September 6th, 2010
What’s at the Heart of This Patient’s Problem?
Anju Nohria, MD and James Fang, MD
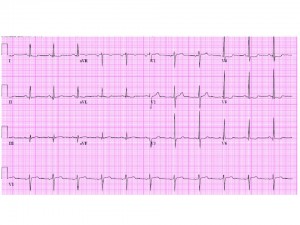
The patient is a 53-year-old lawyer with no cardiac risk factors other than a 70 pack-year history of smoking. He has a known history of diverticulitis with prior gastrointestinal bleeding and presented with lightheadedness and bright red blood per rectum. Initial evaluation revealed a drop in his hematocrit from 43% to 39%. He underwent a colonoscopy the next morning and was found to have multiple diverticula and sigmoid irritation, but no obvious source of bleeding was identified. His initial electrocardiogram is shown below.
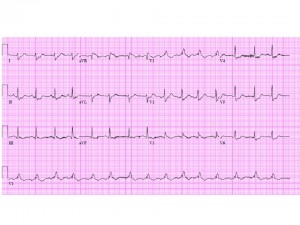
The next day, the patient abruptly bled again and had a further drop in his hematocrit to 29%, with a blood pressure of 85/50 mm Hg and a heart rate of 95 bpm. With this, the patient complained of mild chest pressure, and a repeat electrocardiogram was obtained.

The patient was seen by a surgeon, who recommended an elective partial colectomy. A pre-operative cardiology consult was obtained.
Questions:
- What is this patient’s peri-operative risk?
- Would you recommend any further cardiac evaluation prior to a partial colectomy?
- Would you recommend peri-operative beta-blockade in this patient?
Response
James Fang, MD
This gentleman has developed unstable angina in the setting of hemodynamically significant gastrointestinal bleeding. His perioperative risk is very high by any criteria. I suspect he has severe, life-threatening ischemic heart disease that has been unmasked by his acute medical condition. Although immediate resuscitation with volume and blood products should be the initial strategy, he should undergo urgent coronary angiography to define the extent of his coronary artery disease, so that therapeutic options can be reviewed. The site of his bleeding also remains unclear; once his cardiovascular status is stabilized, a tagged red cell scan or even angiography can be performed to understand the exact nature of his bleeding. Beta blockade is relatively contraindicated in someone with recently stabilized hypovolemic shock.
Part II
Anju Nohria, MD
The patient was transfused with 3 units of packed red blood cells and had a follow-up hematocrit of 32%. Later that night, he became restless, removed his telemetry leads, and was found on the floor in ventricular fibrillation. He was electrically cardioverted and reverted to sinus rhythm, and an amiodarone drip was started. A post-resuscitation electrocardiogram was obtained.
The patient was hypotensive and was stabilized with norepinephrine therapy. An initial creatine phosphokinase returned at 310 U/L, with an MB fraction of 45.3 ng/mL. The troponin I was also elevated at 0.36 ng/mL. Cardiology was urgently called again.
Questions for discussion:
- What additional medical management would you recommend at this time?
- Would you take this patient to the cardiac catheterization laboratory prior to surgery?
- If a significant cardiac lesion was identified, what type of intervention would you recommend?
Response
James Fang, MD
Medical management should include volume and blood resuscitation, as well as definition of the coronary anatomy. The ventricular fibrillation and QRS widening post-resuscitation would be concerning for a large burden of CAD. In light of this patient’s life-threatening GI bleeding, the use of anticoagulants, antiplatelet agents, and even nitrates/beta-blockers is contraindicated until his coronary anatomy is defined. The management of his coronary disease depends on the nature and burden of that disease. The most critical lesion could be treated with temporizing balloon angioplasty. If there is left main and/or severe three-vessel CAD, an intra-aortic balloon pump could be used to stabilize his situation. At that point, other strategies to define his GI bleeding and subsequent therapies could be entertained.
Follow-Up
Anju Nohria, MD
The patient remained hemodynamically stable. His cardiac enzymes continued to rise, with a peak troponin I of 3.85 ng/mL, a peak creatine phosphokinase of 2667 U/L, and an MB fraction of 373.8 ng/mL. An echocardiogram revealed a left ventricular ejection fraction of 50%, with an end-diastolic dimension of 6.2 cm. He had inferior and inferolateral hypokinesis. The mitral valve appeared myxomatous, with a prolapsed anterior leaflet and a fixed posterior leaflet. There was a new posteriorly directed jet of severe mitral regurgitation.
The patient was taken to the catheterization laboratory, where he was found to have multivessel coronary artery disease with 90% left main, 90% mid left anterior descending, 80% proximal left circumflex, and 95% right coronary lesions. His left ventricular end-diastolic pressure was 12 mm Hg with large “v” waves.
He underwent surgical revascularization with a left internal mammary graft to the left anterior descending artery — and saphenous vein grafts to the first obtuse marginal and right coronary arteries. He also underwent mitral valve repair with a Carpentier-Edwards ring and plication of the anterior leaflet.
He did well postoperatively from a cardiac standpoint. He continued to be guaiac-positive but had no frank bleeding. He was discharged home on a proton pump inhibitor and no aspirin or Coumadin.

I believe that his peri-operative risk is high. I would feel better if he had an angiogram prior to his colectomy. If he has anything less than massive ischemia, I would treat medically. If we could get his blood pressure up with blood and hydration I would initiate a low dose of beta blocker prior to surgery.
I think this patient is at very high perioperative risk. Initial ECG shows ST-T abnormalities in a patient with risk factors. Next episode of bleeding unmasks coronatry ischemia which is very significant (and can be considered as a kind of equivalent of stress testing in this case)where the patient should get blood transfusions solving oxygen supply and hypotension as well. Then the patient should have coronary angiogram performed prior to surgery. The second ECG reveals ST elevations in aVR with profound ST depressions in chest leads – this may be the sign of left main disease (septolateral ischemia i.e. LAD plus depression as far as V2 i.e. circumlflex artery) or at least proximal LAD.
