January 5th, 2015
FDA Approves New Drug-Coated Balloon to Open Blocked Leg Arteries
Larry Husten, PHD
Medtronic said today that it had received approval from the FDA to market its IN.PACT Admiral drug-coated balloon (DCB) to treat peripheral artery disease (PAD) in the superficial femoral and popliteal arteries. The device is the second DCB to gain FDA approval. Last October the FDA approved CR Bard’s Lutonix DCB for a similar indication.
The new DCB uses the anti-proliferative drug paclitaxel, which is designed to prevent renarrowing (restenosis) of the blood vessel after it is opened by the expanded balloon. Approval of the device was based on the landmark IN.PACT SFA trial published last month in Circulation. Target lesion revascularization was dramatically reduced in that trial from 20.6% in the group who received standard balloon angioplasty to 2.4% in the DCB group. Medtronic noted in its statement that approval had been granted without the use of an FDA advisory panel.
The IN.PACT Admiral DCB has been available in Europe since 2009.
January 5th, 2015
Healthy Habits of Young Women Lead to Long-Term Health Benefits
Larry Husten, PHD
It may seem obvious, but a new study shows that young women with healthy habits are less likely as they age to get coronary heart disease or go on to develop cardiovascular risk factors like high blood pressure, high cholesterol, or diabetes.
Andrea Chomistek and colleagues analyzed data from more than 88,000 women participating in the Nurses’ Health Study II and who were between 27 and 44 years of age at the start of the study. The investigators used six criteria to assess the lifestyles of their subjects: smoking, body weight, physical activity, television viewing, alcohol consumption, and diet. Women who met all the criteria for a healthy lifestyle — nonsmokers, normal body weight, physical activity for at least 2.5 hours each week, minimum television viewing, moderate alcohol consumption, and a healthy diet — had almost no heart disease and low rates of CV risk factors after 20 years of followup.
When compared with women who met none of the criteria, these women had a 92% reduction in risk for coronary heart disease and a 66% reduction in CV risk factors. With the exception of television viewing, all the individual criteria were significantly and independently associated with improved outcomes. It’s worth noting that only about 5% of the women in the study met all six criteria. The results are published in the Journal of the American College of Cardiology.
In an accompanying editorial, Donna Arnett, a former president of the American Heart Association, writes that although the findings of the study are hardly surprising, the “study represents another instance of the conceptual broadening of the CV public health discussion to trumpet the power of primordial prevention,” which means focusing less on “the things we should not be doing in our effort to prevent disease to the things we should be doing in our effort to promote health.”
Although young women already have low rates of CV disease, in recent years the increases in diabetes and obesity appear to have put a stop to earlier advances against CV disease in this group. “If there’s any hope of successfully convincing young women (and everyone else) not to smoke, to exercise more, and to eat and drink prudently, it lies in creating a world in which doing those things is the default option,” writes Arnett.
December 24th, 2014
An Examination of MR CLEAN
Rory J Spiegel, MD
CardioExchange welcomes this guest post from Dr. Rory Spiegel, who is a third-year and chief Emergency Medicine resident at Newark Beth Israel Medical Center. This piece originally appeared on his blog, EM Nerd.
Published in the NEJM on December 17th 2014, ushered in with the inflated fanfare only the medical industry is capable of, MR CLEAN marks the first successful trial of interventional therapy for acute ischemic stroke. In direct contrast to IMS-3, SYNTHESIS, and MR RESCUE, MR CLEAN is a significantly positive trial. The authors demonstrated success in their primary outcome — “improved neurological outcomes at 90 days” — with an adjusted odds ratio of 1.67 (95% confidence interval [CI], 1.21 – 2.30). Why MR CLEAN was positive when the three trials that came before were negative is still unclear. As discussed in my previous post (as well as far more elegant posts on emlitofnote.com and stemlynsblog.org) it may be due to better equipment, faster symptom onset to recanulization times, and the incorporation of CT angiography to identify a cohort of patients who would truly benefit from these invasive interventional strategies. Conversely it may simply be due to the traditional therapy group performing so poorly.
