June 24th, 2013
Roller Coaster Path to Approval for Eliquis Uncovered by FDA Documents
Larry Husten, PHD
After the presentation and publication of the pivotal ARISTOTLE trial, the novel anticoagulant apixaban (Eliquis, Pfizer and Bristol-Myers Squibb) was widely expected to be a blockbuster. But then it got bogged down at the FDA where initial hopes for a speedy approval were dashed after highly critical reviews. Approval of the drug was delayed for 9 months past the original deadline as a result of both a Prescription Drug User Fee Act (PDUFA) date extension and a complete response letter from the FDA. Now an article by Sue Sutter in Pharmaceutical Approvals Monthly, based on documents posted by the FDA on its website, offers an inside look at the drug’s roller coaster ride through the FDA.
The article describes in detail the efforts of the FDA to investigate evidence of fraud and dispensing errors in ARISTOTLE. As Sutter writes: “To many looking in from the outside, the apixaban NDA filing seemed like a sure thing.” Initial results of ARISTOTLE suggested that it had “the potential to be best-in-class if the published ARISTOTLE data were to be believed.”
It was not publicly revealed at the time, but the FDA documents now show that the reason for the original 3-month extension of the PDUFA date was serious concerns about trial misconduct in China. According to Sutter, a senior clinical site manager, with another monitor, “altered source records to cover up evidence of good clinical practice violations.” This eventually led FDA investigators to question data from 24 of the 36 sites in China.
Ultimately, the FDA reviewers concluded that the results of the trial were not substantially altered by the problem. Sutter writes: “Thus, while the fraud in China did not derail the apixaban application, it appears to have set the review back by three months and, in the process, highlighted clinical reviewers’ larger concerns about sloppy execution and inadequate sponsor oversight of the pivotal trial.”
A second major problem, and the one that ultimately led to the complete response letter, was that the companies were unable to demonstrate that patients received their assigned medications. This was a potential source of enormous trouble because of the study’s double-dummy design, creating the possibility that patients might have received either both active drugs, putting them at high risk for bleeding, or two placebos, putting them at high risk for stroke.
“Questions surrounding the extent of dispensing errors in ARISTOTLE not only raised concerns about how such errors affected study outcomes, they also led FDA reviewers to question the quality of monitoring and oversight of the trial,” writes Sutter. One FDA official wrote that if the agency had been aware of these errors prior to companies submitting the NDA, “we would have refused to file it.”
Three months after receiving the complete response letter the companies resubmitted the NDA. The FDA reviewers then concluded that the major findings of the trial were valid, leading to approval of the drug on December 28, 2012.
A second article by Sutter examines the controversy over the wording and placement of the mortality finding of ARISTOTLE in the Eliquis label. Although apixaban was associated with a statistically significant reduction in mortality in ARISTOTLE, the marginal result (p=0.047) was not strong enough for the FDA. Writes Sutter: “While Eliquis’ sponsors surely would have liked an Indications statement for reduced all-cause mortality, FDA declined to give apixaban such a competitive advantage over Pradaxa and Xarelto.” Instead, the mortality “information is relegated to the Adverse Reactions and Clinical Studies section of the label.”
Sutter reports that there are strong hints in the redacted FDA documents that Pfizer and BMS “requested a mortality reduction claim as part of the proposed Indications statement for Eliquis.” According to Sutter:
The NDA requested approval of Eliquis ‘to reduce the risk of stroke, systemic embolism, [redacted] in patients with nonvalvular atrial fibrillation,’ according to various review documents. A second line of the proposed Indications statement also is redacted.”
Sutter quotes the FDA reviewers:
‘The mortality finding (superiority for all-cause death) is not nearly as robust as the findings for the primary endpoint and major bleeding,’ the reviewers said, noting that the agency’s statistical reviewer calculated that one less death in the warfarin arm would negate statistical significance for apixaban’s superiority.”
