April 20th, 2015
Remembering Kanu Chatterjee
Harlan M. Krumholz, MD, SM
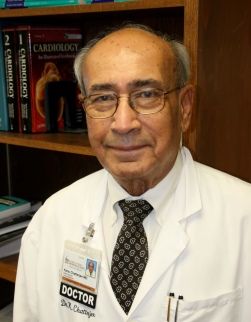 Legendary cardiologist and teacher Kanu Chatterjee passed away last month on March 4th at 81 years old. CardioExchange Editor-in-Chief, Harlan Krumholz, shares memories of his mentor.
Legendary cardiologist and teacher Kanu Chatterjee passed away last month on March 4th at 81 years old. CardioExchange Editor-in-Chief, Harlan Krumholz, shares memories of his mentor.
I have been meaning to write a note about Kanu Chatterjee, but have had trouble finding words that match the man. Dr. Chatterjee (I never felt worthy to call him Kanu – even in later years), a soft-spoken man of great patience, kindness, and wisdom, influenced so many through the wonder of his bedside manner, the brilliance of his mind, and the remarkable incisiveness of his exquisite diagnostic skills. From very modest beginnings – he finished medical school in Calcutta while living in a refugee camp – he rose to become of our nation’s national treasures in medicine.
Rounds with him were a remarkable experience. Every day was a tour de force performance. I would have bought tickets. I would have paid for the experience. I always wanted more. In fact, I chose to do my Chief Residency year at Moffitt Hospital in San Francisco based on the agreement that I could round every day in the CCU with Dr. Chatterjee. It was one of the best decisions I ever made.
Dr. Chatterjee was a master instructor. He would teach at the bedside, in the hall, at the blackboard. We copied the way he approached patients, the way he patiently elicited a history – even the way he wrote. His characteristic drawings of the precordial impulse were artifacts to study and reproduce. When he heard a Dock’s murmur we all strained to listen – and when we failed to hear it, he helped us try again.
He had a wry smile and nothing perturbed him. A call in the middle of the night was always met with a welcoming tone and a reassuring comment. If he came into the hospital at night (he was CCU attending every week of the year except for the rare occasions that he was out of town – and even then he called in every night), he was always in good cheer.
Despite a towering intellect, he had a humility that provided a safe space for questions. He was the ultimate teacher and provided the inspiration for so many to enter cardiology and seek to be like him – which was a destination beyond our abilities, but a very worthwhile goal. When you cared for patients with him you felt you were on holy ground. By his actions every day he honored the profession, respected his patients, and taught us to be doctors. Ask Topol. Or Califf. Or Rumsfeld. Or Masoudi. Or Weiss. Or Pina. Or DeMarco. Or the many, many others whose lives were changed profoundly because they were taught by the Master. We all owe him a debt.
His passing saddens all of us who knew him. I still don’t really have the words to capture his presence and influence. Maybe it is not for words. For those of us who were fortunate to be under his wing, the best we can do is continue our quest to be as good as he was – to care for patients like he did – and to inspire those around us like he did.
April 20th, 2015
Selections from Richard Lehman’s Literature Review: April 20th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
NEJM 16 April 2015 Vol 372
Efficacy and Safety of Alirocumab in Reducing Lipids and Cardiovascular Events (pg. 1489): Your learning task this week is to memorise “proprotein convertase subtilisin–kexin type 9 (PCSK9).” The next big lipid lowering debate will be all about inhibitors of PCSK9, and somebody should urgently invent a popular name for them. I suggest fatins (fat lowering injections), to rhyme with statins. There are two of them at the moment: alirocumab and evolocumab. In this trial, alirocumab was given as an injection every two weeks to two thirds of 2341 patients at high risk for cardiovascular events who had LDL cholesterol levels of 1.8 mmol per litre or more and were receiving treatment with statins at the maximum tolerated dose. The rest had a placebo injection. “At week 24, the difference between the alirocumab and placebo groups in the mean percentage change from baseline in calculated LDL cholesterol level was −62 percentage points (P<0.001); the treatment effect remained consistent over a period of 78 weeks.” The trial was not powered to detect a fall in actual cardiovascular events over this period, but as its name ODYSSEY LONG TERM implies, it means to go on: To strive, to seek, to find, and not to yield. (Last line of Ulysses by Tennyson)
Efficacy and Safety of Evolocumab in Reducing Lipids and Cardiovascular Events (pg. 1500): And now for fatin number two. Evolocumab is a monoclonal antibody that inhibits proprotein convertase subtilisin–kexin type 9 (PCSK9), as you already know: the phrase is already tripping off your tongue. This is Amgen’s answer to Sanofi and Regeneron’s alirocumab, and it has chosen to call its trial OSLER. The effect of the two antibodies seems to be very similar. Again, the early signals point to a substantial fall in cardiovascular events, but only time will tell. This will be a hard fight, but it isn’t clear how big the potential market will be. After all, the real Osler is quoted as saying “The first duty of the physician is to educate the masses not to take medicine.” The statins wars will soon become the fatins wars; and I hereby declare copyright on the word fatin. I am willing to sell this to either drug company for a million dollars. Everyone has their price and mine is very reasonable.
