May 18th, 2011
New Technique Cuts Radiation Dose of MPI SPECT by Half
Larry Husten, PHD
A new study raises the possibility that the radiation dose for MPI SPECT imaging can be reduced by half without sacrificing image quality, according to Dr. Nili Zafrir, who presented the results of the study this week at the International Conference of Non-Invasive Cardiovascular Imaging in Amsterdam.
Recently, software has become available that can reduce the image acquisition time of MPI SPECT. Zafrir and her colleagues in Israel sought to test the hypothesis that the same software could be used to reduce the radiation dose of Tc sestamibi by half. Some 218 patients were randomized to either a “half-dose” protocol using the “half time” software or a “full-dose” protocol using standard software techniques.
The investigators reported that 95% of images in both the half-dose group and the full-dose group were rated excellent to good. The effective dose was 7.2 mSv in the half-dose group compared with 13 mSv in the full-dose group, a highly significant difference (p<0.0001). They further reported that slightly more than a third of patients in the half-dose group had a “stress only” study and received a very low radiation dose of only 2 mSv.
“Clearly, we cannot be certain what the long-term benefit of reducing radiation exposure might be, but theoretically it would seem important,” said Dr. Zafrir, in an ESC press release.
May 18th, 2011
The Curse of the Mummy: Coronary Artery Disease?
Larry Husten, PHD
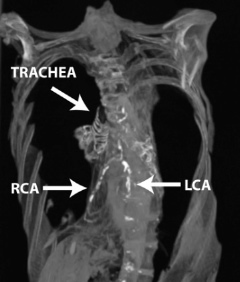
Could the real curse of the mummy be coronary artery disease? Despite strict adherence to the original Mediterranean diet and a complete lack of tobacco, trans fats, and refined sugars, an Egyptian princess who died around 1550 BC is the first person in history to receive a diagnosis of coronary artery disease.
A CT scan of the princess was presented yesterday at the International Conference of Non-Invasive Cardiovascular Imaging in Amsterdam. The princess, who had blockages in her left and right coronary arteries, was one of 52 Egyptian mummies included in the study. Twenty of the mummies had definite signs of atherosclerosis, but only 3 had evidence of coronary narrowing.
“Overall, it was striking how much atherosclerosis we found,” said Dr. Gregory Thomas, a co-principal investigator of the study, in an ESC press release. “We think of atherosclerosis as a disease of modern lifestyle, but it’s clear that it also existed 3500 years ago. Our findings certainly call into question the perception of atherosclerosis as a modern disease.”
(Photographs reprinted courtesy of Michael Miyamoto, MD)
May 17th, 2011
FDA Reviewers Scrutinize ACCORD and Trilipix
Larry Husten, PHD
The FDA has released the agenda, questions, roster, and briefing materials for Thursday’s meeting of the Endocrinologic and Metabolic Drugs Advisory Committee in which the ACCORD trial and the fate of Abbott’s Trilipix (fenofibric acid) will be discussed.
The key questions on which the advisory committee members will be asked to vote are:
- Should the FDA require a new clinical trial to demonstrate the benefit of Trilipix in high-risk patients?
- Regarding Trlipix’s indication for coadminstration with a statin: Should the current indication be maintained, withdrawn, or revised to incorporate the findings from ACCORD?
The FDA reviewers were critical of the data in support of fibrate therapy. Here is the conclusion of the main review of ACCORD:
Fibrates have been investigated in at least five major clinical trials and have produced mixed results. Although outcome trials with gemfibrozil have shown cardiovascular benefit over placebo, fenofibrate has not. The answer to the question of why fenofibrate produced unimpressive cardiovascular outcome results relative to gemfibrozil is not known. The inconsistent findings may be a result of pharmacodynamic differences between individual fibrates and diverse study populations or both.
One way to obtain a more definitive answer to the question of fenofibrate’s cardiovascular benefit when added to a statin is to conduct a clinical trial specifically designed to test the hypothesis that, in high-risk men and women at LDL-C goal on a statin with residually high TG and low HDL-C, treatment with fenofibrate versus placebo significantly reduces the risk for major adverse cardiovascular events (MACE). Such a trial would also provide additional information regarding the cardiovascular effects of fenofibrate plus statin versus statin monotherapy in women versus men.