A closer look at the results from MR CLEAN reveal that though the interventional group outperformed the placebo group by a significant amount (an absolute increase of the number of patients alive and independent by 13.5%) compared to its peers, its performance was far from exceptional. In the IMS-3 trial, 40.2% patients in the control arm (tPA alone) were alive and independent at 90 days compared to only 32.6% of the patients in the intervention arm of the MR CLEAN trial. Even the placebo groups in NINDS and ECASS-3 who received no reperfusion therapies had better outcomes than the patients receiving interventional therapies in the MR CLEAN trial. Twenty-six percent and 45.5% of the control patients in the NINDS and ECASS-3 trials, respectively had a mRS of 0 or 1 at 90 days. Compared to only 11.6% of the patients in the interventional arm of MR CLEAN.
Though it is difficult and not completely appropriate to compare groups from different trials, it does call into question the reasons for MR CLEAN’s staggering success. It may very well have been that the patients in the MR CLEAN cohort were far sicker than the earlier stroke trials, (though both their presenting NIHSS and 90-day mortality rates seem quite similar). It may be that the utilization of CT angiography to select patients for recruitment excluded the majority of the stroke mimics who were included in these earlier trials, and will universally have good outcomes (this seems to be the answer given by the authors when queried by Dr. Ryan Radecki). The subgroup analysis, which indicated only the patients with a NIHSS of greater than 20 demonstrated a statistically significant benefit from endovascular therapy, seems to support this supposition. The authors point to a meta-analysis of the six trials examining endovascular therapy for acute ischemic stroke as additional proof. In this analysis by Fargen et al, published in the J NeuroIntervent Surg, the authors examine the subgroup of patients with radiographically confirmed large vessel occlusion (LVO). Similar to MR CLEAN, patients receiving endovascular therapy had better outcomes at 90 days (a mRS of 0-2 38.3% vs 25.8% respectively ). Even in this combined cohort with radiographically confirmed LVO, outcomes were not as dire as those observed in the MR CLEAN trial.
MR CLEAN’s success may be attributed to the advancements in both procedural proficiency and technological prowess. But it is equally likely that the whimsy of random chance was responsible for these impressive results. On a final note, it is important to remember that all of the trials examining endovascular therapy in acute ischemic stroke were compared to a control group that included the administration of IV tPA, an intervention whose own efficacy is very much in doubt. Although the rate of adverse events in the intervention arm of MR CLEAN did not differ significantly from those given IV tPA, this is only because alteplase comes with its own terrifying set of unpleasantries. When compared to a true placebo group, I am certain the rate of symptomatic intracranial hemorrhage and new ischemic stroke (7.7% and 5.6%, respectively) would appear far more concerning.
Given the universal failure of the previous three trials examining the very same question, surely more confirmatory evidence is required before investing the unimaginable resources required to support the vast infrastructure needed to make interventional therapy a reality. Since MR CLEAN’s success was announced at the 9th annual World Stroke Conference in Istanbul held in October 2014, two trials examining endovascular therapy in acute ischemic stroke, ESCAPE and EXTEND IA, have halted enrollment early for benefit. It will be interesting to see if these premature stoppages were because of preplanned interim analyses or if MR CLEAN’s success influenced their early termination. I hope we invest the time and resources required to answer these questions with the methodological rigor they deserve. It would be frustratingly tragic to once again be forced to practice with continual doubt because we halted all further investigations out of the fear of discovering that reality is not as promising as the false-truth gained from interpreting only the data that pleases us.
December 22nd, 2014
Selections from Richard Lehman’s Literature Review: December 22nd
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
NEJM 18 December 2014 Vol 371
A Randomized Trial of Intra-arterial Treatment for Acute Ischemic Stroke (OL): Dutch researchers have investigated the effect of removing clot from the blocked cerebral arteries following stroke, usually after initial treatment with alteplase. Collectors of silly acronyms will be pleased to note that this trial was called Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands—MR CLEAN. Intra-arterial thrombolysis, mechanical treatment, or both, was compared with usual care—which could include intravenous alteplase—in patients with a proximal intracranial arterial occlusion of the anterior circulation that was confirmed on vessel imaging. The primary outcome was the score on the modified Rankin scale at 90 days. The modified Rankin scale is a 7 point scale ranging from 0 (no symptoms) to 6 (death). A score of 2 or less indicates functional independence. This score was obtained over the telephone by an assessor blinded to treatment allocation. There was an absolute difference of 13.5 percentage points (95% CI, 5.9 to 21.2) in the rate of functional independence (modified Rankin score, 0 to 2) in favour of the intervention (32.6% vs. 19.1%). There were no significant differences in mortality or the occurrence of symptomatic intracerebral haemorrhage. Now this is significant news. If you ask any doctor what they would like if they have a stroke, it is either to die or to come out relatively unscathed. This intervention does not reduce your chance of dying but it increases your chance of regaining independent function. So I’d go for it—although the stroke services and delivery times in your part of the world probably aren’t as good as those in the Netherlands.
