February 28th, 2011
What is the Role of CV Screening Tests in Medicine and Legislation?
Larry Husten, PHD
Three papers in Archives of Internal Medicine scrutinize the role of cardiovascular screening tests not only in medicine but in legislation. In the first article, Nicholas Wald and Joan Morris introduce a new interactive tool that determines the detection and false-positive rates of screening tests. The authors illustrate the value of the tool with the examples of CRP, coronary calcification, glycated hemoglobin, and the QRISK score.
In an accompanying editorial, Thomas Wang writes that the tool “illustrates just how poorly most risk markers perform as screening tests.” He notes the inherent limitation of most screening tests, since “use of these tests requires that the screening threshold be set so low that most who screen positive for events will never have one, or so high that most cases of disease will be missed.”
In a separate commentary, Amit Khera discusses the “broad implications” of a 2009 Texas law mandating insurance coverage for imaging tests used for CV screening. Khera writes that the bill was passed based on input from the controversial Society for Heart Attack Prevention and Education (SHAPE), with no input or support from the AHA or ACC, and with no basis in evidence derived from randomized and controlled clinical trials. “The added costs and potential risks of these imaging tests necessitate a higher level of evidence before considering a broad legislative mandate,” Khera writes.
In an editor’s note, Rita Redberg writes that “at a time when states are facing crises in health insurance spending and cutting lifesaving treatments, and when Texas leads the nation in the percentage of residents without health insurance, it is remarkable that Texas has chosen this path.”
February 27th, 2011
Examining an Ad for a Platelet-Inhibition Test
Harlan M. Krumholz, MD, SM
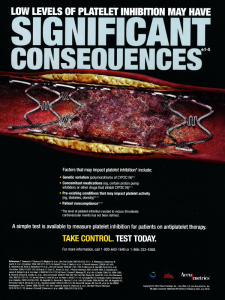 I’ve recently seen in medical journals an advertisement that features an image of a clot within a stent and this headline in all capital letters: “Low Levels of Platelet Inhibition May Have Significant Consequences.” The final two words, “Significant Consequences,” are in a very large font, and the entire ad has an ominous black background.
I’ve recently seen in medical journals an advertisement that features an image of a clot within a stent and this headline in all capital letters: “Low Levels of Platelet Inhibition May Have Significant Consequences.” The final two words, “Significant Consequences,” are in a very large font, and the entire ad has an ominous black background.
Below the image is a bulleted list of “factors that may impact platelet inhibition”: genetic variation, concomitant medications, pre-existing conditions, and patient noncompliance. Each bullet point ends with numbered footnotes, with references appearing at the bottom of the ad.
The ad then asserts, “A simple test is available to measure platelet inhibition for patients on antiplatelet therapy.” In a larger font is the exhortation “TAKE CONTROL. TEST TODAY.”
The ad is jointly copyrighted by Daiichi Sankyo, Inc.; Lily USA; and Accumetrics. Accumetrics makes the test, and the two other companies co-developed and sell prasugrel, which inhibits platelet aggregation.
This ad clearly implies that testing for platelet inhibition is a strategy that reduces the risk for stent thrombosis. But is that really true?
What We Know
Studies have shown that thienopyridines (including clopidogrel and prasugrel) are antagonists to the P2Y12 adenosine diphosphate receptor, which is involved in platelet aggregation. As described in a 2010 ACCF/AHA clinical alert, clopidogrel is an inactive prodrug that must go through several steps to be transformed into an active metabolite. This change is mediated by the hepatic cytochrome P450 system. The relationship between clopidogrel and platelet aggregation varies among individuals, related to genes that regulate the cytochrome P450 system. In contrast, prasugrel is oxidized to its active form in a single CYP-dependent step, and its ability to inhibit platelets seems unrelated to genetic profiles associated with reduced function of the cytochrome P450 system.