JAMA 14 April 2015 Vol 313
Survival and Outcomes Following Bioprosthetic vs Mechanical Mitral Valve Replacement in Patients Aged 50 to 69 Years (pg. 1435): I have a kind of déja-vu feeling about this report on 15 year outcomes in “nonelderly” patients with mitral disease requiring valve replacement who have been treated with either bioprosthetic and mechanical prosthetic valves. Maybe it’s because I have read too much cardiac outcomes research, or because I am approaching the end of nonelderliness. Anyway, in patients aged 50 to 69 years undergoing mitral valve replacement in New York State, there was no significant survival difference at 15 years in patients matched by propensity score who underwent mechanical prosthetic vs bioprosthetic mitral valve replacement.
Acute Stroke Intervention (pg. 1451): “Acute stroke intervention: a systematic review” is a very good update article because it goes a bit further and wider than simply a systematic review. This is a really fast moving subject, and the necessary rush to get patients assessed and treated means that primary care doctors are not involved except occasionally to ring for a blue light ambulance on behalf of the patient. But it’s an area of interest to everyone, since anyone can have a stroke. The two studies of thrombectomy that I recently commented on are still sitting on the NEJM website, and it’s only a week or two since a paper appeared which should be practice changing in a different way. This describes a computerised decision aid, which can help patients and their relatives make very fast decisions about thrombolysis on an individualised basis. It was developed in Newcastle (UK) and every stroke unit around the world needs to know about it.
April 16th, 2015
Cangrelor Finally Gets Nod From FDA Advisory Panel
Larry Husten, PHD
On Wednesday the FDA’s Cardiovascular and Renal Drugs Advisory Committee voted 9-2-1 to recommend approval of cangrelor during PCI to reduce the risk of periprocedural thrombotic events such as MI, stent thrombosis, and ischemia driven revascularization.
The news follows a decade of efforts to develop the drug — a potent, fast-acting, and reversible antiplatelet agent. After the failure of two large clinical trials, the company finally achieved some success with its phase 3 CHAMPION PHOENIX trial two years ago. But last year the FDA raised questions about the trial and withheld approval until the company performed additional analyses.
The committee spent much of the day trying to determine a role for the drug in clinical practice, since it is now intended for use in ad hoc PCI, in which patients undergoing angiography are found to have obstructive coronary artery disease and undergo PCI in the same session. The data suggest that cangrelor may then be beneficial in patients who have not been pretreated with an oral P2Y12 inhibitor. A big problem, however, is that there is a very wide degree of variation in the use and acceptance of ad hoc PCI. The committee concluded that in the real world setting the benefits of cangrelor, though modest, outweighed the small increase in the risk of bleeding associated with the drug.
The FDA is expected to reach a final decision by June 23.
April 16th, 2015
FDA Approves New Heart Failure Drug
Larry Husten, PHD
The FDA on Wednesday approved ivabradine (Corlanor), Amgen’s new heart failure drug. The drug has been available for several years in Europe, where it is sold by Servier under the brand names of Corlentor and Procoralan.