Asked for a response to the articles, Pfizer and BMS sent the following statement:
Bristol-Myers Squibb and Pfizer are committed to achieving the highest level of scientific rigor and adherence to the principles of good clinical practice in all clinical development programs. In response to the Complete Response Letter from the FDA on Eliquis, the companies conducted significant analyses to confirm that although there were medication dispensing errors in ARISTOTLE, the rate was very low and it did not impact the outcome measures of the trial. The questions in the complete response letter were resolved to the FDA’s satisfaction and Eliquis was approved by the agency on December 28, 2012, ahead of the March 17, 2013, resubmission PDUFA date. Bristol-Myers Squibb and Pfizer believe that the FDA approval of Eliquis to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation reflects the strength of the clinical data for Eliquis in this indication.”
Ethan Weiss, a cardiologist at the University of California San Francisco Medical Center, feels strongly that the mortality issue is a red herring. A strong supporter of apixaban, he is most impressed by the safety profile of the drug. The lower rate of intracerebral hemorrhage — the most feared complication of anticoagulant therapy — associated with apixaban in ARISTOTLE means “it is the clear winner.” He wrote me:
To me, the major benefit of this drug is its safety. I am much less impressed by its efficacy, but honestly a drug that is non-inferior to warfarin is all that any of us wanted for a long time. So the most conservative way to look at it is that we have a warfarin replacement that 1) is at least as good as warfarin in terms of stroke prevention, 2) is demonstrably safer in terms of major bleeds (most notably in the head), 3) requires no monitoring, 4) has many fewer drug-drug or drug-food interactions. Put that together and you have a big win.”
June 20th, 2013
Hypertension and Cholesterol Guidelines Delayed Again as NHLBI Gets Out of the Guidelines Business
Larry Husten, PHD
The National Heart, Lung and Blood Institute (NHLBI) will no longer issue guidelines, including the much-delayed and much-anticipated hypertension (JNC 8) and cholesterol (ATP 4) guidelines. Instead, the NHLBI will perform systematic evidence reviews that other organizations, including the American Heart Association and the American College of Cardiology, will use as a resource for their own guidelines.
The exact fate and form of the delayed hypertension and cholesterol guidelines have not yet been decided, though the NHLBI’s Michael Lauer said he was confident that these guidelines would appear in less than a year. But a lot of work remains before the documents can be published. ACC President John Harold said that “the ACC has not formally agreed to or begun the process of updating” the NHLBI documents, “but we are open to this role and look forward to working out details with NHLBI and the American Heart Association.”
The AHA’s chief science officer, Rose Marie Robertson, said “there are no details sorted out about what might happen yet.” She declined to give a time frame for publication of the documents, but noted that “a lot of work has been done already so it’s not the same as starting from scratch.”
The basic work on the NHLBI’s hypertension and cholesterol documents was completed long ago. The delayed release of the documents has sparked considerable frustration and criticism. Many believe the backlash against the USPSTF’s mammography guidelines prompted the NIH and other public officials to avoid making controversial recommendations.
NHLBI director Gary Gibbons explained on the NHLBI website that “the landscape for guidelines development has changed dramatically. More effective strategies and clinical evidence are available to clinicians and patients.” He cited two reports from the Institute of Medicine “that established new ‘best practice’ standards for generating systematic evidence reviews and developing clinical practice guidelines. The reports underscore that these are two distinct, yet related, activities that require careful intersection and coordination.”
In addition to the hypertension and cholesterol guidelines, the NHLBI has been working on guidance for overweight/obesity in adults, cardiovascular risk assessment, and lifestyle modification. (Gibbons and Lauer are also the authors of an article published online in Circulation and the Journal of the American College of Cardiology explaining the new change.)
Both the ACC and the AHA expressed support for the NHLBI announcement. The AHA said it looks forward “to working closely with the NHLBI and other organizations to create evidence-based guidelines that meet the needs of healthcare providers and the public.” The ACC’s Harold said that the ACC “has been in discussions with NHLBI about the planned change in their approach to guidelines. We agree that it makes sense for medical societies like the ACC to take a strong collaborative role in the guideline development process.”
