September 11th, 2012
Advertising That Falls Short — Part 1: Omega-3 Fatty-Acid Supplements
Harlan M. Krumholz, MD, SM
Lately I’ve been pondering the impact of advertisements on the public’s knowledge, and I’ve decided to start a series of posts about some that trouble me.
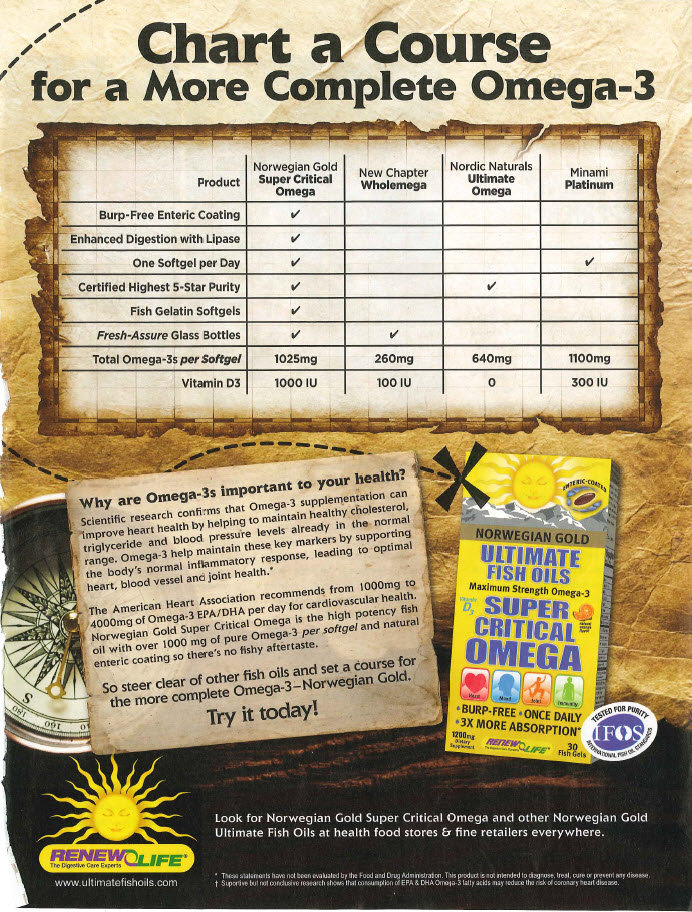
This week JAMA published a meta-analysis showing a lack of evidence that omega-3 fatty-acid supplements reduce the risk for heart disease (confirming an Archives of Internal Medicine meta-analysis from earlier this year). The ad below, created by a company called RenewLife, appears in the October 2012 issue of Yoga magazine.
The ad’s purported focus is to explain why omega-3 fatty acids are important to your heart health — specifically, according to the ad, that they help to maintain “healthy cholesterol, triglyceride, and blood pressure levels already in the normal range. Omega-3 helps maintain these key markers by supporting the body’s normal inflammatory response, leading to optimal heart, blood vessel, and joint health.”
What’s lacking in this message is that these supplements do not improve patient outcomes. The ad does refer to an American Heart Association recommendation from 2003: “For patients with documented CHD, the AHA recommends ≈1 g of EPA and DHA (combined) per day” — with an emphasis on dietary intake.
However, outcomes trials of omega-3 supplements have, overall, failed to show a benefit in preventing heart disease. The possible reasons for that failure are many, and future research might identify an effective dose and formulation. But, for now, a lack of proven benefit is the state of the trial evidence — and that is the message that the public should hear.
What is our role as clinicians in putting ads like this in context for patients?

Our duty is to distinguish the measurable biological effects of any agent(intervention)that is legally permissible to be advertised, from that which is known to be efficacious for disease prevention and/or treatment of any agent(intervention). And, that is a lot to know and explain! Furthermore, an AHA recommendation from 2003- how old is old, outdated,and superceded?
I agree that these ads are misleading. But then again so are ads for Charles Schwab- my investments (if I had any!) are not likely going to grow as much as they say on the ads. However there are two differences here (1) People are accepting of the fact that there is a risk attached to investments and acknowledge that they may not be successsful (2) The disclaimers in the financial industry are such that it seems more difficult to blame/sue investors for failure. So should medical advertisements be viewed differently? I am not sure of the answer.
I think the best we can do is to ask our patients what OTC products including vitamins, etc., they are ingesting, and to have read widely enough that we can tell them of possible dangers (viz. Vit. E) as well as lack of benefits (milk thistle does not benefit patients with liver disease, OTC products have not been shown to help patients with Alzheimer’s Disease). The Medical Letter generally has one or two issues a year devoted to these products.