Ivabradine was approved for the reduction of hospitalization from worsening heart failure. It is indicated for use in stable heart-failure patients who are in sinus rhythm, have a resting heart rate of at least 70 bpm, and who are also taking the highest tolerable dose of a beta blocker. Ivabradine slows the rate of the heart by inhibiting the so-called “funny” current within the heart’s natural pacemaker, the sinoatrial node. The drug received an expedited review under the FDA’s priority review program.
Approval was based on results of the SHIFT trial, published in 2010, which studied 6,558 patients with heart failure who had a heart rate > 70 bpm. After a median 22 months of followup, the rate of cardiovascular death or hospital admission for worsening heart failure was 24% in the ivabradine group and 29% in the placebo group (HR 0.82, 95% CI 0.75–0.90, p<0.0001).
The FDA said that that the most common side effects of the drug were bradycardia, hypertension, atrial fibrillation, and temporary vision disturbance (flashes of light). The FDA said that ivabradine can cause harm to fetuses and that women should not become pregnant while taking it.
In Europe ivabradine has been approved for use for both heart failure and stable angina. In 2014 results from a 19,000 patient stable-angina trial, SIGNIFY, prompted the European Medicines Agency (EMA) to make several recommendations intended to lower the risk of heart problems linked to the drug. Although the overall results of SIGNIFY were neutral, troubling findings occurred in the very large subgroup (more than 12,000 patients) with symptomatic angina. The EMA review concluded that in these patients ivabradine, compared with placebo, had a small but significant increase in the risk of CV death and nonfatal MI (3.4% vs. 2.9% yearly incidence rates) and a substantially higher risk of bradycardia (17.9% vs. 2.1%). The EMA said ivabradine was also associated with an increased risk for atrial fibrillation. SIGNIFY tested a higher dose of ivabradine, but the EMA concluded that the high dose “did not fully explain the findings.”
April 15th, 2015
Diabetes Drugs Get Neither Restrictions Nor Endorsements from FDA Committee
Larry Husten, PHD
Two diabetes drugs survived a meeting of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee on Tuesday. Rejecting recommendations from critics that the drugs should either be withdrawn or get new restrictions on use, the committee voted against any harsh measures, recommending only that information from two neutral clinical trials be added to the drugs’ labels.
The two trials were the first large large cardiovascular outcomes trials of any diabetes drugs. SAVOR-TIMI 53 studied saxagliptin (Onglyza, AstraZeneca), and EXAMINE studied alogliptin (Nesina, Takeda Pharmaceuticals). Both trials were neutral, finding no evidence of either cardiovascular benefit or cardiovascular harm with the drugs, which are DPP-4 inhibitors.
In the morning, the committee voted 13-1-1 that saxagliptin had an acceptable cardiovascular risk profile. In the afternoon, it was alogliptin’s turn, and the drug sailed 16-0 through the committee on the CV risk profile question. The committee also voted that new safety information from the trials be added to the labels of the drugs.
But new diabetes drugs are not yet completely out of danger. In its briefing documents, FDA reviewers raised concerns about a possible increase in death with the drugs. Panel members were unable to find any consistency in the data and did not seem concerned, but they did express fears about another looming issue. A consistent signal for heart failure complications — which were not directly studied in SAVOR and EXAMINE — has not been easy to dismiss. Panel members called on the FDA to get companies to study the heart failure question more closely.
The next big event in the field will be the presentation in June of the TECOS trial, a 15,000-patient cardiovascular outcomes trial studying sitagliptin (Januvia, Merck). The results will add a substantial amount of new data about cardiovascular outcomes, including heart failure, with DPP-4 inhibitors.
For now, though, the diabetes drugs appear to have dodged a bullet. But as one panelist observed, there is an important lingering question about these and other diabetes drugs. Without any evidence of cardiovascular benefit, the panelist said, “the diabetes community needs to demonstrate that lowering HbA1c is beneficial.” No one expects a prompt solution to that problem.
April 14th, 2015
Study Adds to Evidence Linking Divorce and MI
Larry Husten, PHD
A new study shows that after a divorce, people have an increased lifetime risk for myocardial infarction. Although previous studies have found that MIs occur more frequently in people who are divorced, this is the first study to prospectively examine the lifetime relationship between divorce and MI.