The patient with risk factors and symptomatic ischemia docummented by increased ECG signs of ischemia clearly needs an angiogram and intervention besides betablockers started at low dose with uptitration. Betablocker alone will not suffice (unless there is vital indication annd surgery has to be performed as emergency – in that case I would be very afraid of possible MI, and refer the patient to coronary angiogram even if there had been no complications during perioperative period).
1. Any intervention is likely to delay surgery a minimum of 1 month (BMS or CABG) and carry with it a load of anticoagulant and antiplatelet medications (ASA, Plavix, Heparin/Bivalirudin, 2b3a). The combination of the two would make the risk of rebleeding substantial.
2. Trials such as Decrease-V pilot and CARP suggest no benefit to revascularisation prior to non-cardiac surgery. In this case the potential for pLAD and Left main make me concerned but I would be concerned any intervention would do more harm than good.
My approach would be to start with maintaining his BP and Hb (>90) and re-evaluate. If pre-morbid functional status was good (>4 mets) and the evidence of ischemia resolves then I would proceed with OR and deal with the consequences afterwards (once the source of bleeding is controlled).
If he hadn’t had the symptoms and ECG changes after the last bleed, and had pre-op >4 METS capacity he’d have been cleared for surgery. Now he needs a cath since he clearly has ischemic changes at a Hct that they should not appear at. Then you proceed based on the cath results.
I think, I agree with Jason. This patient has serious GI bleeding and is likely to die without urgent surgery. i believe he should be urgently operated after fluid and blood resuscitation. I would avoid beta blockers since they are likely to interfere with body’s compensatory response to hypotension.
Competing interests pertaining specifically to this post, comment, or both:
None
Jason is correct. There is no evidence that revascularization prevents perioperative death or MI, even in “high risk patients. Proceed to GI surgery…CAD issues can be addressed thereafter.
This is a surgical emergency, restoration of volume with some blood then control the haemorrhage is the way to go, I agree with Jason.
Competing interests pertaining specifically to this post, comment, or both:
None
Aortic stenosis with AVMs in the small bowel?
Somebody is forgetting what the urgency of the original surgery was, which basically was elective. His risk of death from possible cardiac source greatly exceeds his risk of bleeding out from his tics. I stick with what I said before, First fix his heart if needed, then his bowel. Didn’t anyone notice he’s a lawyer ????
I agree with Dr. Fang and Dr. Kostek. This patient has high risk of coronary disease. ST segment elevation in aVR and ST depressions in most of the remaining leads worries me for triple vessel or left main disease that has been unmasked by the acute bleeding. I would recommend resuscitation with fluids and blood products as needed in the short term, followed by angiography. I suspect the patient will probably require CABG. Blood and volume can be replenished easier than infarcted myocardium.
Competing interests pertaining specifically to this post, comment, or both:
None.
i agree with dr andrade any cardiovascular intervention implies a lot of anticoagulants , and the risk of bleeding exceeds benefits , i reccomend resuscitation whit fluids and vasoppresors , an intermediate option is to proceed whit a GI angiogram embolization of culprit artery if stabilizes proceed whit cardiac angiogram if not he needs urgent surgery and later fix his heart
1. I would ask the first question, is colectomy an emergent need? From the information given above, I don’t think the surgery is emergent at this point. But hemodynamically significant bleeding mandates not only resuscitation but also closure of tap with tagged RBC scan followed by angiogram/embolization. If bleeding cannot still be controlled by IR guided procedure, surgery is imperative and I would go for it. Though perioperative risk is high, but benefit may marginally outweigh it.
2. Secondly, as I think at this point surgery is not emergently indicated and patient has acute coronary syndrome,patient’s risk of dying of MI is greater. Thus we should evaluate and treat before I will go in for surgery. But how?
Medical – Treatment is limited. I would not give antiplatelet agent or anticoagulation as the risk of bleeding is high. I would not cause B-blockade now as the patient had a recent hemodynamically significant bleeding. However, if he maintains his blood pressure and there is no evidence of bleeding I would err on the side of treating. I would start Statins to keep LDL<70. I will do an echocardiogram and if it shows EF less than 40%, will start on low dose of ACEI.
Invasive- Even if TIMI risk score is high in this patient, the benefit of early invasive therapy will be mitigated by the risk of potential rebleeding. Thus, I would go for PCI, after he is stable.
Since the risk of rebleeding is high, when I recommend PCI, I would recommend balloon angioplasty w/o stenting to avoid the need for dual antiplatelet agents.
Competing interests pertaining specifically to this post, comment, or both:
None
I’m not sure that I agree that this case is “closed.” You discharged a man after CABG and MV repair who also had a recent major GI bleed and has persistent guaiac positive stool with neither aspirin nor Coumadin. As he is in sinus rhythm (I assume), we can probably justify eliminating short-term Coumadin without incurring significant additional risk of stroke, but sending him out without aspirin is another matter. I raise the following questions:
1) Should further attempts have been made to pinpoint the source of bleeding have been made before discharge?
2) If the source of bleeding cannot be identified and treated, which is the greater risk – thrombosing a graft due to the absence of aspirin therapy or an uncontrollable GI bleed if he is treated with aspirin?
My inclination is to give aspirin and risk the recurrent bleed, but I’d like to hear what others have to say.
Competing interests pertaining specifically to this post, comment, or both:
None
I would have gone with the cath first, as they did, but during the procedure, I also would have had a look at his intestinal arteries in order to locate the bleeding source and eventually stop it. Then CABG.