February 12th, 2014
Case: Cardiorespiratory Arrest Requiring Intubation in a Patient with Diastolic Heart Failure
Saurav Chatterjee, MD and James Fang, MD
A 65-year-old African American woman with a history of hypertension, diabetes, and seizure disorder is brought to the ED via emergency medical services for respiratory distress requiring intubation. Two weeks earlier she was hospitalized for an exacerbation of acute diastolic heart failure; a transthoracic echocardiogram at that time documented an LV ejection fraction of 60% with inferolateral hypokinesis. Her current medications are amlodipine, metformin, and lamotrigine.
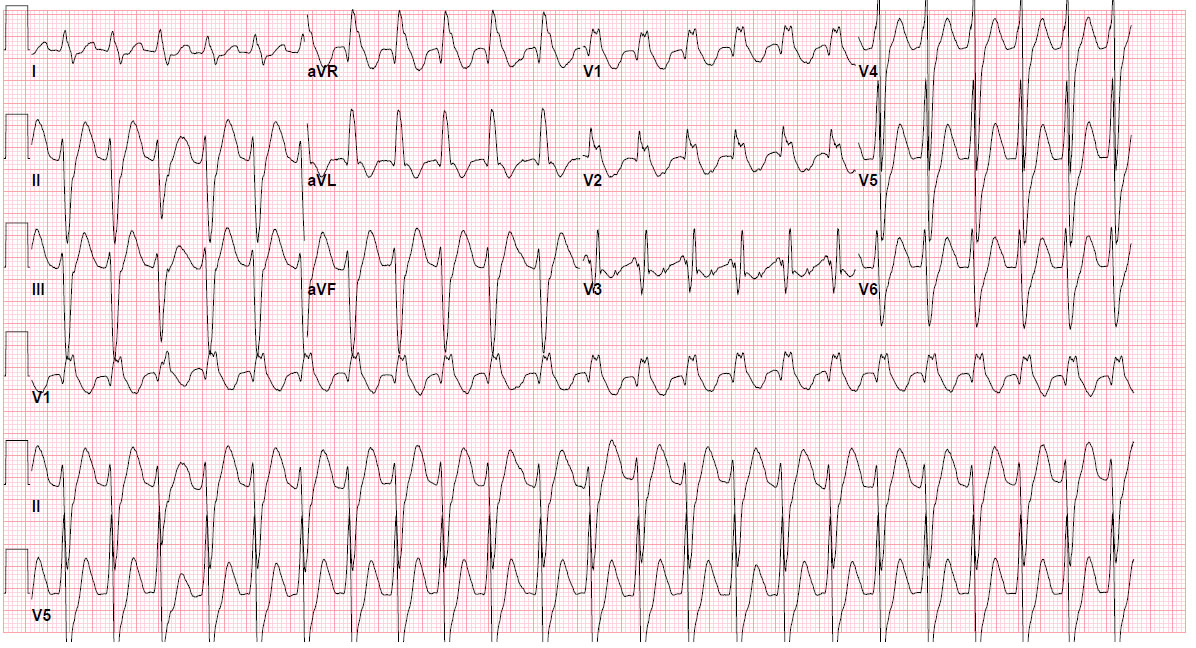
On her current arrival at the ED, she develops pulseless electrical activity requiring CPR for 5 minutes, after which circulation returns spontaneously. She has a heart rate of 122 beats per minute, a blood pressure of 112/74 mm Hg, and a ventilator-assisted respiratory rate of 14 breaths per minute. The patient is intubated but arousable, has diminished breath sounds, and has no murmur on cardiac examination. Her electrocardiogram is shown here:
Questions:
1. What does the electrocardiogram show?
2. What treatment would you recommend next?
3. Should the patient undergo cardiac catheterization? If so, why? If not, why not?
4. Should hypothermia be used in this situation? Explain your answer.
5. How does the patient’s neurologic status influence your decision?
Response:
James Fang, MD February 21, 2014
1. What does the electrocardiogram show?
In the setting of a wall-motion abnormality on echocardiogram (e.g., underlying heart disease), this wide-complex tachycardia (at least 120 ms to my review), RBBB-type, should be considered ventricular tachycardia (or an accelerated idioventricular rhythm due to heart rate) until proven otherwise, although atrioventricular dissociation is not apparent. However, the slow heart rate increases the temptation to consider this either sinus tachycardia or supraventricular tachycardia with aberrancy (e.g., RBBB). Using the Brugada criteria, a diagnosis cannot be made definitively without resorting to morphology of the QRS complexes, which suggests slow VT or accelerated idioventricular rhythm. A definitive diagnosis requires slowing the ventricular response to discern atrial activity and/or having documentation of the tachycardia’s onset.
2. What treatment would you recommend next?
Intravenous amiodarone would be reasonable in this setting until the diagnosis is clear. If the patient remains stable, a beta-blocker could also be considered. Synchronized cardioversion with adequate sedation would also be reasonable if the blood pressure is unstable or other signs of instability are apparent.