June 19th, 2013
Top-Line Results: No Cardiovascular Benefits Found For Saxagliptin
Larry Husten, PHD
Top-line results of a large phase 4 study with saxagliptin (Onglyza, Bristol-Myers Squibb and AstraZeneca) demonstrate that the drug is safe but has no cardiovascular benefits. AstraZeneca and Bristol-Myers Squibb today announced the top-line results for the SAVOR-TIMI-53 Cardiovascular Outcomes Trial of Onglyza®. The full results are scheduled to presented at the annual meeting of the European Society of Cardiology in Amsterdam on September 2 by Deepak Bhatt.
SAVOR-TIMI-53 randomized 16,500 patients with type 2 diabetes with cardiovascular disease or multiple risk factors to saxagliptin or placebo. The companies said that the trial met the primary safety objective, in that it was noninferior to placebo, but that it did not meet the primary efficacy objective, in that it failed to show superiority to placebo in reducing the composite endpoint of cardiovascular death, nonfatal myocardial infarction, or nonfatal ischemic stroke. Saxagliptin, a DPP-4 inhibitor, is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
Sanford Bernstein analyst Timothy Anderson wrote that saxagliptin will now “join the long list of other oral antidiabetics (OADs) that have similarly failed to show a definitive CV benefit over placebo.” He noted that the press release did not provide any information from the trial about the drug’s effect on the pancreas. The FDA is currently investigating the effects of saxagliptin and other DPP-4 inhibitors due to concerns over pancreatitis and pancreatic cancer.
Additional Resources:
June 18th, 2013
FDA Raises Concerns About the Cybersecurity of Medical Devices
Larry Husten, PHD
The FDA has raised concerns about the vulnerability of medical devices to cyberattack. In one dramatic instance, reported by the Wall Street Journal, a VA catheterization laboratory in New Jersey was temporarily closed after malware infected the lab’s computer devices.
The FDA last week recommended that device companies and medical facilities “take steps to assure that appropriate safeguards are in place to reduce the risk of failure due to cyberattack, which could be initiated by the introduction of malware into the medical equipment or unauthorized access to configuration settings in medical devices and hospital networks.”
Many medical devices are vulnerable to cybersecurity breaches through the internet or other wireless technology or from infected flash drives. The FDA said malware could access patient data, monitoring systems, and implanted devices. Older devices may be highly vulnerable, especially if the manufacturers don’t provide timely security updates or if the devices are not updated by the medical facility or the patient with the device. In many cases the existence of the security threat has not been assessed or recognized.
The FDA said that it is “not aware of any patient injuries or deaths associated with” lapses in cybersecurity or that any “specific devices or systems in clinical use have been purposely targeted at this time.” But cardiologist William Maisel, deputy director of science and chief scientist at the FDA’s Center for Devices and Radiological Health, told the Wall Street Journal that the FDA is “aware of hundreds of medical devices that have been infected by malware… it’s not difficult to imagine how these types of events could lead to patient harm.”
The Journal story mentions a Florida VA hospital in which 104 devices were infected with the Conficker virus, including a GE Precision MPI X-ray machine, a Hologic mammography device, and a Siemens gamma camera for nuclear medicine studies.
Another case involved a GE radiology device at Beth Israel Deaconess Medical Center in Boston that stored mammography images and patient information. After becoming infected when a GE technician connected the device to the internet, the hospital discovered “unexpected network traffic.” John Halamka, chief information officer at Beth Israel, told the Journal: “Seeing a radiology workstation sending data to an outside server is highly unusual.”
Halamka offered some additional perspective on the problem to the Washington Post:
“There’s almost no medical device that doesn’t have a network jack on the back. To fight the evils of the Internet, not only do you have to have a moat, you have to have a drawbridge, burning oil to pour on attackers, and guys with arrows.”
June 18th, 2013
Statin Toxicity Associated with CYP3A4-Inhibiting Antibiotics
Higher rates of hospitalization for rhabdomyolysis occur among patients on statins who also start taking clarithromycin or erythromycin, which inhibit statin metabolism, according to an Annals of Internal Medicine study.
