May 22nd, 2012
iFR: A New Tool to Measure Functional Ischemia
Justin E Davies, MD, PhD, Richard A. Lange, MD, MBA and L. David Hillis, MD
The instantaneous wave-free ratio (iFR) is a pressure-derived index of stenosis severity that does not require adenosine administration. The index was introduced at the 2011 TCT conference and validated by the results of the ADVISE study, published in December 2011. Following a series of presentations at the recent EuroPCR congress, Dr. Justin Davies answers questions about iFR from CardioExchange Interventional Cardiology co-moderators Richard Lange and David Hillis.
Lange & Hillis: Interventionalists are familiar with the use of fractional flow reserve (FFR) to identify hemodynamically significant coronary artery stenoses, but the concept of instantaneous wave-free ratio (iFR) is new. Can you briefly explain iFR and how the measurement is obtained?
Davies: iFR is a pressure wire-based technology for measuring the severity of a stenosis. It differs from conventional FFR in that it does not require administration of an hyperaemic agent, such as adenosine. In practice for interventionalists, the technique is identical to measuring FFR, except that when the pressure wire is advanced beyond the stenosis, the data from five beats are taken at rest, after which an assessment of iFR made.
Lange & Hillis: The validity of iFR depends on the assumption that myocardial resistance during a specific part of diastole (iFR) is similar to the resistance calculated from whole-cycle averaged measurements during maximal hyperemia (FFR). Is this true?
Davies: We know from simple physics that pressure is proportional to flow when resistance is constant (Pressure = Flow × Resistance). Previously it was not possible to stabilize resistance by administering a hyperemic agent without affecting the hyperemic state; this was the measure of achieving stable or constant resistance. Now, with advances in sensor technology and computational processing, it is possible to identify a period of stable and constant resistance during the wave-free period in the cardiac cycle. By not having to rely on an hyperemic agent to stabilize resistance, iFR may be more stenosis specific, because it is less dependent on the response of the microcirculation and myocardium to the hyperemic agents that are widely used.
Lange & Hillis: How well does iFR correlate with FFR?
Davies: Three studies have been performed using the Imperial–Volcano iFR algorithm, and one (Verify) has been performed using the St Jude algorithm (see summary
In the three studies using the Imperial–Volcano algorithm (734 patients from ADVISE, ADVISE-Registry, and the South Korean prospective blinded study), a strong correlation between iFR and FFR is present, the variance is low (around 5%), and the diagnostic accuracy is excellent (94% after adjustment for intrinsic variability of FFR – based on the gold standard DEFER reproducibility data).
In the study using the St Jude algorithm, the correlation was not as good, and the variance was far greater.
Lange & Hillis: An FFR <0.8 is considered abnormal (i.e., indicative of a hemodynamically significant coronary stenosis). What value for iFR is considered abnormal?
Davies: In over 700 patients (3 studies in patients with clinically intermediate stenoses), the cut-point is consistently 0.89 (for FFR, as noted, it is 0.8).
Lange & Hillis: FFR is potentially erroneous in individuals with elevated coronary venous pressure or serial coronary lesions. What is known about iFR measurements in these conditions?
Davies: iFR shares many of the physiologic features of FFR and thus is subject to many of the same limitations. Since it doesn’t require a response to adenosine, it may be less dependent on a response from the microcirculation and myocardium and, therefore, more “epicardial specific.”
Lange & Hillis: Under what conditions is iFR least reliable (atrial fibrillation)?
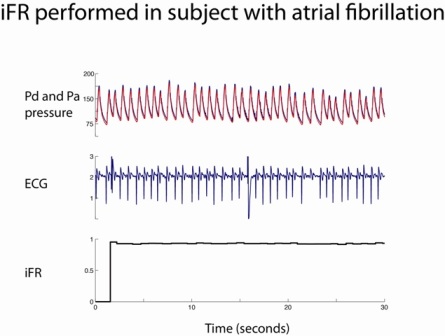
Davies: Our studies involve “all comers” (with the exception of individuals with severe valvular disease). We included patients with atrial fibrillation, ventricular ectopy, etc. The algorithm relies on tracking both the ECG and the pressure waveform, so it is robust; as a result, we can calculate iFR in almost all situations (99.9%). Below is a figure of a patient we saw recently who had atrial fibrillation. You can see that the iFR is very stable, despite considerable variability in the RR interval.
Otherwise, as noted, the limitations are similar to those of FFR (i.e., very small vessels [<2 mm in diameter] and distal territories where flow is very slow [these patients were not enrolled in many of FFR validation studies]).
Lange & Hillis: One of the major criticisms of iFR is that the agreement between the two methods is better for very high, nonsignificant FFR values (>0.85) than for values that indicate hemodynamically significant stenoses. In the clinically relevant range of FFR between 0.60 and 0.90, the correlation between iFR and FFR is rather poor. In what percentage of individual cases would disagreement between iFR and FFR result in reclassification of a stenosis from nonsignificant to significant — and vice versa?
Davies: This is a great question.
The original ADVISE study was an evaluation study; as such, it was designed to test the validity of iFR across a range of physiologic stenosis grades — in a manner similar to the original FFR studies. Clearly, this is not fully representative of a typical patient population. Therefore, we designed the ADVISE-Registry with a simple protocol, and we tested the reliability of iFR in a clinical population. We recruited subjects with angiographically intermediate stenoses. In total, we recruited 312 patients (with 339 stenoses), more than 80% of whom fell within the 0.6–0.9 range. Importantly, however, rather than defining this group by an arbitrary range, we assessed the population with intermediate stenoses seen by all cardiologists daily. Therefore, our results (94% diagnostic accuracy) reflect the patients who are seen every day. We were very careful not to interpret a correlation coefficient over a restricted range assessment, after the recent publication in the BMJ by Bland and Altman. This article specifically cautioned against making any assessment of correlation by reducing range, “Correlation coefficients are a property of the variables and also the population in which they are measured. If we look at a restricted population, we should not conclude that there is little or no relation between the variables because the correlation coefficient is small.”
iFR has a close correlation with FFR and hyperemic stenosis resistance (a pressure and flow-based index) in three studies (800 patients) using the Imperial–Volcano iFR algorithm. The Verify study is an outlier, and it suggests that many of the differences between these studies likely resulted from differences between the Imperial–Volcano algorithm and the St. Jude algorithm. This was perhaps best highlighted by the slides displayed in the Verify presentation, which identified the wave-free period running into the systolic upstroke of the next beat, rather than being restricted to the wave-free window. This difference should not be underestimated, since at this time resistance is highly unstable, and the proportionality of the pressure–flow relationship becomes unreliable.