December 11th, 2014
Triple-Vessel Disease in an Asymptomatic Man: CABG, PCI, or Medical Management?
Amit Shah, MD, MSCR and James Fang, MD
A 66-year-old, physically active, nondiabetic man with no symptoms was tested for coronary artery calcium (CAC) on the advice of his physician, who was debating whether to start him on a statin for an LDL-cholesterol level of 120 mg/dL. The patient’s CAC score was 2000.
In follow-up, exercise echocardiography was arranged. The patient’s resting heart rate was 77 bpm, and his resting BP was 127/63 mm Hg. He exercised for 7 minutes and achieved 109% of maximum predicted heart rate (169 bpm) and a normal exercise BP. His LV ejection fraction was >55% both before and after the stress test, although during stress he developed mild anterior hypokinesis. He experienced no chest pain during exercise, but the test was stopped because slight (<1 mm) ST-segment depressions were observed.
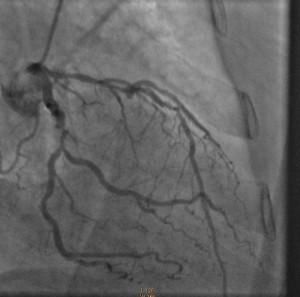
Cardiac catheterization revealed 80% to 90% proximal and mid-stenoses in the left anterior descending (LAD) artery, the left circumflex (LCX) artery, and the right coronary artery (RCA). TIMI 3 flow was noted throughout. The LAD and LCX arteries are shown in the left image below; the RCA is shown on the right.
Patients like this one have not been well studied in clinical trials, but his lack of diabetes, chest pain, heart failure, and functional limitations are positive prognostic signs that negate the severe CAD and coronary calcium burden.
Questions:
1. Given that the main goal is to reduce mortality risk, how would you extrapolate from the current literature to formulate the best plan for this patient? Would any potential mortality improvement from CABG, for example, justify the risks of surgery?
2. High-intensity statin therapy and lifestyle modification have been found to lead to plaque regression. Are these steps sufficient to lead to meaningful anatomical and/or functional changes that would reduce or eliminate any need for surgery? Do you know of any cases in which those steps have been sufficient?
Response:
December 18, 2014
Questions:
1. Given that the main goal is to reduce mortality risk, how would you extrapolate from the current literature to formulate the best plan for this patient? Would any potential mortality improvement from CABG, for example, justify the risks of surgery?
The challenge is to modify this asymptomatic patient’s significantly increased risk for cardiovascular events (as predicated by his CAC and angiographic CAD). Several issues may be underappreciated at first glance:
- Extrapolation from the current literature is difficult because such asymptomatic patients have not been studied in large-scale contemporary randomized trials. In fact, the 1997 ACIP trial suggested that treatment of “asymptomatic ischemia” with revascularization was associated with lower risks for CV events and mortality than was medical management (without a statin).
- The evidence for provokable ischemia by stress testing without symptoms is suggestive of a defective physiologic warning system.
- Revascularization risk in a patient without significant comorbidities is quite modest but quantifiable: <0.5% to 1.0% mortality risk with either CABG or PCI.
Although I support an initial aggressive medical approach (see my NEJM editorial on STICH), close surveillance and acknowledgement of the limitations noted above should be reviewed with the patient. Repeat exercise testing to assess the efficacy of treatment on ischemia would be reasonable as well. Some patients will cross over to revascularization (30% in ACIP); others will elect to be revascularized initially, which I have supported in my practice as well.
2. High-intensity statin therapy and lifestyle modification have been found to lead to plaque regression. Are these steps sufficient to lead to meaningful anatomical and/or functional changes that would reduce or eliminate any need for surgery? Do you know of any cases in which those steps have been sufficient?