The FDA also said that postmarketing observational safety studies had found a moderate to large relative increase in rhabdomyolysis with statins plus fibrates compared with statin monotherapy, but that the absolute increase was still small.
May 16th, 2011
Sleep Deprivation Not as Bad as We Think for Cardiac Surgeons
Larry Husten, PHD
Sleep deprivation in cardiac surgeons does not lead to worse surgical outcomes, according to a study published in the Archives of Surgery. Michael Chu and colleagues collected sleep information from six consultant surgeons working at a large hospital in Ontario, Canada and outcome data from their 4,047 patients who underwent cardiac surgery from 2004 through 2009.
Of the 4,407 procedures:
- 83 were performed by a surgeon with 0 to 3 hours of sleep
- 1595 with 3 to 6 hours
- 2369 with more than 6 hours
Mortality and major complications did not differ significantly across the groups:
- Mortality: 3.6% in the 0-3 hour group, 2.8% in the 3-6 hour group, and 3.4% in the 6+ hour group (p=0.53)
Observed versus expected ratio of major complications:
- 1.20 in the 0-3 hour group, 0.95 in the 3-6 hour group, and 1.07 in the 6+ hour group (p=0.25)
The researchers also found that the age of the surgeons did not significantly affect outcomes.
The authors write that their findings “may have important ramifications in restricting current trainee work hours when future practice may demand optimal performance during sleep-deprived conditions.” Although the ACGME has imposed limitations on work hours for medical trainees, the authors point to studies, including their own, that undermine “the intuitive belief that reduced work hours improves daytime fatigue, trainee performance, and, hence, patient safety…. the findings of our study might suggest reassessment of this belief when contemplating trainee work-hour limitations.”
In an invited critique, David Yuh writes that the “reassuring” results of the study “may not be reflected in future generations of cardiac surgeons” because under new regulations, surgical trainees may not “enjoy the purported benefits of comparatively long hours, including physiologic and mental conditioning and following the course of an acute disease process from beginning to end.” He asks:
“Will patient safety be paradoxically compromised by young practicing cardiac surgeons who can more easily convince themselves that delaying the coronary revascularization of an ischemic patient or repair of an acute ascending aortic dissection for a few hours of extra sleep will actually improve their technical or cognitive performance and therefore serve the best interests of the patient?”
May 13th, 2011
ProPublica Takes Aim at SCAI
Larry Husten, PHD
Now it’s SCAI’s turn. Following its investigation of the Heart Rhythm Society’s ties to industry last week, ProPublica has now focused its attention on the Society for Cardiac Angiography and Interventions (SCAI). In the latest installment of ProPublica’s Dollars for Doctors series, Charles Ornstein writes that SCAI “received 57 percent of its revenues in 2009 from medical device and pharmaceutical makers, according to financial information on the group’s website.” SCAI’s biggest funders are the large stent makers, he reports.
“I don’t think industry is driving the delivery of health care,” Larry Dean, the immediate past-president of SCAI told ProPublica. “The companies that make stents don’t drive it either.”
May 13th, 2011
Simultaneous TIA and ACS After Aspirin Cessation for Palpebral Surgery
Jean-Pierre Usdin, MD and James Fang, MD
A 77-year-old man with metformin-treated type 2 diabetes, high blood pressure, moderate renal insufficiency, stable angina, and a history of phlebitis stopped taking aspirin in preparation for palpebral surgery. A day after the surgery, he presented to the ER with two transient ischemic attacks (TIAs) affecting the left arm.
The patient complained to the examining neurologist of epigastric discomfort. An electrocardiogram showed new abnormalities, and the man was diagnosed with ST-segment elevation acute coronary syndrome (ACS). A head CT was negative for acute thrombosis or bleed. Given the man’s recent surgery, coronary angiography was postponed for 48 hours. Aspirin was given along with other usual medical therapy.
