April 5th, 2011
MAGELLAN: Higher Bleeding Rates Cloud Rivaroxaban’s Effect in VTE Prevention in Acutely Ill Medical Patients
Larry Husten, PHD
The novel anticoagulant rivaroxaban is successful in preventing venous thromboembolism (VTE) in acutely ill medical patients, but a high bleeding rate means the drug probably won’t be used for this indication. Alexander Cohen, presenting the results of the MAGELLAN trial at the ACC in New Orleans, explained by way of background that 50% to 70% of symptomatic thromboembolic events occur in nonsurgical patients.
Some 8,101 patients were randomized to either oral rivaroxaban for 35 days or subcutaneous enoxaparin for 10 days followed by placebo. Among the findings:
- At 10 days, the primary efficacy measure – a composite of asymptomatic proximal DVT, symptomatic DVT, symptomatic nonfatal PE, and VTE-related death – demonstrated that rivaroxaban was noninferior to enoxaparin. The primary outcome occurred in 2.7% of patients in each group (RR = 0.968; p=0.0025).
- At 35 days, rivaroxaban was significantly better than enoxaparin and placebo, as the composite endpoint was reached by 4.4% of patients on rivaroxaban versus 5.7% on enoxaparin and placebo (RR 0.771, p=0.0211).
However, there was a significantly increased risk for bleeding with rivaroxaban at both 10 and 35 days:
- At 10 days, clinically relevant bleeding occurred in 2.8% of rivaroxaban patients versus 1.2% of enoxaparin patients (RR=2.3; p< 0.0001).
- At 35 days, clinically relevant bleeding occurred in 4.1% of rivaroxaban patients versus 1.7% of enoxaparin patients (RR=2.5; p<0.0001).
At day 35, the net clinical benefit – defined as the composite of asymptomatic proximal DVT, symptomatic DVT, symptomatic nonfatal PE, VTE-related death, and treatment-emergent major plus non-major clinically relevant bleeding – occurred in 9.4% of the rivaroxaban group versus 7.8% of the enoxaparin/placebo group.
In response to a question after his presentation, Cohen explained that very few AF patients were enrolled in the trial because most of them would already have been receiving anticoagulation.
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 5th, 2011
Malpractice Lawsuits and Cardiology: Searching for a Safe Harbor
Sandeep Mangalmurti, MD, JD
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
Both New Orleans and ACC.11 continue to remain a feast for the mind and the palate, as we continue through Day 3 of the summit. Too many presentations and too little time…a week would still not be enough.
I made a point of attending a symposium on Professional Liability Claims today, both due to intellectual interest and personal self-preservation; like most physicians, I expect to be sued someday. The lessons imparted are worthy of dissemination, I think. The moderator and discussant (Dr. William Oetgen, MD, MBA and Dr. Frank Flannery, MD, JD) took us through actual case studies where cardiologists had been sued for medical malpractice, and then discussed the key teaching points.
Some of the lessons should already be familiar to cardiologists: follow up on test results, keep patients informed of abnormalities, document extensively and accurately. Basic professionalism goes a long way in managing malpractice risk, and physicians who fail to meet these fundamental standards should be held to account.
A more vexing dilemma is how to deal with liability risk in clinically ambiguous situations where decisions require a balancing of risks and benefits. Here is an actual malpractice case for your review: The patient is a 27-year-old male with a history of obesity and hypertension who presents to his primary care doctor with complaints of 10 days of dizziness, weakness, and near syncope. He is generally a quite active outdoorsman, whose hobbies include rock climbing and scuba diving. His family history is significant only for hypertension and MI. He is noted to be bradycardic to <50 bpm, and serial EKGs show significant conduction abnormalities, including an intermittent LBBB and RBBB, as well as eventual 2:1 AV Block. He remains very symptomatic in the ER, and is immediately transferred to the ICU for monitoring, with a STAT cardiology consult. This cardiologist diagnoses possible complete heart block, and consults a cardiac surgeon for possible pacemaker placement. A DDD device is placed without complication, and the patient is eventually discharged from the hospital to resume his life.
The patient eventually moves out of the area and follows up with a new cardiologist for continued management of his pacemaker. Interrogation shows that the patient no longer requires pacing; his new cardiologist wonders whether his previous heart block might be due to Lyme disease, given the patients’ history of outdoor activity. Lyme titers are ordered, and are positive.