In a paper published in Circulation: Cardiovascular Quality and Outcomes, Duke University researchers analyzed data from a nationally representative cohort of 16,000 adults who were followed from 1992 to 2010. The increased risk for MI among the divorced was not explained by other social, psychological, or physiological factors that have been shown to influence MI.
“Contrary to expectations and existing literature, we found that losses of income and health insurance, and increases in depressive symptoms, alcohol use, and smoking, did not account for the excess risks attributable to a history of divorce in men and women,” the authors wrote. “We suspect that the acute and chronic stress associated with divorce may have played an important role in our findings for both sexes.”
The strength of the association was similar to that of established risk factors like smoking, diabetes, and high blood pressure. The findings suggest that the strength of the link between MI and divorce is comparable to the link with job loss and unemployment.
The findings were different for men and women. Men who divorced and remarried did not have an increased MI risk, but remarried women had an increased risk comparable with women who remained divorced.
April 13th, 2015
Selections from Richard Lehman’s Literature Review: April 13th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
NEJM 9 Apr 2015 Vol 372
Randomized Trial of Primary PCI with or without Routine Manual Thrombectomy (pg. 1389): The major trials of coronary artery thrombus aspiration for myocardial infarction are TAPAS, TASTE, and TOTAL. Think of a bar crawl in Seville. The TAPAS and TASTE are obvious, and TOTAL could refer to the bill, which is sometimes just chalked on the surface you’re leaning on, or to your state of inebriation after eight glasses of fino sherry. Either way, these bars are more interesting than this procedure, which is now ready for burial as a routine intervention for MI. Both TASTE and TOTAL find that it does not improve cardiac outcomes and TOTAL finds an increase in stroke. The accompanying editorial thinks it may yet prove of benefit to high-risk patients, citing observational follow-up and post-hoc subgroup analysis. Maybe one further trial needed in such patients before saying ADIOS to the bartender. But why does cardiology come up with so many failed hopes? It seems so obvious that sucking out a clot as soon as it has blocked a coronary artery will be of benefit, but it just isn’t. Even procedures we believe in, like timely percutaneous intervention for MI, aren’t having the impact we hoped for. The editorial also points out that, “Although door-to-balloon times have improved significantly over the past 10 years, in-hospital mortality for STEMI has remained virtually unchanged.”
Surgical Ablation of Atrial Fibrillation during Mitral-Valve Surgery (pg. 1399): Now let’s move on to mitral valve surgery and atrial fibrillation. It seems clear we can fix this with a mixture of plumbing and electrical engineering. It gets quite sophisticated: “We randomly assigned 260 patients with persistent or long-standing persistent atrial fibrillation who required mitral-valve surgery to undergo either surgical ablation (ablation group) or no ablation (control group) during the mitral-valve operation. Patients in the ablation group underwent further randomization to pulmonary-vein isolation or a biatrial maze procedure. All patients underwent closure of the left atrial appendage.” The primary end-point of the trial was abolition of AF, and by that criterion it was a success, with twice as many in the intervention group remaining free from AF at the end of year. But more than twice as many (21.5%) of the intervention group need to have a permanent pacemaker fitted. “Establishing the effects of ablation on long-term survival, stroke incidence, the need for rehospitalization, repeat rhythm procedures, and freedom from anticoagulation therapy requires further study.”
April 9th, 2015
Selections from Richard Lehman’s Literature Review: April 9th
Richard Lehman, BM, BCh, MRCGP
CardioExchange is pleased to reprint this selection from Dr. Richard Lehman’s weekly journal review blog at BMJ.com. Selected summaries are relevant to our audience, but we encourage members to engage with the entire blog.