3. Should the patient undergo cardiac catheterization? If so, why? If not, why not?
In the setting of CAD risk factors (e.g., hypertension, diabetes) and a wall-motion abnormality on echocardiogram, CAD should be excluded. The patient’s episode of acute diastolic heart failure may have been related to dynamic mitral regurgitation in the setting of the inferior ischemia. Other etiologies, including pulmonary embolism, should also be considered in the differential diagnosis. An echo showing acute RV strain and/or PE protocol chest CT would be a reasonable test in the ED as well. Catheterization is not necessary emergently but should eventually be performed as part of the patient’s cardiovascular evaluation if an alternative diagnosis is not made.
4. Should hypothermia be used in this situation? Explain your answer.
Hypothermia is not necessary. Despite her PEA arrest and being intubated, the patient is arousable and not comatose.
5. How does the patient’s neurologic status influence your decision?
Her almost immediately arousable state suggests that the anoxic insult has been limited and would not therefore attenuate an aggressive approach to diagnosis or therapy. Her presentation was life-threatening and needs a diagnosis.
Follow-Up
February 27, 2014
It was decided that emergent catheterization would have a prohibitive level of risk for the patient. After extensive consultation with the attending physician and the patient’s family, an attempt was made to offer the patient the best possible chance at neurological recovery, by inducing hypothermia with surface cooling to 33°C. A CT scan ruled out acute intracranial pathology.
The patient was successfully cooled and then rewarmed, but unfortunately she never regained a meaningful level of consciousness. Brain imaging conducted at that time revealed diffuse neuronal injury, for which the cause was unclear given that the reported downtime of the patient was just a few minutes. Seven days after admission to the CCU, the family decided to proceed with terminal extubation, after multiple neurologic evaluations indicated that her prognosis was dismal.

What does the electrocardiogram show?
Absence of concordance throughout the chest leads
Long QT interval
R to S interval < 100 mseg.
In V3 it has a notch that it could correspond to a P wave (retrograde vs AV block) this notch has the same rate than the QRS so is very probable they are associated.
Morphology in V 1 – 2 is a RBBB-like with a qR complex in V1 and in V2 a Rr' or notch wave = Marriott's sign but if you see all the complex and alteration in the repolarization, it could be a variant of Bugada like morphology.
Apparence in V6 is a RS complex with a R/S ratio < 1 in the presence of LAD.
aVR has a dominant terminal R' following a QS wave
The QRS in this EKG are very wide but most of the broadening is in the terminal portion of the QRS.
The last two characteristics of the EKG are compatible with a sodium channel blocking toxicity like in tricyclics antidepressants and lamotrigine is also a sodium channel blocking. I would like Brugada special chest derivations.
If the Brugada derivations are compatible with sodium channel blocking toxicity I would start sodium bicarbonate, hyperventilate, magnesium, and avoid Ia and Ic anti arrhythmic, b blockers and amiodarone.
Should the patient undergo cardiac catheterization?
If the patient had elevation of enzymes and echocardiographic alterations I would consider catheterization after the patient is stable.
Should hypothermia be used in this situation?
The majority of evidence using hypothermia was on patients with ventricular fibrillation arrest and continuing loss of consciousness. Evidence on other patients is limited. Other consideration is the experience using lamotrigine and hypothermia, in the context of lamotrigine toxicity you could increase the degree of the sodium channel block.
How does the patient’s neurologic status influence your decision?
The majority of evidence is in continuing loss of consciousness patients so the neurological status is a factor.
RBBB morphology with LAD, consistent with Belhassen VT ie fasicular VT likely posterior fasicle. Tend to respond to CCB and/or adenosine.
Thanks for the exciting brain storming and pushing readers up to their top limits.
Regarding the ECG it shows a wide complex tachycardia ..in lead II I think and I might be wrong that complex number 3 is a fusion beat which tells that patient is suffering of Vtac after her recovery from cardiac arrest.I think whether ECG shows or doesnt show changes consistent with Vtac in a patient with underlying cardiac disease it should be considered as Vtac and treated as VTac as treating a Vtac with Supravent arrythmias treatments (BB/CCB/Digoxin)would be catastrophic.
Adrenaline injections are used in management of PEA and which in addition to hypoxia , acidosis and electrolyte imbalances could cause transient arrythmias which might be serious like this case..searching for and correcting the correctable ones would be important at least to prevent reccurence.
The patient suffered a PEA cardiac arrest which suggest a correctable factor which might be hypoxia , electrolyte imbalance , massive myocardial infarction or massive PE but rapid recovery without measures like thrombolytic therapy or calcium injections to combat hyperkalemia or magnesium injections to combat hypomagnesemia suggests that the reason is probably hypoxia.
Regarding VTac therapy I think lidocaine/Amiodarone will be helpful to control Vtac and revert it to sinus rhythm and prevent its recurrence ..Amiodarone is more effective…if that step fails or haemodynamic deterioration occurs …synchronized cardioversion. Checking for hypokalemia and hypomagnesemia and evidence of myocardial injury is important.
Therapeutic hypothermia improved neurological outcome of outside hospital survivors of cardiac arrest who suffered VTac /Vf and were unarousable after CPR ..whether this can be extrapolated to those arrested in hospital and those arousable after CPR I wish to know more about it if any of colleagues read about recent data on this topic.
Forgive me for spelling mistakes and for my long reply and I will be very happy to hear your comment Dr/ Chatterjee, and Dr/ Fang as well as comments of all colleagues