The patient files a lawsuit against the ER physician, the original consulting cardiologist, and the cardiac surgeon, arguing that they were negligent in failing to test for Lyme disease and failed to meet standard of care by placing a permanent instead of a temporary pacemaker. He further alleges that by not fully informing him of the possibility of Lyme disease as a reversible cause of his condition, informed consent was never obtained. The defendant physicians maintain that routinely checking for Lyme disease is not the standard of care, especially given the absence of history of tick bites or rashes; they resolve to take it to a jury.
One of the most important issues in this case is identifying the appropriate standard of care; specifically, is it standard of care to routinely check Lyme titers in this clinical situation? Sometimes this question degenerates into a battle of experts, with each side marshalling its own witnesses to define the standard in a manner most advantageous to their client. The consequences of ambiguous and shifting standards of care are clearly undesirable. If they don’t know the standard of care, providers may defensively order unnecessary tests and procedures. The actual cost of defensive medicine remains controversial, with estimates ranging in the tens of billions annually. One need only consider the policy consequences of the aforementioned case to appreciate how quickly the costs can add up. If failure to test for Lyme disease is a breach of standard of care, does everyone require this test prior to pacemaker placement? Or does there need to be a “reasonable” clinical suspicion, and if so, what is it? Will busy cardiologists even care what is “reasonable”? Are they likely to just order the test on everyone just to be safe?
In an attempt to add some more consistency and predictability to the system, both providers and policymakers have considered using professional guidelines as a surrogate for standard of care. Adherence to clinical guidelines would serve as a “safe harbor” against liability. These “safe-harbor” statutes were previously attempted in Maine, and have been considered at the national level. In another version of this policy proposal, adherence to guidelines would not automatically shield against liability, but failure to adhere would be powerful evidence of malpractice. (For an excellent discussion of this topic, see Mello M. Of swords and shields: the use of clinical practice guidelines in medical malpractice litigation. Univ Penn Law Rev 2001;149:645-710.)
So do the ACC guidelines help us define standard of care in this case? Somewhat…per the guidelines: Permanent pacemaker implantation is not indicated for AV block that is expected to resolve and is unlikely to recur (e.g., drug toxicity, Lyme disease, or transient increases in vagal tone or during hypoxia in sleep apnea syndrome in the absence of symptoms). However, this is only a Class III recommendation, so it is hardly dispositive, and may not be extraordinarily helpful either to cardiologists or juries. In the absence of formal safe harbors, we are still forced to use guidelines as just one piece of evidence presented to juries, to be given whatever weight they see fit.
In this case, the jury found that standard of care was violated, and Lyme titers should have been drawn prior to placement of either a temporary or permanent pacemaker. However, only $50,000 was awarded, suggesting that the jury did not find the plaintiff had been injured significantly. In the end, one suspects that both defendants and plaintiffs walked away from this case feeling injured.
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 5th, 2011
RIVAL Trial Tests Radial Versus Femoral Access
Larry Husten, PHD
Radial access for angiography has gained increasing acceptance in recent years based on the promise of reduced complications and increased patient comfort. At the ACC, and in a simultaneous publication in the Lancet, Sanjit Jolly and colleagues presented the results from RIVAL, the largest trial to date comparing radial versus femoral access.
Some 7021 ACS patients about to undergo angiography were randomized to either radial or femoral access. The primary outcome – a composite of death, MI, stroke, or non-CABG-related major bleeding at 30 days – occurred in 3·7% of patients in the radial access group versus 4·0% of patients in the femoral access group (HR 0·92, CI 0·72–1·17; p=0·50).
However, in the following prespecified subgroups, radial access demonstrated a significant advantage over femoral access:
- in centers in the highest tertile of volume: HR 0·49, CI 0·28–0·87, p=0·015
- in patients with STEMI: HR 0·60, CI 0·38–0·94, p=0·026
Here are more overall results:
- The rate of death, MI, or stroke at 30 days was identical in both groups: 3.2%.
- The rate of non-CABG-related major bleeding at 30 days: 0·7% in the radial group versus 0·9% in the femoral group (HR 0·73, CI 0·43–1·23, p=0·23).
- Large hematoma at 30 days: 42 of 3507 in the radial group versus 106 of 3514 in the femoral group (HR 0·40, CI 0·28–0·57, p<0·0001).
- Pseudoaneurysm needing closure: 7 patients in the radial group versus 23 in the femoral group (HR 0·30, 95% 0·13–0·71, p=0·006).