NEJM 2 April 2015 Vol 372
Outcomes of Anatomical vs. Functional Testing for Coronary Artery Disease (pg. 372): In English nursery rhyme, it is traditional for a Duke to have 10 000 men. Here is a trial from Duke University that recruited 10 000 men and women, and allowed in a further three for extra measure. These 10 003 recruits were those “whose physicians believed that nonurgent, noninvasive cardiovascular testing was necessary for the evaluation of suspected coronary artery disease.” That is a fate which befalls a staggering four million Americans every year. These people were randomised to be investigated either by coronary computed tomographic angiography or functional testing, which in almost every case meant exercise ECG. I struggled a little with some of the figures, but I broadly agree with the conclusion: “In symptomatic patients with suspected CAD who required noninvasive testing, a strategy of initial CTA, as compared with functional testing, did not improve clinical outcomes over a median follow-up of two years.” But I do just wonder how many of these people really “required” testing in the first place.
Oh, the PROMISE trial of Duke,
It had 10 000 men;
They marched them up on a treadmill test,
Or they scanned their arteries then.
And when they were clear, they were glad,
And when they were blocked, they were down,
And when they were only halfway blocked,
They were neither glad nor down.
Nobody knows the meaning of the original nursery rhyme, and I’m not sure I know the meaning of this trial either.
“Demographic and Epidemiologic Drivers of Global Cardiovascular Mortality (pg. 1333)”: That’s the kind of topic the Lancet is good at dealing with—much better, it turns out, than the NEJM. You need a big long article with lots of charts that you can play with. And it should be open access too: I thought the Bill & Melinda Foundation insisted on that. But this over compressed, under illustrated piece is behind a paywall. And you’re not missing much if, like me, you are interested in the age and social class distribution of cardiovascular disease in individual countries and what may lie behind these. I’m aware that there are numerous intriguing paradoxes, but this article doesn’t have the detail to help you find or understand them. A missed opportunity.
JAMA April 2015 Vol 313
Efficacy of Folic Acid Therapy in Primary Prevention of Stroke Among Adults With Hypertension in China (OL): A Chinese trial in people with elevated blood pressure raises the intriguing possibility that supplemental folic acid may reduce stroke. They recruited over 20 000 adults and gave them enalapril alone or enalapril plus 0.8mg of folic acid and followed them up for a median 4.5 years. The absolute risk reduction for first stroke between the groups was 0.7%, which on an individual level seems trivial: but if you look at this from a long term population perspective, this 20% reduction in relative risk might result in millions fewer strokes in China. This calls for replication in different populations. And is one more reason to put folate in bread, or rice.
JAMA Intern Med April 2015 Vol 175
Primary Results of the Patient-Centered Disease Management for Heart Failure Study (OL): Next week I’ll be putting my head above the parapet and giving a couple of short talks at Evidence Live. One of them will be about how we try to fit patients to the evidence and the outcomes we want: it is so much simpler than seeing how much of the evidence actually applies to each individual and corresponds with the outcomes they want. My illustration will be heart failure. The median age of patients is 76 or more, they have other illnesses—including whatever caused their heart to fail—they are tired and scared. They know they are going to die, most probably from pulmonary oedema, and many of them have experienced how distressing and protracted that can be. The majority would rather have better symptom relief than a longer life. And they want a place of comfort and safety when they die, not rushed treatment in a noisy ward where they are just another old person with HF. One way to tackle this would be to provide them with patient centred disease management at home, and this was the laudable aim of John Rumsfeld’s PCDM trial reported here. But the terse conclusion reads: “This multisite randomised trial of a multifaceted HF PCDM intervention did not demonstrate improved patient health status compared with usual care.” It is laudable that the authors chose this as their primary outcome measure and stuck with it. Had mortality been the criterion, this trial would have been a success. And levels of depression were significantly lower in the intervention group. Let’s build on this great work and see if we can do better. We owe it to these millions of people ending their lives in distress.
The BMJ 4 April 2015 Vol 350
Precision Medicine to Improve Use of Bleeding Avoidance Strategies and Reduce Bleeding in Patients Undergoing PCI: The curmudgeonly old fart in me bridles at the phrase “precision medicine,” but on reflection it is an aspiration that I share. And seeing John Spertus’s name on this paper is a guarantee that at least this one is going to be good. The only time I ever saw patients immediately after percutaneous coronary intervention was when they came to me with big groin haematomas. Bleeding after PCI is a problem that lends itself to precision medicine, because you can calculate personalised risks using the Patient Risk Information Services Manager (ePRISM). So in your highest risk patients, you try to avoid the groin and go into the radial artery instead, and use bivalirudin and perhaps a closure device. I leave the details to any interventional cardiologists who are reading this. And this strategy did reduce bleeding when it was adopted, although “Marked variability between providers highlights an important opportunity to improve the consistency, safety, and quality of care.” Cardiologists, honestly.