Two days later, a few minutes before the scheduled angiogram, the patient developed a serious nosebleed and the angiogram was canceled. After another two days, the angiogram was finally performed, 300-mg clopidogrel was given, and a drug-eluting stent was placed in the left-anterior descending artery using a right femoral artery approach. A few minutes after the patient left the cath lab, the nosebleed recurred. No transfusion was necessary.
The day after the angiogram, an asymptomatic left femoral vein thrombus was detected on systematic vein Doppler imaging. This 88-kg man with a serum creatinine level of 2.5 mg/dL was discharged 3 days later on fondaparinux (5 mg/day), aspirin, and clopidogrel.
Another 10 days later, while at his country house, the patient experienced another nosebleed and was driven to the closest hospital. The attending physician decided to stop fondaparinux and start warfarin; aspirin and clopidogrel were continued. Phlebitis, again confirmed, was healing well.
Questions:
1. Was the initial delay in performing the angiogram warranted?
2. Was it appropriate to implant a drug-eluting stent?
3. Was the choice of fondaparinux a good one, would low-molecular-weight heparin have been a better choice, or would warfarin have been preferable from the start?
Response:
James Fang, MD
This complicated case represents what clinicians are increasingly encountering in practice: a patient with concomitant bleeding and thrombosis. The general approach is to consider the most life-threatening issue first and to recognize that other medical treatments for acute ischemic heart disease (short of mechanical revascularization) are often underutilized. Unfortunately, the relevance of evidence-based strategies to these situations is often limited because most clinical studies exclude such patients.
A TIA followed by a STEMI should raise concerns about brain–heart syndromes, such as embolic conditions (endocarditis, atrial fibrillation, heart failure, myxomas) and aortic syndromes (dissection, aortic plaque, vasculitis). Pre-intervention imaging is crucial in such cases because specific brain–heart diagnoses are difficult to make purely on the basis of clinical acumen.
In this particular case, an initial delay in performing coronary angiography would seem appropriate until the neurologic issues were comfortably resolved. However, the narrative does not make clear why resolution took 48 hours. Was the STEMI aborted with medical therapy? A small but significant proportion of infarcts can be aborted with aggressive medical management short of mechanical reperfusion. Although this was presumably an anterior MI, was it a “high-risk” situation? Clinical tools (e.g., the STEMI TIMI risk score) can be used to help determine the level of risk. Coronary angiography and PCI can be performed in a patient, even with a serious nosebleed (particularly if the STEMI is a high-risk one). It is not clear how the nosebleed was investigated or addressed, but being unable to control this type of bleeding is unusual.
Given the presence of both bleeding and thrombosis (and the possible need for subsequent warfarin anticoagulation), a bare-metal stent might have been a reasonable choice to avoid the need for prolonged dual antiplatelet therapy. If the vessel was quite large and the diseased segment relatively short, the risk for restenosis with a bare-metal stent might have been acceptable despite the patient’s diabetes.
With a new thrombosis, systemic anticoagulation needs to be strongly considered. However, this man has several risk factors for bleeding (older age, acute coronary syndrome, diabetes, renal insufficiency, dual antiplatelet therapy), and the use of “triple therapy” will undoubtedly be complicated by bleeding. Although some concern about hypercoagulability may be warranted without bridging antithrombin therapy to warfarin, one can make a case for initiating warfarin without the bridge. Use of a retrievable inferior vena cava filter as adjuvant therapy could even be considered.
This case was submitted by a member of the CardioExchange online community. If you have an interesting case for the community to discuss, submit it to our physician-editors.
May 12th, 2011
TAVI & Stroke: More Details Surface About PARTNER A
Larry Husten, PHD
In the past year transcatheter aortic valve implantation (TAVI) has emerged as a possible new treatment for patients with aortic valve disease who are not surgical candidates (the PARTNER B study) and for some patients as a viable alternative to surgery (the PARTNER A study). TAVI was found to be noninferior to surgery in the PARTNER A trial, however, a major question lingers over the higher rate of stroke in the TAVI arm. In a presentation (PowerPoint slide set) earlier this week at the annual meeting of the American Association for Thoracic Surgery, Craig Miller presented results of the PARTNER A stroke substudy.