JAMA 17 December 2014 Vol 312
Effects of High vs Low Glycemic Index of Dietary Carbohydrate on Cardiovascular Disease Risk Factors and Insulin Sensitivity (pg. 2531): A pitifully short trial, with a small sample size, poor completion rate, and entirely surrogate markers. Is this what we need to guide a lifelong intervention for hundreds of millions of people? Alas, it is not. This was an overambitious crossover trial in which 163 overweight adults (systolic blood pressure, 120-159 mm Hg) were given four complete diets that contained all of their meals, snacks, and calorie-containing beverages, each for five weeks. The results were gathered for all who completed at least two diet cycles, and they showed that diets with low glycaemic index of dietary carbohydrate, compared with high glycaemic index of dietary carbohydrate, did not result in improvements in insulin sensitivity, lipid levels, or systolic blood pressure. No matter: I am strongly inclined to believe that a low glycaemic index diet might be beneficial to vast numbers of people, but this is not the way to test it.
December 18th, 2014
Demystifying the Taboo of Sex Counseling After Acute MI
Stacy Tessler Lindau, MD, MAPP
The CardioExchange Editors interview Stacy T. Lindau about her research group’s prospective observational study of sexual-activity counseling for adults, age 18 to 55, in the U.S. and Spain during the first month after acute MI. The study is published in Circulation.
Editors: Please briefly summarize your results.
Lindau: Our main finding was that very few patients, particularly women, reported receiving counseling about sexual activity after an acute MI, even though the majority had been sexually active during the year before the MI. Those who received counseling were often given restrictions not supported by evidence or guidelines.
Editors: Why do you think this is an important area to study?
Lindau: Healthcare providers are people, and sexuality is both a core characteristic and a private matter for most people — so I understand why the topic is often avoided. However, our study and others show that people — even those with life-threatening illnesses — value their sexual function and believe that it is appropriate for healthcare professionals to raise the issue. When the topic of sexual function is omitted, patients perceive that it’s not relevant to their medical condition or that they are alone in experiencing problems resuming normal sexual activity. Healthcare providers simply need to bring up the topic.
U.S. and European guidelines on best practice after MI recommend counseling about sexual activity. So if the physician does not bring it up, the patient may need to put aside his or her discomfort and ask the doctor straight up, “Is it ok for me to resume sexual activity — and when? What symptoms should I look out for?” Our prior research shows that in the year after MI, mortality risk was no higher among people who resumed sexual activity than among those who didn’t — in fact, the risk for death was lower among the people who did resume sex.
Editors: Did anything in your results surprise you?
Lindau: Interestingly, among women who received counseling about sexual activity after MI, those in Spain were significantly more likely than those in the U.S. to be given restrictions. That finding suggests that cultural factors, physician factors, or both influence decisions about sexual-activity counseling after an MI. Such factors are mutable, and no clear medical reason explains this difference in practice.
Editors: What should we do to improve our care in this area?
Lindau: I will continue encouraging physicians to talk with their patients about sexual activity in the context of healthcare. Healthcare providers, especially the physician who knows the patient’s heart best (to quote a finding from one of our prior studies), should routinely inform all patients — women and men, young and old, married and single, sexually active before the MI and not — that it is ok to engage in sexual activity. They should also explain which symptoms should prompt cessation of sexual activity and be reported to the doctor. For reproductive-age people who have a heart attack, preserving sexual function is not only relevant to preserving intimacy and pleasure, but obviously also critical with respect to childbearing.
JOIN THE DISCUSSION
Do you counsel your post-MI patients about sexual activity? Will Dr. Lindau’s study change your approach to this issue?
December 17th, 2014
Dutch Trial Gives Support to Thrombectomy for Ischemic Stroke
Larry Husten, PHD
A large new trial provides the first substantial evidence that thrombectomy may be beneficial in patients with acute ischemic stroke. Previous thromboectomy trials have been disappointing; some experts have speculated this may be due to the use of early-generation devices, long treatment delays, and difficulties in recruiting suitable patients into the trials.
The Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN), published in the New England Journal of Medicine, was designed to address the limitations of previous trials. Some 500 patients with ischemic stroke were randomized to usual care or the addition of intraarterial treatment within 6 hours of symptom onset. Ninety percent of patients in both groups received intravenous alteplase before randomization. More than 80% of patients in the intraarterial treatment group were treated with a contemporary retrievable stent. Treatment was open label but the endpoint evaluation was blinded.
There were significant differences between the groups in outcomes. For the primary outcome measure, there was a one-point reduction in the modified Rankin scale at 90 days, from 4 in the control group to 3 in the treatment group. Some 32% of patients in the treatment group and 19% of patients in the control group were functionally independent (modified Rankin score, 0-2). The results were consistent across all prespecified subgroups.
There was no difference in mortality between the groups. More patients in the treatment group had clinical signs of a second ischemic stroke in a different vascular territory (5.6% versus 0.4%).
In addition to the use of retrievable stents, the authors speculated that a key factor in the success of intraarterial therapy in their trial was that all patients had a radiologically proven intracranial occlusion.
In an accompanying editorial, Werner Hacke praises the trial as a “first step in the right direction” but believes that it is too early to proclaim thrombectomy “the new standard treatment for severe stroke with proximal large-vessel occlusion up to 6 hours after stroke onset.” Several ongoing trials are still needed, he writes.
December 16th, 2014
No Advantage for Low-Glycemic-Index Diet
Larry Husten, PHD
In recent years the glycemic index (GI), a measure of a carbohydrate’s impact on blood sugar, has assumed a major role in discussions about diets and nutrition. Now a study suggests that by itself, within the context of an otherwise healthy diet, GI may not be an important factor in improving cardiovascular risk.
In a paper published in JAMA, Frank Sacks and colleagues report the results of a randomized, crossover-controlled, 5-week feeding trial comparing four different diets in 163 overweight or obese adults. The diets were either low- or high-carbohydrate and either low- or high-GI. Importantly, all the diets were based on previously established healthy dietary patterns based on the DASH diet, which is low in saturated and total fat and includes substantial amounts of fruits, vegetables, and low-fat dairy foods.
The findings did not suggest any major benefits associated with low GI. In the main comparison of interest, the low-GI, low-carbohydrate diet — when compared with the high-GI, high-carbohydrate diet — lowered triglycerides from 111 to 86 mg/dL but had no significant impact on insulin sensitivity, systolic blood pressure, LDL cholesterol, or HDL cholesterol. Unexpectedly, in a comparison of the low and high-GI diets within the high-carbohydrate group, insulin sensitivity was decreased and LDL was increased in the low-GI group.
The authors caution that their trial did not attempt to “address the effect of glycemic index in a typical US diet.” They also warn that they did not study the effect of lowering GI in people who have type 2 diabetes or for weight loss. Current evidence suggests that a low GI diet may be helpful in these situations.
Another factor to consider is that because “nutrients often cluster… the effects of glycemic index, if any, might actually result from other nutrients, such as fiber, potassium, and polyphenols, which favorably affect health.”
In an accompanying editorial, Robert Eckel writes that the “unexpected findings of the study… suggest that the concept of glycemic index is less important than previously thought, especially in the context of an overall healthy diet…. These findings should therefore direct attention back to the importance of maintaining an overall heart-healthy lifestyle, including diet pattern.”
December 15th, 2014
The Latest on Culprit-Vessel vs. Multivessel Primary PCI for STEMI
Bilal Iqbal, MBBS MRCP PhD and CardioExchange Editors, Staff
The CardioExchange editors interview M. Bilal Iqbal about his study group’s real-world observational analysis of culprit-vessel versus multivessel intervention at the time of primary PCI for STEMI. The study is published in Circulation: Cardiovascular Quality and Outcomes.
CardioExchange: How do your data, results from the PRAMI trial, and findings from the unpublished CVLPRIT trial differ? And what conclusions can we draw from all of these data?
Iqbal: Certainly, a lot of recent data explores revascularization strategies for STEMI patients with multivessel disease, and the recent PRAMI and CVLPRIT randomized trials add to the evidence base. These important studies, together with future randomized trials, will define how we manage bystander coronary artery disease at the time of primary PCI. I’m not sure our observational study tells us anything new compared with previously reported registry analyses, but it does offer a more contemporary analysis in a real-world setting. We must acknowledge the limitations of observational analyses. Although we used various statistical methodologies to address measured confounders, unmeasured confounders may have affected the results. Therefore, our results should be considered hypothesis-generating.