Harlan, there are a couple of logic flaws in your argument. Lack of evidence for benefit is not the same as proving lack of benefit. For an industry that continues to do stress tests and stenting despite the evidence of lack of benefit but criticizes omega-3 producers because of a lack of evidence of benefit is hypocrisy at its best.
First off, the fact that the meta analysis failed to demonstrate a value by no means proves that there is no value. Meta analyses are considered a poor substitute for a prospective randomized trial. Reaching any conclusion from a meta analysis other than the need for more studies is foolish and a major over-reach.
There are prospective studies such as JELIS, DART, and GISSI-Prevenzione trial showing a significant benefit in subjects randomized to omega-3 fatty acid. There are also a multitude of observational trials demonstrating a correlation between high consumption of fish oil derived omega-3 and reduced coronary disease.
In addition, there is a substantial wealth of bench research showing the role of omega-3 in the production of anti-inflammatory substances, improvement in HDL cholesterol, reduction in triglycerides, improvement in LDL particle number and improvement in mood which could be protective with respect to coronary disease development.
I reject your conclusion that there is no role for fish oil derived omega-3 fatty acids in coronary prevention and treatment. I suggest you expand your literature review and pass judgement more slowly on producers of fish oil derived omega-3 fatty acids.
Till AHA comes up with a new recommendation people will go on using the old recommendation.
I get my patients to declare each and every supplement and OTC they take. I then systematically dissect with them, in evidence-based fashion, the harms and lack of efficacy of most of the products they take. For indeed there are reported randomized trial derived harms for folic acid, vitamin E, vitamin C, vitamin A, L-arginine, Magnesium, vitamin D, calcium and many other “nutraceuticals”. We walk through each trial and supplement together. Many assumed that because it was “natural” it was safe. Nothing could be further from the truth.
Great comments. I know that there are still aficionados of supplements – and no meta-analysis will convince everyone – and for any given patient it is impossible for an average effect to exclude the possibility of benefit. However, when we are talking about treatments for prevention – so not for symptoms – but to prevent future events – the question is: what evidence of benefit do we need before making recommendations. Is plausibility enough. Are open-label trials enough? Is our stance more toward use until proven useless – or be cautious until shown beneficial? I tend to be cautious as I have found that we are not always correct in our expectations of the effect that many of these medications/supplements have.
To answer the above questions:
1) Open-label trials are not enough as there are much empiric data showing they exaggerate benefit and minimize potential harms.
2) Drugs should be considered guilty until proven innocent – at least in terms of safety, but I believe in terms of clinically important endpoints as well.
Finally, I would argue we can do a tremendous amount in terms of lifestyle modification (look at STARS and Lyon Heart Trial for examples), before we need to resort to a cornucopia/pharmacopia of supplements, and particularly in primary prevention, before we need to start everyone on metformin, ramipril and atorvastatin. I have seen marked diminution in risk factor burdens while weaning off such medications in patients who I am doing dietary counselling with (have seen it in myself as well).
Dr. Blanchet,
You are right that “no evidence of effect” is different from “evidence of no effect” –this is known to all. But the question is whether we should remain indifferent when an intervention, advertised widely for the public, has not consistent proof of benefit.
And your remark about (elective) PCI overuse is widely discussed everywhere, including in CardioExchange. And if you are confident about lack of evidence regarding stress testing –I’m not familiar with that literature –best is that you to write a blog or other piece about it, rather than criticizing why omega-3 supplements are questioned in the current blog.
A meta-analysis of smaller trials is not as helpful as a well-conducted RCT with the same total number of patients. Again, this is a simple known fact. But dismissing the finding of meta-analyses is very crude. “When it is not in our power to follow what is true, we ought to follow what is most probable -Descartes”.
I agree that future studies can confirm whether omega-3 supplements are helpful in a distinct subset of patients (people). However, for now, selective reporting of the evidence could be problematic. While you cite some positive studies, I wonder if you also recall the large negative trials, such as the Alpha-Omega, ORIGIN, OMEGA, and SU.FOL.OM3 to name only a few.
Bench research is fantastic –but for hypothesis generation not for clinical practice, especially in a setting where we have comparative effectiveness data available. Haven’t we learnt enough that our reductionist interpretations of mechanistic relationships fall short of truth, more often than not? I think we received the answer with COURAGE, HOPE2, ILLUMINATE, PALLAS and many other trials.
Dr. Bikdeli,
I cannot argue with your logic however the trials you chose to prove your point should be further illuminated.