In combination with results from previous trials, the data “show that radial access reduces major vascular complications compared with femoral access,” according to the investigators. “Percutaneous coronary intervention success rates seem to be similar. Both patients and clinicians might choose radial access because of its similar efficacy and reduced vascular complications.”
In an accompanying comment, Carlo Di Mario and Nicola Viceconte point out that although the highest-volume operators had better results with radial access, the group in the middle tertile had the worst outcome. In addition, they note that the radial approach did not reduce the hospital length of stay or the amount of contrast used. Nevertheless, they offer a cautious endorsement of the technique, writing that there is now “little justification to ignore one of the main developments in interventional cardiology and stubbornly refuse to embrace a technique likely to reduce minor adverse events (but in patients with STEMI, possibly also major adverse events and mortality) and improve patients’ comfort. Especially, operators with a high workload of acute procedures should seriously consider retraining in radial angioplasty, and all new trainees should be taught and become proficient with this approach. Conversely, it is important not to demonise the femoral approach, which is more suitable when large guiding catheters are required and prolonged procedural time is expected for complex lesions, such as chronic total occlusions, some large bifurcations, and diffuse or very calcified lesions.”
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 5th, 2011
Great Things at the ACC Poster Hall
Amit Shah, MD, MSCR
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
One of my biggest challenges in coming to conferences like ACC is figuring out how to handle the painful dilemma of choosing amongst 3-4 sessions that are being broadcast simultaneously. From talking to others, I’m not alone in this!
Nonetheless, one of the things I’ve appreciated here is the down-time that is given to actually attend posters between talks; in contrast, I never found the time to do it at AHA because of so many excellent talks going on throughout the day, with no breaks! This was really nice…
In the process of perusing a few of the posters, I came to really appreciate the great science they have to offer, but simultaneously lamented the fact that I only had time to check out a small percentage of them. Nonetheless, a few caught my eye…
One study, by Makani et al, showed results from a meta-analysis of dose-response relationship in anti-hypertensive therapy. It found that for most anti-hypertensives, except for ARB’s, the level of blood pressure control is not significantly different between high and low doses. A little surprising, but useful…perhaps the next time my patient is above goal, I should consider adding another class of medication, rather than the increasing dose of another medication?
Another poster I found interesting was the study of AMI hospitalizations before and after Hurricane Katrina by Hameed et al. Excellent timing, I thought. Not only did the study find a 3-fold increased prevalence of AMI amongst yearly hospitalizations after the hurricane, but it also found that many psychosocial factors, like joblessness, were more prevalent in the AMI victims after the hurricane. While the literature abounds on psychosocial risk factors and heart disease, I found this study unique and compelling. I think it’s always good to keep cardiologists around in times of natural disasters, superbowls, and NCAA championships! In response to the recent earthquake in Japan, perhaps we should be shipping statins and beta-blockers, in addition to food and water?
Many more interesting studies to discuss/report, but I’ll leave that for another time, or for any other contributors…feel free to share!
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
ACC the Second Time Around: Pharmacology Spotlight on HF and A-Fib and Immersion at the Heart Hub
Hansie Mathelier, MD
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
After attending my first ACC conference last year and feeling overwhelmed by all the potential knowledge I could acquire, I felt like this would be different experience because I was no longer a novice attendee. Boy I was wrong! But the difference for me this year and last year is that I am ok with not being able to attend everything that I want to.
On Saturday I attended the Pharmacology Spotlight conference regarding atrial fibrillation and heart failure. Who knew, that if you wanted a seat you needed to arrive at 6am… Just kidding but not really. The expected attendance for these two conferences was underestimated. An overflow room twice the original conference size was needed to allow all knowledge seekers to attend! Was the attendance to these sessions filled to capacity because of the topic or the meat of the conference had not begun? I think a mixture of both.
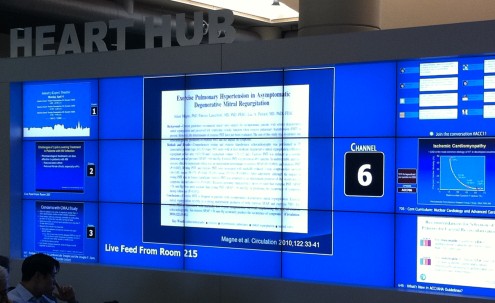
The best part of my Saturday morning was sitting at “Heart Hub” and being able to watch six talks at the same time in a comfortable chair. I easily could see myself sitting at “Heart Hub” everyday to maximize my learning. It is also the perfect place for the cardiologist who wants to multi-task the conference by being able to toggle between the talks. After about 90 minutes, I realized sitting here throughout the conference would give me a headache.