In the CVLPRIT trial, a strategy of complete revascularization before hospital discharge was associated with improved outcomes. The PRAMI trial found that a strategy of complete revascularization at the time of primary PCI was associated with improved outcomes. Although the two trials suggest that complete revascularization is a superior strategy, the composite endpoints in these studies included outcomes that may themselves be dictated by treatment strategy (e.g., refractory angina, ischemia-driven revascularization).
In our study, the main outcome analyzed was mortality. With respect to mortality, no difference was found between the two strategies in either PRAMI or CVLPRIT. Furthermore, our study looked specifically at culprit-vessel versus multivessel intervention at the time of primary PCI (index intervention procedure), whereas CVLPIRT studied complete versus incomplete revascularization before hospital discharge. Notably, in CVLPRIT, 57% of the patients underwent multivessel revascularization at the time of the primary PCI, and the rest received complete revascularization before discharge. An important question stemming from CVLPRIT is whether outcomes are better with complete revascularization at the time of primary PCI or before hospital discharge.
CardioExchange: STEMI guidelines have traditionally recommended culprit-vessel intervention alone. Do you think the issue needs to be re-addressed by the guidelines, or are the data from your study sufficient to leave them as they are?
Iqbal: Again, our study is observational and should only be considered hypothesis-generating. Given the results of PRAMI and CVLRIT, it is clear that the issue needs to be re-addressed in the guidelines. However, further trials are required to define the optimum revascularization for patients and with STEMI and multivessel disease. We must wait and see what future studies tell us.
CardioExchange: If you have a patient who comes in with STEMI and other lesions, what are you recommending?
Iqbal: At present, our practice reflects current recommended guidelines, and we perform culprit-only PCI in the absence of cardiogenic shock and/or ongoing ischemia.
JOIN THE DISCUSSION
How does Dr. Iqbal’s study influence your perceptions of culprit-vessel versus multivessel primary PCI for STEMI?
December 15th, 2014
Selections from Richard Lehman’s Literature Review: December 15th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
NEJM 11 December 2014 Vol 371
Factor XI Antisense Oligonucleotide for Prevention of Venous Thrombosis (OL): The prevention of venous thrombosis is one of the biggest markets in medicine, and it seems strange now that for decades we got by using nothing but heparin and warfarin. Devilish cunning is now employed to find new ways to interrupt the clotting cascade in such a way as to prevent unwanted thrombosis without increasing the risk of bleeding. A new target is factor XI, and you will be interested to learn that factor XI levels can be lowered with FXI-ASO (ISIS 416858), a 2′-O-(2-methoxyethyl) (2′-O-MOE) second generation antisense oligonucleotide that specifically reduces human factor XI messenger RNA expression in the liver. Well, Isis Pharmaceuticals would like you to be interested anyway, and have persuaded the NEJM to accept what appears to be a phase 2 open label trial of the drug in 300 patients about to undergo unilateral knee replacement, with enoxaparin as the comparator. Their drug had an equal protective effect with less bleeding. But when you are thinking of giving a preventive treatment to millions of healthy people, you need quite a lot more evidence than this.
Lancet 13 December 2014 Vol 384
Ultrathin Strut Biodegradable Polymer Sirolimus-Eluting Stent vs. Durable Polymer Everolimus-Eluting Stent for Percutaneous Coronary Revascularization (pg. 2111): Does the world need new stents? No, but device companies need new products for when current ones go off patent. And the Lancet needs to sell article reprints as part of its stated business plan. But do you, dear reader, really need to read a paper entitled “Ultrathin strut biodegradable polymer sirolimus-eluting stent versus durable polymer everolimus-eluting stent for percutaneous coronary revascularisation (BIOSCIENCE): a randomised, single-blind, non-inferiority trial?” I would suggest not.
December 11th, 2014
Triple-Vessel Disease in an Asymptomatic Man: CABG, PCI, or Medical Management?
Amit Shah, MD, MSCR and James Fang, MD
A 66-year-old, physically active, nondiabetic man with no symptoms was tested for coronary artery calcium (CAC) on the advice of his physician, who was debating whether to start him on a statin for an LDL-cholesterol level of 120 mg/dL. The patient’s CAC score was 2000.