“While you cite some positive studies, I wonder if you also recall the large negative trials, such as the Alpha-Omega, ORIGIN, OMEGA, and SU.FOL.OM3 to name only a few.” You reference these trials as though they were definitive. Further evaluation shows otherwise.
Alpha-Omega: This study used a very low dose of omega-3. Only 400 mg of omega-3 in the form of 20gms of margarine spread was used. Compliance with such a study should be questioned. The potential interaction with other fats in the margarine spread makes this study a poor example for your point. The dose of omega-3 is almost homeopathic.
ORIGIN: This study still used a modest amount of omega-3 but less than the dietary consumption in countries such as Japan with lower incidence of vascular disease. Only 900mg of omega-3 was used however the “placebo” was 1 gm of olive oil. As there is reason to believe that olive oil might be beneficial in coronary disease, this study again should be questioned. A large concern should be that this study was performed in 573 centers from 40 countries which makes accuracy of reporting next to impossible to validate.
OMEGA: Again, this study is flawed by using a relatively low dose of omega-3, 1 gm, with a “placebo” of olive oil 1 gm.
SU.FOL.OM3: This study used only 600 mg of omega-3 in a complex pool of multiple other B vitamins.
In most of these studies, although not reported, I am assuming that many of the subjects were on high does statin therapy. It is possible that although with low dose statin therapy in Jelis, the 1,700mg of EPA was associated with a reduction of events, it is very possible that high dose statin therapy interferes with the benefit from omega-3 fatty acids.
When the NIH puts together a study looking at at least 2 gms of DHA plus EPA omega-3 in a patient population not on high dose statin therapy, I predict that we will see a dramatic reduction in coronary disease events. As the “neurtaceutical” industry is targeting exactly this population, I think it is likely they are doing people good.
Unlike the statin industry, there are no companies poised to make billions of dollars a year off of selling fish oil. We will never see the likes of the mountain of statin trials available. As a consequence, we may forever need to rely on epidemiology, biochemistry, and a few small, well conceived studies.
It does trouble me that centers of excellence such as Boston and New Haven are publicly stating that fish oil has no value based upon the quality (or lack there of) of the studies upon which that conclusion is based.
I would not agonize too long on trying to determine if some commercial enterprise is really making money on a basis of scientifically sound theory, – or not, – or whether they got their facts right. They are not selling science or evidence. They are selling a fairytale of “happily ever after”. A fairytale of medicating patients out of their lifestyle. Which is futile. Always was, and (most likely) always will be.
Which does not mean that some enterprising people/doctors will not be able to make a quick buck (or a few millions) on selling this dream – by (sometimes) doing a study, writing a book, consulting for/starting a company and then, ideally,- selling it all to a big pharma before the bubble bursts (resveratrol is a prime example). In this society there is apparently nothing wrong (or at least criminal) in it. From snake oil and cocaine and lithium laced drinks to every sort of vitamin and antioxidant, from low protein to low fat to low carb diets, from high (milk or fecal) colonics to probiotics – we had seen it all.
I am sure there are people who believe that this time – “OM3 time” – we are getting it right. Finally. Definitely.
Or may be not.
If history is to be our guide – I would say – most likely -“not”.
“Those who cannot remember the past are condemned to repeat it” George Santayana
I agree with Dmitri. A well-considered examination of the evidence (the fourth this year) suggests no benefit to omega-3 fatty acid supplementation. You cannot take a complex mixture of macromolecules as found in an oily fish species like salmon or tuna and distill it down to two micronutrients in supplement form. It is the fish-consuming lifestyle that is beneficial, not the omega-3.
I read the paper in full and it suggests considerably narrowing benefits in the contemporary era.
Dr. Blanchet,
Thanks a lot for the fruitful discussion. I agree with many of your points. But we all know that there are diverse opinions even about the clearest of trials –which is good for science –and I am sure we can find some of these pitfalls in the positive omega-3 trials, too (just as a single example, benefits in the GISSI-HF trial did not reach statistical significance in the “main” pre-specified unadjusted analysis, and reached significance only after some adjustments…). That being said, we see that a large proportion of studies –despite all their limitations –do not show a consistent benefit.
I do not argue that “omega-3 supplements are not good for any patient subgroup” but do think that we should be cautious and that we need more evidence before recommending supplements to a wide array of people (patients). As you know, there are some notable ongoing trials which will provide additional insight about the efficacy of omega-3 supplements.
Dr. Bikdeli,
As you quoted,
“When it is not in our power to follow what is true, we ought to follow what is most probable -Descartes”.
