December 28th, 2016
A Reflection on The Hippocratic Oath
Kashif Shaikh, MD

Kashif Shaikh, MD, is the 2016-17 Chief Resident in Internal Medicine at the University of Central Florida College of Medicine.
Questions for young physicians:
Do you remember and recall the series of events that inspired you to become a healthcare provider? Are you satisfied with the field of medicine? Have you ever thought about your perceptions of healthcare before and after becoming a physician? Have you ever been a patient yourself? What attributes in our healthcare system do you wish didn’t exist or need to change?
After finishing my rounds in the ICU, I was speaking to one of our charge nurses. We were discussing the advent of electronic health records and charting and its effects on patient satisfaction. She has been a nurse at our hospital for more than 25 years. Her thoughts: She was able to chart effectively and efficiently before the advent of EMRs, and she was also able to spend considerable amount of time at the bedside speaking with patients. But now, she must meet the excessive demands of EMR charting, which are strictly enforced. This has led to a decreased amount of time spent at the bedside with patients.
Patient satisfaction scores and charting are key determinants in hospital reimbursement these days. Insurance companies are the main driver in the relationship between adequate charting and hospital reimbursement. But the required “adequate charting” affects patient satisfaction scores in inadvertent ways: A frequent complaint that we hear from our patients is that the providers don’t spend enough time talking to them at the bedside!
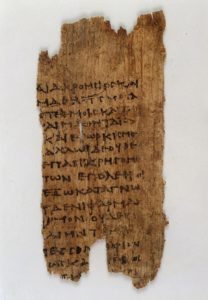
Papyrus text: fragment of Hippocratic oath. Wellcome Library, London. Wellcome Images (http://wellcomeimages.org). Copyrighted work available under Creative Commons Attribution only license CC BY 4.0.
Here is he modern Hippocratic oath, to refresh our memories:
“I will remember that I do not treat a fever chart, a cancerous growth, but a sick human being, whose illness may affect the person’s family and economic stability. My responsibility includes these related problems, if I am to care adequately for the sick.”
I had another conversation, similar to the one I had with our nurse, with one of our senior vascular surgeons. He has been a surgeon for more than 30 years. He mentioned how he spends hours working on his daily progress notes on the electronic health record. We also discuss how much time is spent on charting in the U.S. compared with other countries. For example, in the U.K., charting is done specifically to document pertinent patient information, for the sole purpose of patient care, rather than to justify requirements of insurance companies for billing purposes.
Sadly, today, most providers at the hospital are busy charting and documenting patient care in front of computer screens. Providers go to great lengths to meet requirements for healthcare reimbursement, and most of them are under time constraints to complete their paperwork. They also put in orders electronically. These tasks directly affects the amount of time spent at the bedside talking to the patients. The components in the history & physical and progress notes mandated by the insurance companies require a substantial effort, and some of those requirements have no bearing on patient care.
I agree that EMRs are a more cost-effective and efficient way to track patient care than is paper charting. It is also an effective way to put in orders. But a universal EMR would save tremendous resources. But we need to define an effective universal EMR system for documentation and charting that targets patient safety, quality, and continuity of care. Those functions would allow us to do what healthcare providers need to do: Spend time at the bedside talking to our patients and their families (read: increase patient satisfaction). It would also foster good rapport between healthcare teams and patients.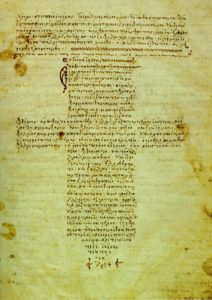
Foto de la Biblioteca Vaticana scan from book. User: Rmrfstar [Public domain], via Wikimedia Commons
I would like to end this article on the last paragraph of the Hippocratic Oath.
“If I do not violate this oath, may I enjoy life and art, respected while I live and remembered with affection thereafter. May I always act so as to preserve the finest traditions of my calling and may I long experience the joy of healing those who seek my help.”
Residency isn’t easy. But it doesn’t have to be quite so hard. Explore NEJM Resident 360.

![By Jerry Berger [CC BY-SA 4.0], via Wikimedia Commons](https://blogs.jwatch.org/general-medicine/wp-content/uploads/sites/4/2016/08/EMR-300x200.jpg)
![Clinic Painter [CC BY 3.0], via Wikimedia Commons](https://blogs.jwatch.org/general-medicine/wp-content/uploads/sites/4/2016/08/AncientMedicine-300x270.jpg)


Many feel the Hippocratic oath had some deficiencies, and was somewhat outdated and incomplete. I agree however with your notes that it has a a lot of important things of merit to consider. It only relates (of course) to individuals – not health care systems – do THEY have a similar oath?
P.S. Was surprised to realize my own statement/aphorism – “treat the patient – not the results” is a direct take from the HO.
Very good piece. I am one of those physicians who completed residency training and entered community practice prior to the widespread dissemination of the EHR. I am one of many who saw their immense promise and who have subsequently experienced such immense disappointment and frustration. We would do well to follow your two main proposals: first, agree on a single open-source platform (for example, the one on which the VA system is based); second, agree as a community of professionals to resist/defy the pressures of the industry, and turn our attention back to the patient and her family.
As long as the patient remains the pawn instead of the customer and as long as physicians kowtow to extortionists, forget altruism.
Dr Shaikh,
Please consider that physicians CAN make choices to shape their professional future. Be brave and do not accept simple employment by a healthcare institution, but instead, choose private practice where you can choose the type of EHR you use, or choose NOT to use one at all, if it suits you. Work to procure technology that truly benefits your practice and your patients. Consider being independent of the demands of health insurance companies and administrators of institutions by being an independent private practice- perhaps by rejecting insurance as payment- allow your patient and yourself to partner on treatment plans without the interference of these same insurance companies and institutions, whose motivations are not so pure as yours.
Look into Docs4PatientCare (d4pcfoundation.org), as an organization trying to promote the primacy of the physician-patient relationship, and facilitate physicians acting as true advocates for their patients. And consider restoring the dignity of your profession by referring to yourself and colleagues as “physicians” rather than “providers”- at least “clinicians”.
Physicians CAN be successful as independent entities.
Pass the word!
Many hospitals have “scribes” so that the MD doesn’t have to chart, just review the note.
Yes, it’s a catch-22 situation- we have to chart why we do something and why we do not. I think though that it’s more to prevent litigation- it does have to do with reimbursement as well. Maybe a software engineer will come up with a program where the MD just speaks and it types and enters it into the medical record. In rounds years ago-the MD spoke into a voice recorder and the transcriptionust typed the note-pasted it in the chart and the MD signed off on the note during follow-up rounds.
Yes- I use voice dictation that scribes then enter into the “medical record”. It works.
IDEALLY the record shows the physicians THINKING, as well as a transcript of what was done.
Pilots use cockpit voice recorders . . . and now video’s.