May 1st, 2011
Don’t Miss the New AHA Recommendations on Triglycerides
Harlan M. Krumholz, MD, SM
I’ve been surprised at the lack of fanfare surrounding the American Heart Association’s recently published scientific statement on triglycerides and cardiovascular disease (CVD). The attention it did receive focused on the lower fasting triglyceride level that is now considered optimal: <100 mg/dL. In my opinion, the real headline was the committee’s important statements in support of less drug treatment — in particular, the recommendation for a substantial increase in the triglyceride level that should trigger consideration of pharmacologic therapy.
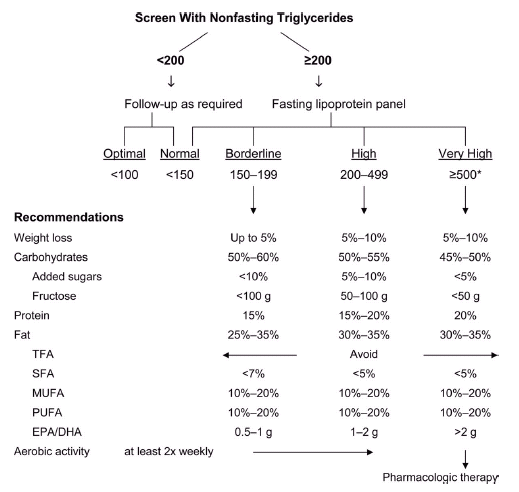
After a careful review of the recent literature, the committee concluded that pharmacologic therapy should not be started until a patient’s fasting triglyceride level is ≥500 mg/dL (in contrast to the Adult Treatment Panel’s recommendation of ≥200 mg/dL). See the figure below, which also appears on page 17 of the AHA statement.
The AHA committee also explicitly acknowledges (on page 6) that “the independence of triglyceride level as a causal factor in promoting CVD remains debatable. Rather, triglyceride levels appear to provide unique information as a biomarker of risk, especially when combined with low HDL-C and elevated LDL-C.” This clear statement—together with the new, higher threshold for initiating drug treatment—represents a remarkable change.
Meanwhile, on April 20, Abbott announced that sales of its flagship fenofibrate drugs increased by 28% in the first quarter.
Two questions:
- Why are doctors prescribing fibrates with growing enthusiasm when data from negative drug trials support an increasingly conservative approach to drug treatment?
- Given the new AHA recommendations, what should we do about all the people who were started on drug therapy to lower triglyceride levels that were less than 500 mg/dL?
I welcome your insights.

The FIELD trial had long back exposed the limitations of fenofibrate.It is not that triglyceride lowering is not important,it is a weakness of this particular drug despite theoretical benefits.Should we not be using niacin more often?How about omega 3 fatty acids?
Competing interests pertaining specifically to this post, comment, or both:
None.
elevated fasting TG’s, are also a surrogate marker for Insulin resistance, at the level of adipose tissue – so if we find elevated TG’s along with Obesity, IGTT or T1DM/ T2DM – then what i believe is, it is more important to treat the latter conditions rather than targeting TG’s with fibrates – at least for first 3 months into the treatment either with diet/exercise/ Insulin sensitizer’s, the TG’s could be reveiwed at followup and fibrates could be prescribed – if they are still above baseline.
Competing interests pertaining specifically to this post, comment, or both:
None
Understanding physician behavior is challenging. Hopefully our profession will increase its understanding of itself, but right now its sad to say that the drug companies may have a better understanding on the whole. A drug without major harm and with a visually gratifying result on a” bad” marker is hard to slow down. It will be even harder to withdraw.
Fibrates are not drugs to treat atherosclerosis however they are helpful in preventing the micro-vascular disease of diabetes. Fibrates are Type II diabetes drugs.
The issue is not that triglycerides should not be treated, the problem is that fibrates do not change macro-vascular endpoints. The treatment of triglycerides with Omega-3 fatty acids and niacin is important. Fibrates are needed when triglycerides are high enough to cause pancreatitis.
Competing interests pertaining specifically to this post, comment, or both:
I used to speak for Lovaza. I no longer do. I frequently use purified omega-3 fatty acids to treat atherosclerosis, elevated triglycerides, and heart failure with good success.
I used to speak for Abbott, I no longer do. I frequently use extended release nicotinic acid to treat atherosclerosis, elevated triglycerides, and low HDL cholesterol.
I have been looking for a case report or article showing the effect of fibrates on reducing the risk of pancreatitis – have you seen one. And with respect to microvascular complications in patients with diabetes – the evidence is not strong – particularly for outcomes that patients experience. In fact, I have not seen anything persuasive. The retinopathy study for ACCORD showed improvement in a surrogate endpoint composite score – but no effect on vision – and the relationship of that score to future vision problems is not well established – at least as far as I can see. Please share your information if you know something more.
It is really surprising why people are using too much of fibrates.There is no evidence regarding any significant benefit in the hard end points.
I think drug therapy should not be considered if the TGL is less than 500.
Competing interests pertaining specifically to this post, comment, or both:
none
elevated TG’s are surrogate marker of insulin resistence, therefore – the approach should be to treat assosciated obesity, IGTT , T1DM or T2DM – may be with diet, exercise, or insulin sensitizer’s rather than targeting TG’s alone. they can always be reviwed 2-3 months later – and fibrates could be an option. the AHA flowchart further simpifies the treatment protocol.
Competing interests pertaining specifically to this post, comment, or both:
none
The ACCORD Lipid Study (http://dx.doi.org/10.1056/NEJMoa1001282) showed worsening renal function and no cardiovascular benefit from fibrates when fibrates vs. placebo were added to statins in diabetics.
You cannot interpret the study to say fibrates were a clear winner for renal outcomes. To clarify, fibrates were associated with an increase in creatinine and a lower incidence of microalbuminuria (absolute difference about 3%) and macroalbuminuria (absolute difference about 2%). There was no difference in renal outcomes that patients actually experience.
Do we need any more evidence that Pharma is about money and not patients?
Competing interests pertaining specifically to this post, comment, or both:
None
No reason to disparage industry. Most people believe that lowering risk factors lower risk. We need to recognize that it is not that simple – and practice accordingly.
I have recently seen a woman in her 50’s with obvious metabolic syndrome and carotid artery disease that necessitated stenting last year. She had minimal cardiac issues, and no known coronary disease. Her fasting lipid profile was acceptable except her fasting triglycerides that were approaching 300 mg/dl. I opted to counsel her for diet and exercise as she was clearly obese and sedentary. I am curious to see if anyone would argue to initiate pharmacological therapy in this patient? She is currently on combnation of simvastatin and ezetimibe…There is evidence of atherosclerosis but no prior vascular events.
Competing interests pertaining specifically to this post, comment, or both:
None
Given the adverse effects of ezetimibe on even surrogate CVD outcomes (i.e. carotid IMT in the ARBITER 6–HALTS and ENHANCE), I would recommend against its use in this setting. Niacin or OM3FA are more appropriate as adjunctive agents in patients already on statin therapy.
Competing interests pertaining specifically to this post, comment, or both:
None
This is a tough situation because we so want to help her and respond to her numbers. It is just that we have little evidence that adding to her medical regimen will reduce her risk – though we can make her numbers look better. I like your approach with diet and exercise – you are consistent with the new AHA recommendations, which do not recommend drugs until the TG level is more than 500 (see the original post). And why is she on ezetimibe? I agree with Dr. Harrell.