Using provincial databases, researchers examined 30-day outcomes among some 140,000 Ontario residents who were taking a statin metabolized by the cytochrome P450 isoenzyme 3A4 (CYP3A4). All participants were aged 66 or older. Roughly half were starting a prescription for the CYP3A4-inhibiting antibiotics clarithromycin or erythromycin, and the other half were starting azithromycin.
CYP3A4-inhibiting antibiotics were associated with a 0.02% increase in absolute risk for hospitalization with rhabdomyolysis, the study’s primary outcome, compared with azithromycin (relative risk, 2.17). Increased risks for acute kidney injury and all-cause mortality were also noted.
The authors recommend that coprescribing a CYP3A4-metabolized statin (atorvastatin, simvastatin, or lovastatin) and a CYP3A4-inhibiting antibiotic (clarithromycin or erythromycin) “be avoided when possible.”
June 17th, 2013
Selections from Richard Lehman’s Literature Review: June 17th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint selections from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
BMJ 15 June 2013 Vol 346
Associations Between the Organization of Stroke Services, Process of Care, and Mortality in England: Stroke care improvement programmes in the UK seem to work, just as stroke centres did when they were first set up. A prospective cohort study examines the figures and looks for the contribution made by each element of improved care. Once again we get this wretched word bundle, and Bundle 4 is defined as: “patient given antiplatelet therapy where appropriate and had adequate fluid and nutrition for first 72 hours.” Why on earth bundle together adequate food and fluid with antiplatelet therapy? Anyway, this bundle makes the most difference: it is perhaps a marker for units where the nurses have enough time to make sure the patients are fed and watered.
JAMA Intern Med 10 June 2013 Vol 173
Waste and Harm in the Treatment of Mild Hypertension (pg. 956): It’s great to see Iona Heath featured in a viewpoint on waste and harm in the treatment of mild hypertension in a leading US journal. It is taking so long for the entrenched models of thinking about cardiovascular risk factors to give way to a patient centred view of risk and benefit.
June 17th, 2013
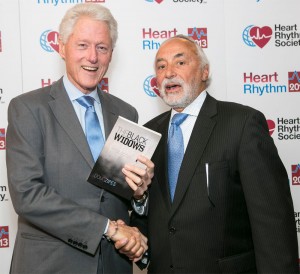
Douglas Zipes: Portrait of the Electrophysiologist as a Novelist
Douglas P Zipes, MD, John Ryan, MD and Harlan M. Krumholz, MD, SM
CardioExchange’s John Ryan and Harlan Krumholz interviewed renowned electrophysiologist Douglas Zipes about his alternative career as a novelist. Zipes is the author of two novels, The Black Widows and Ripples in Opperman’s Pond.
Why and when did you decide to write novels?
Zipes: I began 20+ years ago, after reading a medical thriller by a best selling author, and feeling, “I can do a better job than that.” I have always liked writing and am a good story teller. However, I found out writing fiction was a lot harder than it looked, and totally different from scientific writing. My first novel — co-authored with my wife (long story) — is in a drawer, but it was a good beginning. I then took several fiction writing courses and the first result is The Black Widows. Ripples in Opperman’s Pond followed about two years later.
Finally, at this time of my life, another scientific publication, while always rewarding, does not have the “zing” it once did, while entering into an entirely new venue, where they ask, “Zipes? Who the hell is he?” is a challenge like being an intern all over again.
What is your creative process – how do you do the writing?
Zipes: I write like you drive home at night: you know where you start from, where you have to end up, but your headlights illuminate only 100 yards at a time, and you follow them. You could get to the final target by multiple routes. Sometimes you hit a dead end, and have to try a different road. But the exploration is exhilarating.
For The Black Widows, I basically knew the beginning, since it was a theme I had kicked around in my head for many years, and the ending, which took place in Petra, Jordan, which I had just visited as a tourist. I had no idea how to get from point A to point B, but I knew I wanted my hero chasing a bad guy in the old ruins. I learned that, for me, writing in the first person freed my creative spirit, so I became my hero in the novel.
