejection fractions. Previous studies have raised the possibility that these patients may benefit from biventricular pacing with a CRT device.
Now, results from the BLOCK HF (Biventricular versus Right Ventricular Pacing in Heart Failure Patients with Atrioventricular Block) trial, published in the New England Journal of Medicine, lend more support for the expansion of CRT devices into this population. Anne Curtis and colleagues randomized 691 patients to standard RV pacing or biventricular pacing. After 37 months of follow-up, a primary outcome event — death, urgent care visit for heart failure that required intravenous therapy, or a 15% or more increase in the LV end-systolic volume index — occurred in 55.6% of the RV pacing group versus 45.8% of the biventricular pacing group (HR 0.74, CI 0.60-0.90).
The results were similar, and remained significant, when only the first two components of the endpoint were considered. The investigators also reported “a remarkably similar clinical effect, despite a marked difference” in ejection fraction, in the pacemaker and ICD groups.
In a comment published in Journal Watch Cardiology, Mark Link writes that the trial “extends the patient population that benefits from cardiac resynchronization therapy to those with left ventricular ejection fractions greater than 35% who are likely to require pacing a high percentage of the time…. The body of evidence is thus approaching critical mass to render future trials comparing right ventricular pacing and CRT unethical, perhaps even in patients with preserved LVEF.”