I am off to patio to get my daily dose of vitamin D and plan the rest of my day and perhaps conference.
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
The Real Show: The Expo Hall
Justin M Vader, M.D.
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
There’s a sucker born every minute. I am that sucker. I went to the Expo hall with the plan of scoring some swag – maybe a pair of calipers that are subtle enough not to pique my son’s interest in the sharp objects in Dr Dada’s white-coat pockets. I left the Expo hall with $200 less in my pocket. But by God I will now hear that phantom S4 my clinic attending hears in everyone – I have purchased an electronic stethoscope. The truth will out Dr Geltman!
The Expo hall is awesome in the original sense of the word. The billions of dollars of innovation in the room, the creative energy poured into the displays, the many attractive people at the booths that remind us why we had to work hard to get good grades in school because it just wasn’t going to be easy with a mug like this – awesome truly. In a way, I’ve found the Expo hall equally as informative as the scientific sessions given that it shows both what’s new and intriguing and how we’ll meet these technologies and products in the marketplace. Designs in echo seem to be moving towards the Apple-simple with the ability to acquire multiplane images then later integrate and analyze after the patient is gone. Anyone who has been run over and nearly killed by an echo machine rolling down a ramp near the CT surgical ICU (not that it’s ever happened to me or anything) will appreciate the shrinking size. Health information technology outfits are present but surprisingly unboisterous given that a common thread of discussion here is electronic health records and the financial incentivization of uptake now rather than later. I would wonder if it might be that everyone who’s going to buy in has bought in, but my own august top 10 American hospital home still uses paper charts and dictaphones with manual transcription – there must be plenty of other places twiddling their technological thumbs. This is all coming from a guy who has a broken 5-year-old Samsung flip phone – more Luddite than “early-adopter”. Even more quiet than the electronic health record companies are the drug companies who have segued to minimalist displays, and, in the case of Daichi-Sankyo, Zen gardens. Makes you long for the dog days of statin warfare.
Beyond the Expo hall and lecture rooms, I’ve been surprised to find that the real pleasures of being here are in-between rooms, in the halls of the conference, and out in the Vieux Carre. Meeting friends from residency who are training elsewhere has been both a chance to catch up on real life events (babies, divorces, marriages) and a chance to gain perspective on work life and training. Though there’s undoubtedly a selection bias, friends from residency seem genuinely happy with life in cardiology training and optimistic about the future…even after a few beers/hurricanes/glasses of absinthe/etc. It’s reaffirming.
I’ll leave off here. The other guys’ posts captured some of the better moments of the day yesterday. I’ll be headed back tomorrow, so I’ll leave some parting impressions for what they are worth later this afternoon. Late-breaking trials just came across this morning – STICH, EVEREST II. More fun to be had.
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
“Speed Dating” Lunch for Fellows in Training: Board Prep, Career Development, and Financial Planning
Amit Shah, MD, MSCR
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
Free lunch! That’s all that needed to be said to attract masses of fellows. Today I attended an excellent and tasty lunch-time session for the Fellows In Training (FITs) called “What you need to know in starting a cardiology career.” It was a very informative session with several 15-minute mini-lectures (“speed dating”) on a hodgepodge of different career topics. Many of the key points were practical and thought-provoking. Here I offer some “tweets” – needless to say, there are many important points I am leaving out…
Boards Prep by Dr. Goyal and Dr. Murphy
- Take the boards as soon as you are eligible, and during fellowship; when you are attending, it only gets more difficult
- 90% of people pass the boards; if they fail, it’s usually because of the ECG section….wait, isn’t that supposed to be our bread and butter!? We get stooped by the guessing penalty and short amount of time allotted
- O’Keefe is an excellent ECG book that provides many didactic ECG cases
- Know class I and III guidelines for some of the main topics
- Questions can be tricky: in a sense, it is a mind game between you and the question-writer
- If demographics are provided for an ECG, it’s because it’s an essential part of the question
- One of the best ways to learn is to actually write practice questions
- Clinical trials that have been released within the last 12 years will not be covered because of the lag time between writing questions and having them appear on the test
Careers Talks with Susan Childs, Dr. Cuffe, and Dr. Walsh
- In the face of many changes and uncertainty, many private practices are moving to the hospital-employed; strength lies in numbers
- Accountable care organizations will change the face of cardiology; read more here
- Several different estimates of average salary were given, ranging from 220K to 300K+; geography matters — certain states such as Minnesota, Indiana, and New Hampshire offer more attractive salaries
- All negotiating power is gone once the contract is signed; make sure to ask for a contract as well! Otherwise you may just get a signed letter
Academia vs. Private Practice is a complex, multifaceted debate:
- Either you are building your nest (private practice) or you are trying to climb the ranks (academia)
- Academia offers a large range of career types, from bench researcher to clinician educator to administrator
- Academia can include other, non-salary financial benefits, such as tuition benefits for children.