In follow-up, exercise echocardiography was arranged. The patient’s resting heart rate was 77 bpm, and his resting BP was 127/63 mm Hg. He exercised for 7 minutes and achieved 109% of maximum predicted heart rate (169 bpm) and a normal exercise BP. His LV ejection fraction was >55% both before and after the stress test, although during stress he developed mild anterior hypokinesis. He experienced no chest pain during exercise, but the test was stopped because slight (<1 mm) ST-segment depressions were observed.
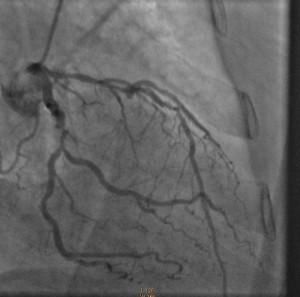
Cardiac catheterization revealed 80% to 90% proximal and mid-stenoses in the left anterior descending (LAD) artery, the left circumflex (LCX) artery, and the right coronary artery (RCA). TIMI 3 flow was noted throughout. The LAD and LCX arteries are shown in the left image below; the RCA is shown on the right.
Patients like this one have not been well studied in clinical trials, but his lack of diabetes, chest pain, heart failure, and functional limitations are positive prognostic signs that negate the severe CAD and coronary calcium burden.
Questions:
1. Given that the main goal is to reduce mortality risk, how would you extrapolate from the current literature to formulate the best plan for this patient? Would any potential mortality improvement from CABG, for example, justify the risks of surgery?
2. High-intensity statin therapy and lifestyle modification have been found to lead to plaque regression. Are these steps sufficient to lead to meaningful anatomical and/or functional changes that would reduce or eliminate any need for surgery? Do you know of any cases in which those steps have been sufficient?
Response:
December 18, 2014
Questions:
1. Given that the main goal is to reduce mortality risk, how would you extrapolate from the current literature to formulate the best plan for this patient? Would any potential mortality improvement from CABG, for example, justify the risks of surgery?
The challenge is to modify this asymptomatic patient’s significantly increased risk for cardiovascular events (as predicated by his CAC and angiographic CAD). Several issues may be underappreciated at first glance:
- Extrapolation from the current literature is difficult because such asymptomatic patients have not been studied in large-scale contemporary randomized trials. In fact, the 1997 ACIP trial suggested that treatment of “asymptomatic ischemia” with revascularization was associated with lower risks for CV events and mortality than was medical management (without a statin).
- The evidence for provokable ischemia by stress testing without symptoms is suggestive of a defective physiologic warning system.
- Revascularization risk in a patient without significant comorbidities is quite modest but quantifiable: <0.5% to 1.0% mortality risk with either CABG or PCI.
Although I support an initial aggressive medical approach (see my NEJM editorial on STICH), close surveillance and acknowledgement of the limitations noted above should be reviewed with the patient. Repeat exercise testing to assess the efficacy of treatment on ischemia would be reasonable as well. Some patients will cross over to revascularization (30% in ACIP); others will elect to be revascularized initially, which I have supported in my practice as well.
2. High-intensity statin therapy and lifestyle modification have been found to lead to plaque regression. Are these steps sufficient to lead to meaningful anatomical and/or functional changes that would reduce or eliminate any need for surgery? Do you know of any cases in which those steps have been sufficient?
In addition to plaque regression, high-intensity statin therapy improves coronary endothelial function and reduces the biologic susceptibility to plaque rupture, a predominant mechanism of myocardial infarction and sudden cardiac death. It is likely that such changes, rather than a reduction in severity stenosis per se, produce the 30% to 40% reduction in cardiovascular outcomes seen in statin trials. Many cardiologists, myself included, have anecdotal experiences successfully managing large-burden CAD with aggressive medical management (but bear in mind that achieving optimal outcomes requires aggressive lipid lowering, treatment of ischemia, optimized management of comorbidities, and close patient surveillance).
Follow-Up:
December 24, 2014
After discussion with his physicians and family, the patient opted for an initial intervention involving aggressive medical therapy and lifestyle changes. He is currently taking aspirin 81 mg, metoprolol 25 mg twice daily, lisinopril 2.5 mg daily, and atorvastatin 40 mg daily — and he undergoes cardiac rehabilitation 5 days per week. He has been a lifelong vegetarian, but in addition he is now reducing his consumption of refined carbohydrates and sugars. After completing cardiac rehabilitation, he will undergo another stress test to assess his functional capacity, symptoms at peak exercise, and ischemia burden.