January 5th, 2015
Screening Heart-Failure Patients for Cognitive Impairment at Discharge
Eiran Gorodeski, MD, MPH
The CardioExchange Editors interview Eiran Gorodeski about his research group’s study of cognitive-impairment screening for patients who are hospitalized for heart failure. The study is published in Circulation: Heart Failure.
CardioExchange Editors: Please summarize your main findings for our readers.
Gorodeski: We used a brief cognitive-impairment test — the Mini-Cog (three-word recall and clock-draw test) — to screen 720 consecutive older adults who were hospitalized for heart failure (HF) at Cleveland Clinic. Nearly a quarter of this population performed poorly on the Mini-Cog, thereby meeting criteria for cognitive impairment. Poor performance on the Mini-Cog was associated with significantly elevated adjusted risks for all-cause rehospitalization and all-cause mortality.
CardioExchange Editors: When and how did you start to think about this study?
Gorodeski: Several years ago, a group of us (a cardiologist, a geriatrician, and home-care specialists) decided to collaborate on a care-transitions and telehealth program intended to reduce rehospitalizations for HF. As the cardiology lead, I assumed that many of the patients would be readmitted for HF decompensation and, as such, designed the program to focus on decompensation monitoring and intervention. We regularly reviewed our efforts and program outcomes and discovered that most of the readmissions were unrelated to HF.
At first I found this very irritating. How could we reduce readmissions if HF exacerbations were not the cause? Our home-care nurses shared many anecdotes about homebound older adults who had insufficient support and were struggling to understand their medical condition and complex treatment regimens. They described patients who were completely unable to execute even seemingly simple tasks, such as organizing their medications. Our geriatrician co-lead suggested that cognitive impairment could be a common denominator, and we decided to implement routine Mini-Cog assessment for all patients entering our program.
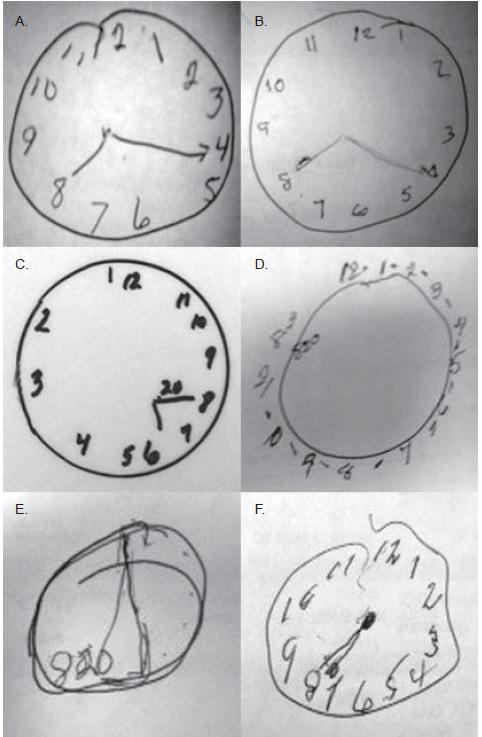
When we saw the grotesque-looking Mini-Cog clocks that some of our patients were drawing in the hospital, often showing the wrong time or with other grossly incorrect features, we realized that an image is worth a thousand words.
Here are clocks drawn by several patients that are featured in a recent Circulation tweet:
We asked our nurses to photograph the clocks with their iPhones and upload the images into the EMR so that other team members could view the misdrawn clocks, not just the Mini-Cog score. We did this for several years as part of routine clinical care, and then we went back to assess the cognition data more formally. That is how the study began.
CardioExchange Editors: What does this study mean for physicians? Should doctors be assessing cognitive function for all patients at discharge?
Gorodeski: I think that doctors should view cognitive function as a “vital sign,” like blood pressure and pulse rate. This ultra-short screening test, which takes fewer than 3 minutes to perform, can be completed by any clinical personnel. Knowing what I know now, I would say that cognitive function in patients with heart failure is probably a more important predictor of short- and intermediate-term outcomes than any of the traditional vital signs.
I also now realize that cognitive impairment is subtle and could be missed frequently if not formally assessed. Physicians’ ultra-brief interactions with HF inpatients on daily hospital rounds are probably insufficient to help us understand their cognitive function. I have seen many patients who smile and greet me in a seemingly normal fashion, but when I challenge them with the Mini-Cog, they exhibit poor recall and fail to draw a clock appropriately. I hope that our study will draw attention to the high prevalence of cognitive impairment in patients hospitalized for HF — and to the fact that its presence could be a sign of impending danger and should not be ignored.
Finally, the Mini-Cog may be a more powerful readmission risk-prediction tool than any existing risk models we have, which is really mind-boggling. This has to be studied further.
CardioExchange Editors: How should management be changed for patients with mild to moderate cognitive function?
Gorodeski: I suspect that we can use the Mini-Cog assessment to guide resource utilization. To achieve better outcomes, patients with cognitive impairment are likely to need a structured care environment and engaged caregivers. In our study, cognitively impaired patients who were transferred to skilled nursing facilities had better outcomes in the short run, compared with cognitively impaired patients who were discharged home. That is probably because of the facilities’ highly structured environments.
Interestingly, in our study, “plain vanilla” home care did not seem to make a difference for cognitively impaired patients who were discharged home. I suspect that those patients need more-intensive daily supervision and assistance than what routine home care currently provides. I am hopeful that such intensive, home-based interventions can be designed, because ultimately patients desire most to be at home, and that is where they do best. In contrast, HF patients who are cognitively intact may not need intensive hands-on interventions; “light touch” telehealth monitoring for early disease decompensation may be more appropriate and helpful.
CardioExchange Editors: Do you have any plans for a next study in this area?
Gorodeski: My immediate plans are to raise awareness about cognitive impairment and about its value as a “vital sign” for patients served by the cardiology and broader healthcare community. I have started doing this by tweeting images of clocks drawn by cognitively impaired HF patients who were in our study. I also plan to work toward routinely screening the cognitive ability of patients hospitalized for HF at my home institution.
Many questions related to cognitive impairment in heart failure need to be studied further. I am most interested in whether and how cognitive impairment fluctuates during acute and post-acute hospitalization for heart failure, how to utilize cognition as a vital sign along with other markers of risk for readmission, and whether any novel models of post-acute care can specifically help this population of patients. This timely and exciting area of investigation may be best addressed in a multidisciplinary fashion.
JOIN THE DISCUSSION
How does Dr. Gorodeski’s research affect your interest in screening hospitalized heart-failure patients for cognitive impairment? View more examples of the clocks at http://www.eirangorodeski.net.

We have found CI to be both the most prevalent risk factor and strongest correlate of 30 day readmissions (Ketterer et al., Psychosomatics 2014,
54(6). doi:10.1016/j.psym.2013.06.019). Preliminary results (as yet
unpublished) demonstrates that Cognitive-Behavioral psychoeducation w patients/families reduces early readmissions by 35%.
Respiratory, cardiac and renal insufficiency we recognize and treat. Cerebral insufficiency becomes apparent when the patient is exposed to stress, and in the worst situation can proceed to delirium, which is an ominous sign. Dr. Gorodeski and his co-workers are to be commended for their bottom-to-top research, trying to detect and roughly quantify their patients’ cognitive capacity, which affects the prognosis in any type of “somatic” illness. Unfortunately, we have no effective cure, and few resources, to mitigate the problem of cognitive decline. We will be forced to address this issue in the decades ahead, and this study is a step in the right direction.