- Although academia is usually chosen for the opportunity to teach and do research, private practice does not entirely cut-off these opportunities. Nonetheless, in academia one is engaged in a structured, vibrant, intellectual community
- Every academic center is different: “If you’ve seen one, you’ve only seen one.”
- Too much protected time may be a bad thing if you cannot show for it with productivity, as justifying it may be difficult down the road
- Entering a practice in a big city is obviously more competitive and difficult; in such cases, it is important to understand the specific needs of that market
Last and not least, Michael Merrill and Anders Ramstad from North Star presented an excellent financial planning talk…
- Do you know your net worth? Most fellows have a net-worth average of NEGATIVE 150K
- Try to keep an emergency reserve of 3 to 6 months of expenses
- Debt rule – if you have any debt with greater than 8% interest, pay it off ASAP!!!
- Do not finance a home for more than 3 times your salary; otherwise “prepare to eat food that starts with HOT and ends with DOG”
- Disability insurance is highly recommended
- Put away 20% in long-term saving; Roth IRA is the way to go because we are in the lowest tax bracket we will be in moving forward.
Did you attend? If so, what did I miss? Or do you have other advice that you’ve heard on these topics that you’d like to share?
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
PRECOMBAT Explores PCI Versus CABG for Left Main Disease
Larry Husten, PHD
In the PRECOMBAT trial, Korean investigators randomized 600 patients with unprotected left main disease to either PCI with a sirolimus-eluting stent or CABG. The results were presented at the ACC and published simultaneously in the New England Journal of Medicine.
At 1 year, the incidence of the primary composite endpoint – death from any cause, MI, stroke, or ischemia-driven target-vessel revascularization – was 8.7% (26 patients) in the PCI group versus 6.7% (20 patients) in the CABG group, for an absolute risk reduction of 2% (95% CI -1.6 – 5.6, p=0.01 for noninferiority). At 2 years, the incidence was 12.2% for PCI versus 8.1% for CABG (HR 1.50, 95% CI 0.90 -2.52, p=0.12).
The authors conclude that although the trial “met the prespecified criterion for noninferiority,” their results “cannot be considered to be clinically directive” because “the power of the trial was lower than anticipated and because the noninferiority margin was wide.”
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
Viewing the ACC from Afar: It Is Not the Same
John Ryan, MD
Several Cardiology Fellows who are attending ACC.11 this week are blogging together on CardioExchange. The Fellows include Sandeep Mangalmurti, Hansie Mathelier, John Ryan (moderating and providing an outsider’s view from Chicago), Amit Shah, and Justin Vader. See the previous post in this series, and check back often to learn about the biggest buzz in New Orleans.
Part of the argument to explain decreasing conference attendance in recent years is the rise of electronic communication. This morning when I awoke, I had already received a few emails detailing the results of PARTNER A from a variety of news sources. And although I now had access to a variety of sound-bites regarding stroke risk and vascular complications, I realized that I was missing something. I was missing the buzz in the room when results like these are produced, but most of all, I was missing the ability to form my own opinion of these results.
Also, the electronic updates mostly address only the major, late-breaking clinical trials. They do not address the smaller, intimate sessions where new advances and innovative thinking are unveiled. The findings and proposals introduced at these sessions, such as carotid applanation tonometry, can take up to year before reaching publication, if not longer. Often, it is the side rooms that you stumble into when you cannot find any of your friends that prove the highest yield. The other advantage of going to these smaller talks is that they can provide fodder for one’s own research projects. Thomas Ryan, MD, (no relation) once told me that the best research at the national conferences is often in the poster hall and advised me to spend as long a time as possible walking carefully through the science presented there. Again, this isn’t possible when fifteen hundred miles away.