Ripples in Opperman’s Pond was entirely different. It is based on two court trials in which I was the medical expert. The first was defending a prominent physician being sued by the widow of a famous basketball player who had sudden death. The second trial was as a plaintiff expert in which a prominent pharmaceutical company was being sued for not revealing complications of an NSAID. I put both experiences together and created Ripples. I thought the theme of identical twins — nature v. nurture — would also be fun. And finally, I wanted a memorable opening sentence that people would remember, like, “Call me Ishmail” or “It was the best of times, it was the worst of times…” So, the first sentence (spoken by one of the twins) is, “We were identical, Dorian and I, but not at all alike.”
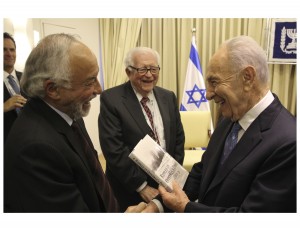
Eugene Braunwald watches while Douglas Zipes gives Israeli president Shimon Peres a copy of his book.
You can always find time for a passion. We love medicine and find time to do all the things we do (ask Harlan!). So, I make time to write. But it’s different than writing an article for Circ/JACC/NEJM in that you can pick it up and work on it for an hour, and then put it down again. I need BLOCKS of time for fiction. I need to get back into the story, become the protagonist, remember whether I said her eyes were blue or brown, etc. It’s a lot harder to re-connect than writing science.
If you were talking to a young Doug Zipes would you tell him to become an electrophysiologist or an author?
Zipes: You’ve got to follow your passion, whatever it is and wherever it takes you. If it’s writing, then do it. Same for medicine. However, you’re more certain of a reasonable lifestyle being a doctor than a writer. Consider: there are about 1 million new titles published annually in the U.S. And there are a lot more writers than doctors waiting on tables in restaurants!
June 14th, 2013
New European Hypertension Guidelines Released with Simplified Blood Pressure Target
Larry Husten, PHD
New hypertension guidelines from the European Society of Hypertension and the European Society of Cardiology were released in Milan today at the European Meeting on Hypertension & Cardiovascular Protection.
 The authors of the guidelines write that “despite overwhelming evidence that hypertension is a major cardiovascular risk, studies show that many are still unaware of the condition, that target blood pressure levels are seldom achieved.” They report that hypertension affects 30-45% of people in Europe.
The authors of the guidelines write that “despite overwhelming evidence that hypertension is a major cardiovascular risk, studies show that many are still unaware of the condition, that target blood pressure levels are seldom achieved.” They report that hypertension affects 30-45% of people in Europe.
Perhaps the biggest change in the new document is the adoption of a single systolic blood pressure target for almost all patients: 140 mmHg. This replaces the previous, more complicated target, which included both systolic and diastolic recommendations for different levels of risk (140/90 mmHg for moderate- to low-risk patients and 130/80 mmHg for high-risk patients). One of the co-chairs of the Guidelines Task Force, Robert Fagard, commented: “there was not enough evidence to justify two targets.”
For the first time the European guidelines join the current trend and specifically grade the level of scientific evidence and the strength of recommendations contained in the document.
The approach to drug therapy for hypertension has also been thoroughly revised. Drugs are no longer suggested for the treatment of high normal blood pressure. No single drug or class is given special preference, since the benefits of treatment are largely based on the blood-pressure-lowering effect of the drugs. The guidelines recommend an individualized approach to treatment, based on clinical and demographic considerations.
The guidelines provide perspective on the much-discussed new technology of renal denervation for resistant hypertension, saying that renal denervation is “promising” but that more trials are needed before it can be fully assessed.
The new guidelines put a greater emphasis on considering hypertension within the context of additional cardiovascular and other risk factors. Home blood-pressure monitoring and ambulatory blood-pressure monitoring also gain an increased role.