April 9th, 2015
Association Between Shorter Height and Heart Disease Largely Explained by Genes
Nicholas Downing, MD
The “well-established” link between shorter adult height and increased risk for coronary artery disease (CAD) is largely explained by height-associated genetic variants, researchers conclude in the New England Journal of Medicine.
Using data from genome-wide association studies, the researchers examined the relationship between 180 height-associated genetic variants and CAD among 65,000 cases (adults with histories of myocardial infarction, coronary revascularization, or angiographic coronary disease) and 128,000 controls. These variants have previously been shown to explain roughly 10% of the variation in adult height.
Overall, for each 1-standard-deviation decrease in genetically determined height, there was a 13.5% increase in CAD risk. Higher LDL cholesterol and triglyceride levels were also found to be associated with shorter height, but they accounted for only 30% of the observed relationship between height and CAD. Accordingly, the authors attribute much of the association to “shared biologic process that determine achieved height and the development of atherosclerosis.”
April 9th, 2015
Digoxin Use in Afib: Revisiting Data from ROCKET AF
Manesh R. Patel, MD
The CardioExchange Editors interview Manesh R. Patel about his research group’s retrospective analysis of data on digoxin use among patients with atrial fibrillation in the ROCKET AF trial. The study is published in The Lancet.
CardioExchange Editors: Please recount your study design and main findings.
Patel: In a retrospective analysis of the ROCKET AF trial, we looked at the use of digoxin at baseline and outcomes. We stratified patients by the presence or absence of heart failure presence and did several types of analysis to account for possible bias, including multivariate adjustment and propensity analysis. After the adjustments, digoxin was associated with significantly increased risks for all-cause mortality, vascular death, and sudden death.
Editors: How does this add to the other recent articles on this topic?
Patel: Some recent reports have noted a possible hazard with digoxin. We found that a significant number of patients with atrial fibrillation (with or without heart failure) were treated with digoxin in the ROCKET AF trial. In fact, we found that some patients with atrial fibrillation were treated with digoxin before other rate-control agents. What we add to the available literature is that ROCKET AF had data on blindly adjudicated events, including CV death, sudden death, MI, stroke, and bleeding. Digoxin increased the risk for CV death and sudden death without the other events. Note that this was a retrospective, non-prespecified analysis with many possibly confounding factors.
Editors: In your article’s discussion section, you stop short of calling for a moratorium on the use of digoxin for patients with atrial fibrillation. Given your findings, the findings of others, and the absence of trial support, why do you think that digoxin use should not be suspended for these patients?
Patel: We believe, as we wrote in the discussion, that the question for clinicians should not be whether digoxin is harmful. That would be hard to answer absolutely without a large randomized trial of the drug in patients with atrial fibrillation. However, we say that even if you think our analysis contains bias from unmeasured factors for which the adjustments cannot account, it is still unlikely that digoxin yields a clinical improvement for patients. So for patients with atrial fibrillation (with or without heart failure) who require rate control, many other alternatives (such as beta-blockers or calcium-channel blockers) should be considered before digoxin. Furthermore, we know that digoxin is a poor rate-control agent.
Editors: What do you tell your patients who are on digoxin for atrial fibrillation?
Patel: I tell patients with atrial fibrillation without heart failure that is it not clear that digoxin is helpful, and we often stop it and use other rate-control therapies. For patients with heart failure and low blood pressure, where other agents cannot be used, we will consider digoxin. But aside from these caveats, I am not using digoxin or recommending it specifically for atrial fibrillation. My colleagues in heart failure may still use digoxin to help with long-term management, but that is a separate discussion.
JOIN THE DISCUSSION
How do the findings from Dr. Patel’s study affect your view of digoxin use in patients with atrial fibrillation?