One of the great bonuses of attending these meetings is getting the chance to see one’s co-fellows present. Many fellowship programs offer a dry run where, in the weeks leading up to the meeting, fellows present their talks to their peers and faculty. Again, this pales in comparison to being there for the real thing. Of course, sometimes the dry run goes a lot better than the conference talk, but getting the chance to see your colleagues present is a unique opportunity, should not be taken for granted, and should not be missed.
From a faculty perspective, there are several reasons to ration the number of meetings that one attends — limited time-off, funding constraints, and heavy clinical and research burden. However, as fellows, this is our time to take advantage of having some more freedom with our schedule, as we are defining our interests and careers. Although previously I did not fully appreciate the unique opportunities that these national meetings offer, I know now that there is more to these conferences than can be summarized in 140 characters or less.
For more of our ACC.11 coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting, check out our Coverage Roundup.
April 4th, 2011
ACC.11: CardioExchange Coverage Roundup
CardioExchange Editors, Staff
Whether you’re attending ACC.11 or not, check out our coverage of late-breaking clinical trials, interviews with the authors of the most important research, and blogs from our fellows on the most interesting presentations at the meeting.
VIEWS AND ANALYSIS
- PARTNER A: An Investigator’s View: Michael Mack, a principal investigator of the PARTNER study of TAVI versus AVR in patients with aortic stenosis, discusses the results released at ACC.11 and answers questions from CardioExchange’s Rick Lange and David Hillis.
- STICH: What’s the Value of CABG in Patients with LV Dysfunction?: Eric Velazquez, an investigator for the STICH (Surgical Treatment for Ischemic Heart Failure) trial, discusses the findings presented at ACC.11 and answers questions from CardioExchange’s Anju Nohria.
- TAVI: PARTNER or Blind Date?: Rick Lange looks at the PARTNER results and asks, “Will you offer TAVI to your ‘high-risk’ aortic stenosis patients as an ‘excellent alternative’ to AVR?”
FELLOWSHIP BLOGS
- Flying Back Home: Reflections on ACC.11: Hansie Mathelier looks back at her ACC.11 experience and gives us the “Top Eight Things” that she learned while at the conference.
- Getting “Under the Skin” of Resistant Hypertension: Amit Shah describes a new technology in the pipeline for combating treatment-resistant hypertension — an implantable Baroreceptor Activation Therapy device.
- Malpractice Lawsuits and Cardiology: Searching for a Safe Harbor: Sandeep Mangalmurti discusses the lessons he learned at a symposium on professional liability claims.
- Great Things at the ACC Poster Hall: Amit Shah appreciates the down time he has at ACC to spend in the Poster Hall and discusses two of the studies he found most interesting.
- ACC the Second Time Around: Pharmacology Spotlight on HF and A-Fib and Immersion at the Heart Hub: Hansie Mathelier describes her second time attending ACC, discussing a surprisingly well-attended conference and the informative — but headache-inducing — experience of the Heart Hub.
- The Real Show: The Expo Hall: Justin Vader marvels over the innovative technology to be found in the Expo hall, and finds the true pleasure of the meeting to be reconnecting with old friends from residency.
- “Speed Dating” Lunch for Fellows in Training: Board Prep, Career Development, and Financial Planning: Amit Shah recounts a lunch session for fellows-in-training that was full of great information about starting a cardiology career.
- Viewing the ACC from Afar: It Is Not the Same: John Ryan discusses what is lost when a conference is experienced solely through electronic communication.
- The Cardiology Profession: At the Table or on the Menu?: Sandeep Mangalmurti reflects on the plenary lecture and the profession in the context of health policy.
- From Far in the Future to the Here and Now: Reflections on the Translational Research Symposium and a Session on VADs: Justin Vader attends a session on stem cells and a Mayo Clinic session on VADs.
- Who’s Paying for the Fellows?: John Ryan asks what meetings fellows want to attend and how they get there.
NEWS
PREVIEWS
- A STICH in Time: Presenter Eric Velazquez previews the Surgical Treatment for Ischemic Heart Failure trial being presented at ACC.
- A Meeting That Could Change How You Practice: John Ryan previews the ACC.11 for fellows and other attendees.
- Choosing a PARTNER for Life: A or B?: Rick Lange previews the showdown between surgery and TAVI.
- A Delectable Side Benefit of ACC — New Orleans Restaurants: John Ryan offers some tips on New Orleans cuisine.