In addition to plaque regression, high-intensity statin therapy improves coronary endothelial function and reduces the biologic susceptibility to plaque rupture, a predominant mechanism of myocardial infarction and sudden cardiac death. It is likely that such changes, rather than a reduction in severity stenosis per se, produce the 30% to 40% reduction in cardiovascular outcomes seen in statin trials. Many cardiologists, myself included, have anecdotal experiences successfully managing large-burden CAD with aggressive medical management (but bear in mind that achieving optimal outcomes requires aggressive lipid lowering, treatment of ischemia, optimized management of comorbidities, and close patient surveillance).
Follow-Up:
December 24, 2014
After discussion with his physicians and family, the patient opted for an initial intervention involving aggressive medical therapy and lifestyle changes. He is currently taking aspirin 81 mg, metoprolol 25 mg twice daily, lisinopril 2.5 mg daily, and atorvastatin 40 mg daily — and he undergoes cardiac rehabilitation 5 days per week. He has been a lifelong vegetarian, but in addition he is now reducing his consumption of refined carbohydrates and sugars. After completing cardiac rehabilitation, he will undergo another stress test to assess his functional capacity, symptoms at peak exercise, and ischemia burden.


Yes several cases I have managed conservatively with excellent results. Some have had surgery already and have recurrent stenoses, some have had other comorbidities that increased risk of surgery, some have declined surgery once I have explained the evidence
Yes I have managed some cases only with medication, no surgery because the cases were so complicated that were considered that surgery was a very high risk.
I remember one special case that had triple coronary stenosis, bilateral carotid stenosis and was rejected for surgery, all this about 10 years ago, with medication he is still well, with more than 80 years old.
He did 109% of his predicted heart rate… He did well, cardiac rehabilitation program and OMT is warrant, after at least 6 months should be done another exercise echocardiography… If its better or equal OMT should continue… Otherwise syntax score would be done; if 23, CABG would be an answer… Only in the preferences of the patient
Asymptomatic, non-diabetic, with good effort tolerance, TVD, needs only intensive statin therapy with Life style modification. Noted for any intervention.
No symptoms ,no significant ischemia during supra-maximal exercise test and no LV systolic dysfunction; CABG has no proven benefice over OMT on survival.
I would recommend high-dose statin and active live style and reassess regularily.
Im not sure to be conservative except for the moment and with very close follow up
I would like to know to decide hereditary antecedents kind of stress he sopports in real life and results with invasive or surgical results results at his health
facilities Changing lifestyle is fair but is it always possible in the patients society? Besides one should monitor muscle eventuall muscle complaints with high dose statins for if he develops muscle damage may be less able to exercise
Meanhle ill do a Holter for if he has eventually ventric arrythmia i would consider to be more agressive
3-V CAD: non-diabetic, normal LVEF, good functional capacity, no symptoms. Calls for rosuvastatin, ASA, and other risk-factor modification. This elicits Loeb’s Law of medicine:
1. If what you’re doing is working, keep doing it.
2. If what you’re doing is not working, quit doing it.
3. If you don’t know what to do, don’t do anything.
4. Above all else, don’t let a surgeon touch your patient.
2000C CAC score is very high and suggests this patient is at very high risk for CV events in the (very next?) future.
As Matthew J. Budoff discusses in his excellent editorial (Eur. Heart J) “Progression of Coronary Calcium is not as Predictable as 1-2-3” doi: 10.1093/eurheartj/ehu377. “those with more calcification progression …can be treated more aggressively” So what?
In this case:
N° 1 Who wants to wait for more Agatston score progression?
N° 2 Who would have the nerves of steel to tell the patient ” you have (severe?!) coronary stenosis in all of three vessels but with medical treatment and close follow-up, normally no cardiac events will happen!”? I am not sure I will be able to do so.
N°3 Why coronary angiogram was performed?
One of our colleagues presented a nearly similar case in our last staff:
An asymptomatic patient, CAC 900, coro-scan showed tight stenosis on RCA, confirmed by angiogram… (Single vessel). Without qualms our colleague performed angioplasty and placed an active stent in the same procedure!.
Finally
I am surprised that no one in the discussion suggested any revascularization in your case report.
And to follow to Dr Payne and Loeb’s Law:
“Do not let an invasive cardiologist perform a coronary angiogram!”
