April 11th, 2012
Anticoagulation Conundrum
Tariq Ahmad, MD, MPH and James Fang, MD
A 75-year-old woman presents to a general cardiology clinic for the first time. She has a history of atrial fibrillation, sick-sinus syndrome requiring a permanent pacemaker, hypertension, and dyslipidemia. She has no specific complaints other than shortness of breath on exertion. Her medications include aspirin (81 mg daily), carvedilol (25 mg twice daily), lisinopril (5 mg daily), and furosemide (40 mg daily).
The woman has just moved in with her daughter, who lives in the area. She helps take care of her grandchildren and buys the groceries for the entire family.
A transthoracic echocardiogram reveals severe left-ventricular hypertrophy and an LV ejection fraction of 45% (atrial fibrillation is consistently rate-controlled). The patient has mild aortic, mitral, and tricuspid regurgitation. A mass detected in the left atrium does not opacify with contrast, suggesting the possibility of a thrombus.
The patient has brought medical notes from previous physician visits, showing that she was hospitalized 3 years ago with a severe headache. She was found to have a subarachnoid hemorrhage that required embolization. At that time, she had an INR in the 2.0 to 2.4 range on warfarin, which was discontinued in light of the subarachnoid hemorrhage.
A year later, the patient was hospitalized with severe bilateral calf pain. A CT scan revealed thrombotic occlusion of the right common iliac and right external iliac arteries. She underwent bilateral iliac and left profunda thrombectomy, with stent placement in the right common iliac artery. After much discussion between the cardiologists and neurosurgeons, the decision was made to re-initiate anticoagulation with warfarin.
Within 6 months after discharge, the patient was readmitted with a massive GI bleed requiring 8 units of packed red blood cells. At the time of this admission, her INR was 2.2. Subsequently, all anticoagulation was stopped. Six months before the patient’s current clinic visit, she had re-initiated aspirin therapy, which she tolerated well.
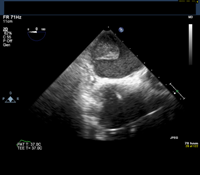
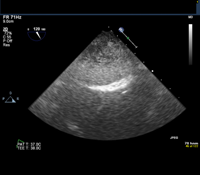
Given this history, the patient is scheduled for an elective transesophageal echocardiogram the day after presenting to the clinic. The images below show the TEE findings: a large 5.5-cm x 2.7-cm heterogeneous multilobulated mass, attached along the posterior wall of the left atrium, which likely represents a thrombus. (Click to enlarge the images.)
Questions:
1. Would you anticoagulate this patient? If so, which agent would you use?
2. Would you perform any further diagnostic testing?
Response:
April 24, 2012
This type of scenario, in which the risks for bleeding and clotting are roughly balanced, is common in clinical practice. The notion that “all bleeding stops” favors anticoagulation (given that stroke is irreversible), but the ultimate extension of that course of action is fatal hemorrhage. This patient has had several life-threatening episodes of both hemorrhage and thromboembolism, so applying traditional risk modeling is not likely to be appropriate.
Discussion of agents other than warfarin in this setting would be largely academic, given that this patient would not be included in a clinical trial.
Unfortunately, an evidence base to inform us here is scant, so we must rely on good old-fashioned common sense, keeping in mind the adage to do no harm. A reasonable empiric approach is an unfractionated heparin “stress test.” Acute bleeding would answer the immediate question of whether to initiate anticoagulation, although this method would be limited in its ability to predict future bleeding. If the UFH is tolerated, I would consider a transition to oral warfarin with an INR target of 2.0 to 2.5. One unifying diagnosis would be amyloidosis, senile or primary.
Finally, I, too, would have tried to get more imaging of the posterior left-atrial mass. However, I have seen this sort of finding after surgical or percutaneous ablations for atrial fibrillation.
Follow-Up:
April 30, 2012
Thank you all for your comments — I wish we had consulted fellow cardiologists in real time. The patient was started on a heparin drip, which she tolerated without any evidence of bleeding. Consistent with a finding of intra-atrial thrombus, she underwent a cardiac CT scan (MRI was not done because of her pacemaker). A diagnosis of amyloidosis was considered and ruled out. The patient was transitioned to warfarin and thus far has done well without any further evidence of bleeding or thromboembolism.

This is surely a complex case. This patient a surely at very high risk for thromboembolic complications. The PVD is just one of the complications. Considering the risk benefit ratio in this perculiar setting I will anticoagulate her with Low molecular heparin and then continue with warfarin with close monitoring of her INR.