Overall, said Miller, the 30-day rate of stroke and TIA was low in both groups, considering the very high baseline risk of the patients:
- Surgery=2.6% versus TAVI=5.6% (p=0.05)
PARTNER patients in whom the transfemoral (TF) approach was possible had an even lower risk of stroke and TIA:
- TF group: Surgery=1.4% versus TAVI=4.6% (p=0.04)
Major stroke at 30 days:
- Surgery=2.3% versus TAVI=3.8% (p=0.25)
- TF group: Surgery=1.4% versus TAVI=2.5% (p=0.37)
Miller reported that in the early phase the risk of stroke was elevated in the TAVI group, particularly in patients with a smaller AVA index. In the subsequent period, patients with a “generalized heavy arteriosclerotic burden” who were not candidates for the TF approach had a higher risk of stroke or TIA.
“The higher observed incidence of neurological events in the ‘non-TF candidate’ stratum reflected the patient substrate, and was not related to the transapical TAVR or AVR procedures per se,” he concluded.
Stroke and TIA had a different effect on subsequent mortality depending on treatment group. In the surgery group, a neurological event was associated with an early high peak in mortality which quickly returned to baseline. In the TAVI group, the increase in mortality risk remained elevated during the 2-year follow-up period, especially in patients in the transapical group.
May 11th, 2011
Optimal Medical Therapy and the Lack of COURAGE
William Borden, MD and John Spertus, MD, MPH
We welcome William Borden and John Spertus to answer questions from CardioExchange Editor-in-Chief Harlan Krumholz about their JAMA paper showing that optimal medical therapy (OMT) for patients with coronary artery disease (CAD) did not receive a meaningful boost from the publication of the COURAGE trial, despite the trial’s clear message showing the benefits of OMT.
Using data on 467,211 patients in the National Cardiovascular Data Registry to analyze the use of OMT in CAD patients prior to PCI and at the time of discharge, both before and after COURAGE was published, they found:
- Before PCI: OMT was used in 43.5% of patients before COURAGE and 44.7% after COURAGE.
- At discharge after PCI: OMT was used in 63.5% of patients before and 66.0% after COURAGE.
“Collectively, these findings suggest a significant opportunity for improvement and a limited effect of an expensive, highly publicized clinical trial on routine clinical practice,” the authors wrote.
Krumholz: Could the low rate of OMT be a result of patient preference?
Borden and Spertus: In our study, the low rate of OMT is not due to patient preference, since our database documents only those medications prescribed by the physician, not whether or not the patients were actually taking the medicines. Also, if a physician did not prescribe a medication because of patient preference, then that preference could be documented as a contraindication, which would not lower the OMT rate.
Krumholz: Are you sure about the quality of the medication data in the CathPCI registry?
Borden and Spertus: The medication data in the CathPCI registry are reported by the individual institutions according to rigorous data definitions and training. We cannot confidently exclude the possibility that these are not accurately abstracted, although registering patients’ medications on admission is a standard of care and should render these data easy to identify and record. Moreover, there is no reason to think that the quality of the medication data would have changed from the pre-COURAGE to the post-COURAGE period, and finding no meaningful increase in the use of OMT after COURAGE suggests that among the patients undergoing PCI, clinicians are not being substantially more aggressive in attempting OMT to see whether PCI could be avoided.
Krumholz: What do you recommend for someone with a high-risk study who does not want to try medications?
Borden and Spertus: Ultimately we believe that patients are autonomous and can request procedures that are medically reasonable. Based on the 2009 ACC/AHA Appropriateness Criteria for Coronary Revascularization, someone with a high-risk stress test on no medications would be considered appropriate for revascularization. However, we would want to be sure that the patient clearly understood that the procedure is not likely to make him or her live longer or prevent a heart attack. Furthermore, the patient would still be encouraged to take aspirin, thienopyridines, statins, and beta-blockers. The PCI does not obviate the benefit of these medications. The primary benefit of revascularization would be the alleviation of symptoms, which might also be accomplished with aggressive OMT alone.