Thank you for this very impressive and interesting discussions
I really appreciate the engaged discussion. Of note, most physicians this patient encountered recommended revascularization.
A recent meta-analysis shows mortality benefit (0.80 hazard ratio) from CABG vs. medical therapy – http://www.ncbi.nlm.nih.gov/pubmed/24958153
Nonetheless, this includes older studies in which medical therapy was not as intense, and many patients were symptomatic.
If you take it at face value, however, the reported 20% relative risk reduction in a patient pool with a 30% 10-year risk of death (for example) means that CABG could offer a 6 absolute risk reduction vs medical therapy. The NNT is therefore 17. One may advise such patients, “Your changes are 1 in 17 of this surgery saving your life over the next 10 years.” In this case, the NNT for death is likely higher because medical therapy has progressed and the patient has lower baseline risk. On this other hand, if you include non-fatal events in the outcome of interest, then the NNT is likely lower.
Interesting discussion. Dr. Shah can you tell us what happened with this patient?
Thanks
The main question is “how would you treat him?” but….the first question do we have to do is “why this patient has this type of lesions?”
He has not diabetes or hypertension; he is not sedentary, LDL 120 mg/dL, physically active.
So….which is the cause of his disease?
He has very high levels of Lp(a), for example?
I think we have to search the cause of him disease, because we can treat him, but we have to know what exactly are we will treating.
This is a very interesting case. No risk factors, no symptoms. In the other hand a CAC score of 2000! If we are fighting disease the patient is asymptomatic any interventions will not be appreciate. If we are fighting death the CAC score put him in high risk.
But high risk is a verdict with a sentence? Some people believe the unstable plaques are not so frequent in the high grade obstructions but other believe if you have an important coronary heart disease without any risk factors your Genoma play an important part, if this is the case any interventions will be futile or partial. So the family history is very important but you can have mutation.
If he has any complications trying to help him he will not understand because he was fine before. If you try something invasive and everything goes right he will not appreciate any objective benefice because he was asymptomatic.
My recommendations it is the same OMT, cardiac rehabilitation an close follow up.
But in this case is very important the opinion of the patient and expend time being sure he understand the risk and benefice.
Life is quality, not the life span.
Happy Holidays!
Thanks again for everyone’s comments. The patient is currently weighing his options, but for now has deferred revascularization, and instead doing CR and medical therapy with aspirin, metoprolol, lisinopril, and high dose atorvastatin.
There is no known family history of premature CAD. Nonetheless, he is South Asian, which may place him in a high risk category based on genes.
I was also thinking that perhaps it is prudent to measure other markers in attempt to explain his mechanism of disease. Lp(a) is one possibility; any others?
i would put him on moderate statins, Atorvastatin 20 mg/ day, Metorprolol 50 mg/day & Aspirin 75 mg/day. would advice adequate life style modification to start with continued Physical activity & SOS Nitrates.
the rationale behind is, he is asymptomatic, non diabetic & Physically active, could run on treadmill upto 7 minutes. the Risk of surgery at 66 yrs of age for above individual may balance the benefits, but optimal medical management atleast for 3 months ff by stress TMT & ECHO, is my best bet.
yes, i have few of my patients, who couldn’t avail stenting or CABG, but are doing fine on OMT, with followup as long as 4 years.
I THINK THAT GOOD RESULT FROM CABG IN THIS AGE GROUP WITH IMPROVED MORBIDITY AND MORTALITY.
I find myself confused about this subject’s management to date.
1. Why did we do an echo stress test in this asymptomatic active subject.
2. With an equivically positive stress test, why did we do an angiongram.
We know that heart attacks occur from rupture of plaque (most often non-obstructive plaque). The score of 2,000 translates into a high risk for plaque rupture and therefore a mandate for effective medical management.
As he has no symptoms and is active, I can think of no circumstance whereby we could find a lesion to fix that would improve his outcome. We now know that even in subjects with angina, revascularization does not reduce MI or coronary death.