In a press release, Giuseppe Mancia, Co-Chairperson of the Guidelines Task Force, said:
“This is certainly the most important current overview to consider the totality of hypertension treatment; it will form the basis of hypertension care for the foreseeable future. The WHO has already recognised hypertension as the leading global risk for mortality in the world, and as we identified in the document, the public needs to be more aware of just how common hypertension is. Not only that, doctors and patients need to recognise that we have good treatments which can control hypertension.”
The much-awaited U.S. counterpart to these guidelines have been subjected to multiple delays, to the frustration of many in the hypertension community.
June 13th, 2013
Too Much, Too Fast? Cross-Country Skiing and Heart Arrhythmias
Larry Husten, PHD
When it comes to exercise, it may be true that you can do too much or go too fast. It might seem counterintuitive, but a new study finds that among cross-country skiers, the risk for having a cardiac arrhythmia is highest in those who race the fastest or most often.
 Although lack of exercise is almost certainly a major contributor to cardiovascular disease, the beneficial effects of moderate exercise may not always be extended with more frequent or more intense exercise. Previous research has raised the possibility that a small number of elite athletes may be at increased risk for heart rhythm and cardiovascular problems.
Although lack of exercise is almost certainly a major contributor to cardiovascular disease, the beneficial effects of moderate exercise may not always be extended with more frequent or more intense exercise. Previous research has raised the possibility that a small number of elite athletes may be at increased risk for heart rhythm and cardiovascular problems.
In a paper published in the European Heart Journal, Swedish researchers report on more than 50,000 participants in the Vasaloppet, an enormously popular 90 kilometer cross-country skiing event that takes place each year in Sweden. Previous research has shown that Vasaloppet participants are, not surprisingly, healthier than other Swedes across a broad range of measures.
With nearly 10 years of follow-up, there were 919 cases of arrhythmia. People who completed five or more races and people with the fastest finishing times each had a 30% increase in the risk for arrhythmia compared with the rest of the participants. Atrial fibrillation and bradyarrhythmias were the most common arrhythmias that occurred. There was no difference between the groups in the risk for the most dangerous, life-threatening arrhythmias (ventricular tachycardia, ventricular fibrillation, or cardiac arrest).
“The present study investigates the higher end of the physical activity level scale and shows how very high physical activity level affects risk of arrhythmias,” said the lead author of the study, Kasper Andersen, in a press release. But, the Swedish cardiologist said, it is “important to emphasize that numerous studies have shown that exercise protects against heart disease and numerous other diseases. Our findings should not deter people from exercising, especially as we did not find any increased incidence of arrhythmias leading to sudden death…. We believe that it is generally safe to prepare for and participate in the Vasaloppet races.”
Andersen was cautious in his interpretation of the data: “These findings suggest there is a dose-response relationship: the more races skiers complete and the faster they go, the greater their risk of subsequently developing arrhythmia. However, it is important to stress that this study does not show that the exercise causes arrhythmias, only that it is associated with an increased risk.”
June 13th, 2013
A Wiki World for Physicians
C. Michael Gibson, M.S., M.D. and John Ryan, MD
CardioExchange’s John Ryan interviews Harvard Medical School professor C. Michael Gibson, founder and editor-in-chief of WikiDoc.org, a “living textbook of medicine” online.
Ryan: Why did you create WikiDoc?
Gibson: Innovation increases as free and open access to information grows. Our mission statement is that “Healthcare is enriched when medical information flows freely.” Traditional textbooks, typically in paper format, are often outdated before they are printed. At best they permit one-way flow of information, with no opportunity for bidirectional exchanges, comments, or reader participation.
Access to traditional print educational content is limited to those who can afford to buy it. The copyrighted material is owned by the publisher and cannot be broadly disseminated or repurposed. Many people now view access to medical information as a right. Although free online content is available, nearly all accessible sites (including society websites) are supported by pharmaceutical and device companies (an exception is the National Library of Medicine).