What We Do Not Know
No study has shown that a strategy guided by platelet aggregation testing produces better outcomes for patients. We know that a head-to-head comparison of clopidogrel with prasugrel in the TRITON-TIMI 38 study showed that prasugrel recipients had a slightly lower risk for cardiovascular events and a slightly higher risk for major bleeding, but the participants were not selected based on platelet-inhibition response to the drugs. The investigators have not published a study showing the results stratified by genetic profile or response to the drugs. Although platelet aggregation can predict outcomes, it is not known whether using a drug that is more consistent in its platelet inhibition will be better to reduce risk for adverse events. We know that some drugs seem to be superior because of their mechanism of action but fail to actually improve patient outcomes. So although it appears logical to use a test to select a drug that is successfully inhibiting platelet aggregation, the evidence to close that loop does not exist.
The aforementioned 2010 ACCF/AHA clinical alert states clearly: “The evidence base is insufficient to recommend either routine genetic or platelet function testing at the present time.”
I wish that information were also in large capital letters in the ad.
February 25th, 2011
FDA Approves Azilsartan Medoxomil (Edarbi) for High Blood Pressure
Larry Husten, PHD
The FDA has approved azilsartan medoxomil (Edarbi, Takeda) for the treatment of high blood pressure. The new angiotensin II receptor blocker (ARB) will be available in 80 mg and 40 mg doses. The recommended dose is 80 mg once daily. The 40 mg dose is used in combination with a diuretic.
The FDA said that, in clinical studies, azilsartan medoxomil was more effective than valsartan (Diovan) and olmesartan (Benicar) in lowering 24-hour blood pressure.
In a separate development, Takeda announced yesterday that it had submitted an NDA for a fixed-dose combination of azilsartan medoxomil plus chlorthalidone.
February 24th, 2011
Study Probes BMI-Associated Risk in Asia
Larry Husten, PHD
The association between BMI and the risk of death in Asia is mostly similar to that seen in people of European origin, but there may be some important differences between populations, suggesting that being underweight may be a more potent risk factor than being overweight in Asia. In a large pooled analysis including more than 1.1 million people in 19 separate Asian cohorts, Wei Zheng and colleagues found a U-shaped curve among East Asians in which the lowest risk of death was found in people with a BMI in the range of 22.6 to 27.5. Risk was elevated by as much as 1.5 times in East Asians with a BMI over 35 and by as much as 2.8 times in those with a BMI of 15 or lower.
However, among Indians and Bangladeshis, high BMI was not associated with an excess risk of death, although the association with low BMI remained significant. In the discussion section of their report in the New England Journal of Medicine, the authors note that “socioeconomic status could confound the association between BMI and the risk of death, since in less well-developed countries, people with a high BMI are more likely to have a high socioeconomic status (and thus better access to health care) than are those with a lower BMI.”
The authors concluded that “overall, the risk of death among Asians, as compared with Europeans, seems to be more strongly affected by a low BMI than by a high BMI.”
February 23rd, 2011
Air Pollution and Cocaine Among MI Triggers Analyzed in Lancet Study
Larry Husten, PHD
Air pollution is a weak cause of MI, increasing risk by only 5%, but because so many people are exposed to polluted air the population effect is quite large. By contrast, cocaine increases MI risk by 23 times, but does not have nearly as large an effect on the population. These are two of the key results from a study published in the Lancet. The authors analyzed data from 36 epidemiologic studies and calculated population attributable fractions (PAF) in order to perform a comparative risk assessment of multiple MI triggers.
Here are the calculated PAFs:
- traffic exposure: 7.4%
- physical exertion: 6.2%
- alcohol: 5.0%
- coffee: 5.0%
- air pollution: 4.8%
- negative emotions: 3.9%
- anger: 3.1%
- heavy meal: 2.7%
- positive emotions: 2.4%
- sexual activity: 2.2%
- cocaine use:0.9%
- marijuana smoking:0.8%
- respiratory infections: 0.6%
The authors concluded “that acute effects of both participation in traffic and exposure to particulate matter air pollution are substantial contributors to the triggering of myocardial infarction in the population. Improvement of the air we breathe is a very relevant target to reduce the incidence of this disease in the general population.”