I propose that the score of 2,000 was the only information needed and effective medical management should be undertaken.
This begs the question as to what we defign as optimal medical management. There seems to be a consensus that high dose statin equals optimal management. With a calcium score of 2,000 the annual risk for a coronary event is as high as 20%. Assuming a 30% reduction in events with statin use (a rather optimistic assumption), his annual risk on high dose statin is still 14% and therefore exceedingly high risk.
I would add a discussion on diet including lots of fruit, vegetables(especially pigmented berries) and beneficial fats such as fish oil, olive oil, tree nuts and avocado. I would place him on low dose aspirin and fish oil supplements.
The use of an ACE or ARB is prudent. I would not use a B-blocker unless BP could not be controlled with an ACE and Ca channel blocker.
I would discuss dental hygiene and advise daily flossing and appropriate Dentist visits.
If he did not tollerate a statin, we would use a bile acid sequestrant, niacin and high dose omega-3.
I would screen for sleep apnea and subclinical diabetes.
Finally I would do a follow up calcium score in one year. The baseline calcium score was of monumental importance in identifying his risk. The follow up score will determine if his risk is managed. In a subject with his level of plaque, there is a 40 fold difference in MI incidence between calcified plaque progression and stability.
The follow up score is very good at encouraging compliance and lifestyle changes.
I currently have 25 patients with cac scores over 1,000 (the highest is 11,000). With the above described management and serial calcium imaging, I have seen 0 heart attacks in this group over the last 5 years. None have angina or any lifestyle limitations due to atherosclerosis.
Although a decade ago, I would have been in the camp that wanted to do the stress imaging and consider revascularization, I now feel that it is a remarkable waste of resources to look for ischemia in asymptomatic active subjects.
This is a great case on several levels. It illustrates a conundrum for which there are no clear well established answers (ideal therapy of an asymptomatic patient with significant coronary artery disease). It also illustrates a collection of wrong decisions that have led to an angiogram after which we are essentially “stuck”.
A. Decision to performing CAC – unclear what the need is/was here. This patient is a diabetic and has a CHD equivalent state. Not sure why the “his physician, who was debating whether to start him on a statin for an LDL-cholesterol level of 120 mg/dL”. He should have been put on a statin period, there wasn’t any clear reason for doing a CAC.
B. Decision to perform stress testing – appropriate in the light of diabetes status and also in the light of high CAC
C. Decision to performing coronary angiography – inappropriate in my opinion. It is not clear what the need is/was here. The stress test did not show extensive “high risk” ischemia and the patient is clearly asymptomatic (assuming the history is correct). The stress test successfully excluded a high risk ischemic state and the evaluation should have ended in aggressive medical therapy. This is precisely the reason why calcium scoring and even CT angiography is widely criticized – patients end up in the cardiac catheterization laboratory for the wrong reason.
D. Decision to revascularization – this is now unclear. On the one hand intuitively the answer is “yes” because we always perceive “fixing blockages” as a “good” thing. Given diabetes and extensive calcific disease probably CABG would probably be the right mode of revascularization. On the other hand, he does not have extensive ischemia to justify revascularization. Plus the patient is asymptomatic. ACIP was an old trial that suggested a benefit but that was in the days before very aggressive statin therapy and as mentioned by others, we all have patients with a lot of coronary artery disease who’ve done well on medications. However, once the coronary anatomy is “known” everyone including the patient is “uncomfortable”. Plus there’s that nagging “medicolegal” issue in which the doctor gets nailed for not revascularizing the patient if a bad outcome happens. So here, I’d have a frank and point blank discussion with the patient and offer both avenues (medications and revascularization and let him decide). The point, however, was that this patient should not have reached the angiography stage at THIS point in time.
Apologies – misread the original case as diabetic instead of non-diabetic. Hence point , i.e., perofrming CAC was appropriate but and still hold
Apologies – misread the original case as diabetic instead of non-diabetic. Hence point A, i.e., performing CAC was appropriate but points C and D and still hold