In late 2005, I created WikiDoc as a free, open-access website that allows an international community of healthcare professionals to “co-create” webpages without requiring that they be familiar with HTML or computer programming. Rather than top-down creation and one-way delivery of content, it is a bottom-up, grassroots, participatory community with bidirectional flow of information. Instead of a vertical organizational structure at a single academic institution, our horizontal structure of co-creation (which we also call “collective genius,” “peering,” or “online collectivism”) has engaged 7082 authors worldwide who have contributed to 200,458 chapters (with 26,625 freely downloadable images) that have been edited 768,180 times.
Our reader-supported site has no funding from pharmaceutical or device companies — and no advertisements. Instead of being copyrighted, the content is legally protected as “copyleft,” which safeguards against control by any individual and ensures free access forever. Visitors can copy, modify, and redistribute the information for their own purposes, as long as the new version grants the same freedoms to others and acknowledges the source or authors of the original content (e.g., parts of this sentence came from WikiDoc).
Our content is increasingly multilingual and organized into “microchapters” that display well on mobile devices, which many healthcare providers in the developing world can access despite being unable to afford print textbooks. The physician and patient content for a given topic are linked together. An overview page is written at the level of a medical student, and the microchapters are written at the level of a subspecialist. There is bidirectional flow of content with Wikipedia, although WikiDoc is targeted at physicians, whereas Wikipedia aims to reach a general readership. Several years ago we launched a sister site, WikiPatient, whose 1200 chapters of content are written at a fifth- to eighth-grade reading level.
About 20 full-time volunteer physicians in Boston curate the content. We meet every morning at 8:30 to set our goals, and again at 4:30 that afternoon to review our progress and address questions. These amazingly dedicated volunteers (our deputy editors-in-chief) labor along with me at night and on weekends. The content is served on Amazon Right Scale, which can recruit an expandable number of servers to scale up as traffic increases. Last month, in 46 hours, the site was visited 4.7 million times (about 2.5 million times daily or 896 million times a year).
Ryan: How do you ensure accuracy on WikiDoc?
Gibson: Traditional textbooks represent the views of highly selected authors. Content on a collaboratively authored site tends to be less biased, as it is based on consensus rather than any individual’s point of view. A discussion page allows a community of writers to openly vet WikiDoc content so that a consensus can be reached. Consensus does have its limitations, lest we forget that the “wisdom of the crowd” once perpetuated the view that the earth was flat and the sun revolved around it. Indeed, it was not until “content experts” like Copernicus, Galileo, and their predecessors were given a voice that the scientific paradigm shifted. Thus, experts have a critical role in moderating the wisdom of the crowd, and our goal is to crowdsource experts. Collaborative authoring on Wikipedia has been shown to be as accurate as Encyclopedia Britannica content or information in a Nature article.
Authors must register via a system that requires a “captcha” to verify they are human, and a team member also reviews their credentials. Prior versions of webpages are stored, and a page can be instantly reverted to any of its previous states if vandalism occurs. WikiDoc authors can choose to be alerted by email when changes are made to a topic that interests them. Only approved users who request permission are allowed to edit drug pages.
Ryan: How have patients responded to the site?
Gibson: Some 57% of patents use the internet to obtain medical information. In the past, doctors were trusted providers who delivered paternalistic, proscriptive information to largely uninformed patients. Guidelines and checklists have represented a great advance, but they tend to deliver one-size-fits-all healthcare. Doctors must now earn the trust of increasingly knowledgeable patients through open dialogue and conversation. Patients now want more-personalized medicine, tailored to both their genome and their envirome (their environmental risk factors). WikiDoc content allows patients to become better-educated consumers of healthcare. For many years, I posted my phone number online, and calls from patients who desired education were some of the highlights of my career.
Ryan: What is the future of WikiDoc?
Gibson: My son is spearheading the creation of board review questions at Harvard Medical School. We are working toward a process of “micro-CME” or “CME on the fly” as physicians access or create content. We hope to provide free content for integration into electronic medical records as part of the health information technology revolution. We have a variety of artificial intelligence initiatives underway and welcome all who would like to get involved. Just email me at charlesmichaelgibson@gmail.com.
Have you used WikiDoc? What are your thoughts about this online venture?