Looking at the DATA from Gissi and Jelis, it seems probable that higher doses of omega-3, especially in subjects on low dose or no statin is likely beneficial.
Assuming it is not beneficial, what is the likelihood of harm? It costs pennies a day and separate from the cardiovascular world, diets high in fish oil omega-3 are associated with a 40% reduction in Alzheimer’s Disease and age related macular degeneration. Diets high in unsaturated fats is also associated with a significant reduction in Parkinson’s disease.
No study on the use of fish oil derived omega-3s have shown net harm.
So if you are right and omega-3 has no value and a study of 11,000 subjects with a dramatic reduction in events (GISI Prevenzione) was just chance, people taking fish oil will be a little poorer but no less healthy. If I am right and fish oil is an important component in a program to prevent heart attacks, then people are helped a lot!
I fail to see the need to try to convince people to stay away from fish oil when the options for outcome are either dramatic improvement in health or at worst no harm to health. If more DATA is coming, lets use omega-3 until the DATA is here.
The safety profile of omega-3 supplements appears to be probably better than many other drugs/supplements. However, they may not be free from risk. For example, in the OPACH study (http://www.ncbi.nlm.nih.gov/pubmed/17699287), there were more cerebrovascular events in the omega-3 arm (12/103 vs. 5/103). Numerically higher cerebrovascular events were also observed in GISSI-HF, Omega, and GELIS. Strikingly, such data are not presented in the Alpha-Omega trial. We may need a formal meta-analysis to see if the pooled results of all trials confirm such a risk but ,in general, supplements may not be risk-free, as we have seen previously.
Also, I am unaware of clinical trial data about the benefits of such supplements in healthy adults. And in the subset of patients that there is some signal of benefit, we should be cognizant of issues such pill burden, that may affect the medication adherence in the real world.
All in all, my personal preference is for dietary sources of omega-3. Beyond that, you may consider prescribing the supplements on a case-by-case basis and based on shared decision-making, for patients who are compliant for the extra pill burden and accept the inconvenience in a hope for a possible (not definite) benefit.
GISSI-P also showed trend to excess of all and non-fatal strokes in OM3 group, especially early on (RR 3.23 at 3 months).
There is at least an intermittent signal of increase in hemorrhagic strokes in the trials that reported isch/hem strokes separately.
Safety of any pharmaceutical – even “naturally derived” – cannot be automatically assumed, and needs to be confirmed. There is no free lunch. Ever.
The trend toward increaed CVA is a distraction, not a fact. There were very few strokes in Gissi-P compared to the coronary events noted (and prevented). GSK (Lovaza) has studied the safety of high dose fish oil derived omega-3 FFA with no significant increase in ischemic or hemorrhagic strokes.
NEJM looked at the purity of the fish oil in the US and determied that fish oil is safer to consume than fish due to the higher mercury and agricultural toxins found in fish. I don’t avoid dietary omega-3 however I am not sure that recommending more mercury in the form of fish flesh is necessarily a great idea.
Dr. Blanchet:
the question is if one follows the paradigm of “shoot first – answer questions later” or “primo no nocere”. Put in a different words – would you rather not to miss a chance to deliver benefits – or avoid doing harm. And – no – we cannot have it both ways. There is no “balance”. I am still faithful to the oath I took – call me a “dinosaur” if you wish.
“Significant” is the key word here. Especially when it comes from the GSK (one of my former speaking/consulting employers – sorry). And -“there are no facts – only interpretations” (Nietzsche).
Yet – I have to admit – that for GISSI-P or GISSI-HF type of patients I unequivocally recommend 1 gram of OM3FA. The results are just too dramatic and potential downside is seemingly so small – as you noted – CV events by far outnumbered strokes.
Primary prevention – is a whole different story, however. The only evidence we have comes from Inuit and Mediterranean population observational studies and essentially a single half-decent interventional study which used Mediterranean diet with added margarine enriched with vegetable source OM3 (not fish!).
There is a complete-absolute- zero interventional outcome data on fish-derived OM3 for primary prevention. Never was, never will be. All there is -an overt or poorly concealed (and very skillful) marketing of unregulated supplements or a use of a prescriptional medication (Lovaza) in unapproved dose for unapproved indication(s).
Thus, with my patients -I stress pesco-vegetarian diet with emphasis on sustainably harvested (whatever this means in the US) cold water wild fish (no mercury) and Mediterranean “don’t worry – be happy” mental attitude and overall lifestyle. Achieving these in North American patient population is nearly impossible (the patient has to seize to be North American in lifestyle and set of mind) – but when it happens – the results are nothing but…well…Mediterranean…