In an accompanying comment, Andrea Baccarelli and Emelia Benjamin call the study “an exemplary piece of epidemiological work that furthers our understanding of myocardial infarction triggers. Their work stands as a warning against overlooking the public health relevance of risk factors with moderate or weak strength that have high frequency in the community.”
February 23rd, 2011
High Pacemaker Insertion Rate Observed After CoreValve TAVI Implantation
Larry Husten, PHD
One-third of patients who underwent transcatheter aortic valve implantation with the CoreValve device required a permanent pacemaker within 30 days, according to a report published online in Circulation. Researchers in the UK examined data from 243 patients who received the CoreValve device. The incidence of LBBB was 13% prior to the procedure and 61% afterward.
Patients who had periprocedural atrioventricular block, balloon predilatation, a larger device, interventricular septum diameter, and a prolonged QRS duration were most likely to require a pacemaker.
The rate of pacemaker implantation in patients who have received the Edwards-Sapien valve has been much lower, according to the authors. They speculated that the greater need for pacemakers after implantation of the CoreValve device may be due to “the precise position of the valve within the aortic root,” so that the skirt sits “directly adjacent to the LBB.”
Electrophysiologist Westby Fisher joked on his blog that the requirement for permanent pacemakers could represent a “new annuity” for electrophysiologists.
February 22nd, 2011
Study Finds Nitroglycerin Improves Bone Density
Larry Husten, PHD
A new study raises hope that nitroglycerin may help stem the rising tide of fractures in the elderly. Earlier research with nitrates had suggested the possibility of benefit in this area. Now, in a paper published in JAMA, Sophie Jamal and colleagues report the result of a single-center, double-blind, placebo-controlled trial of 243 postmenopausal women randomized to either nitroglycerin or placebo applied at bedtime.
After 2 years, nitroglycerin significantly increased bone density in the lumbar spine, femoral neck, and total hip compared to placebo. Major adverse events occurred equally in both groups, but headaches occurred more frequently in the nitroglycerin group.
The authors concluded that their findings suggest that nitroglycerin might reduce fractures and note that “nitrates have a potential advantage of easy administration as an ointment, patch, or pill and wide availability of generic preparations.”
In an accompanying editorial, Sundeep Khosla writes that the study “should set the stage for an adequately powered, larger study using nitroglycerin ointment with fracture as an outcome. If such a study demonstrates efficacy for reducing fractures, clinicians would have a novel and inexpensive therapy for osteoporosis.”
February 22nd, 2011
Study Links Stent Thrombosis to Circadian Variation
Larry Husten, PHD
Circadian patterns have long been known to influence the cardiovascular system, resulting in early morning peaks in blood pressure, heart rate, and certain hormone levels, as well as an increased risk for MI and sudden cardiac death. Now, in a study published in JACC: Cardiovascular Interventions, Karim Mahmoud and colleagues have found that coronary stent thrombosis is more likely to take place in the early morning hours. Using the Mayo Clinic Percutaneous Coronary Intervention Registry, the team identified 124 patients with definite stent thrombosis and a known date and time of symptom onset.
Peak incidence for stent thrombosis occurred at 7 AM; the association was significant only in the 49 patients with early (0 to 30 days) stent thrombosis, not in those with late or very late stent thrombosis. The researchers found no association with the day of week, but did observe a higher incidence of stent thrombosis in the summer, which they speculated may have been related to increased activity.
“The most practical implication of these study results is that it may be of benefit for patients with coronary stents to take their antithrombotic medication in the evening (rather than in the morning) to prevent nadir levels of medication during the hazardous morning hours,” said Mahmoud, in an ACC press release.