Krumholz: Why do you think this is inadequate translation of COURAGE? Couldn’t this be a conscious decision by patients and their doctors after taking into account COURAGE?
Borden and Spertus: Our study does not preclude the possibility that some practitioners are following the COURAGE insights with attempting OMT in their stable angina patients and not referring them to PCI, as we only studied those patients who underwent PCI. In fact, a recent publication by Ahmed and colleagues noted a decrease in the proportion of PCI patients with stable angina in Northern New England. However, among those referred to PCI, we did not appreciate substantial increases in the use of OMT prior to treatment. While I doubt that this is a conscious decision of patients, there are a number of potential explanations, including possible clinicians’ disbelief of the COURAGE results, economic incentives to preferentially treat with revascularization, referral patterns, and concerns of interventionalists that if they don’t perform the PCI for a referring doctor that the doctor will not refer future patients. More work is clearly needed to illuminate the opportunities to further improve the use of OMT prior to, and after, PCI.
Krumholz: How would you improve current care?
Borden and Spertus: One key step to improving care may be through better collaboration among caregivers. Primary and interventional cardiologists could work together to ensure that patients, both before and after PCI, are on appropriate medical therapies. Supporting such collaboration and emphasizing medical management should be a priority of ongoing efforts toward improving our healthcare system.
May 10th, 2011
Trial REVEALs No Benefit and Some Concerns with Erythropoietin After Primary PCI
Larry Husten, PHD
Erythropoietin alfa failed to reduce infarct size and was associated with more cardiovascular events when given after successful PCI in STEMI patients, according to results from the REVEAL (Reduction of Infarct Expansion and Ventricular Remodeling With Erythropoietin After Large Myocardial Infarction) trial published in JAMA.
In the trial, which included a dose-escalation safety phase and a single-dose efficacy phase, 222 patients at 28 sites in the U.S. were randomized to epoetin alfa or placebo following successful reperfusion. Overall, there was no difference between the groups in infarct size as assessed by MRI. However, among patients 70 years of age or older (a prespecified subgroup), infarct size in the first week was significantly greater with treatment than with placebo: 19.9% versus 11.7% LV mass (p=0.03).
During the safety phase of the study, the composite endpoint of death, MI, stroke, or stent thrombosis occurred in 5 of the 125 patients in the treatment group compared with none of the 97 patients in the placebo group (p=0.04).
In an accompanying editorial, Deepak Bhatt writes that the results “raise further questions about the safety of epoetin alfa in the context of acute MI.” He continues:
“The totality of evidence strongly suggests that this class of medication has cardiovascular risk, most likely to manifest in higher-risk individuals. Until compelling data become available to support routine use of these agents in patients with anemia, it would be prudent to minimize their use, especially for patients at high risk for cardiovascular disease or with an acute ischemic syndrome.”
May 10th, 2011
Short-Term NSAID Use Linked to Increased CV Risk
Larry Husten, PHD
Short-term use of NSAIDs, including diclofenac, is associated with increased cardiovascular risk, according to a very large study published online in Circulation.
Danish researchers used a national registry to study more than 83,000 patients who were admitted to the hospital for a first MI from 1997 to 2006. Some 42% of the patients received NSAIDs during the follow-up period, during which there were 35,257 recurrent MIs or death. The NSAID-associated risk started early in treatment and persisted over the treatment course:
- First week: HR 1.45; CI 1.29-1.62
- After 90 days: HR 1.55; CI 1.46-1.64
A significant increase in risk was observed with all the NSAIDs. The risk was slightly lower with naproxen, while diclofenac was associated with the highest risk (HR 3.26; CI 2.57-3.86 for death/MI in the first week).
The authors write: “Particularly worrying was the fact that the widely used nonselective NSAID diclofenac was associated with early and higher cardiovascular risk than the selective cyclooxygenase-2 inhibitor rofecoxib, which was withdrawn from the market in 2004 owing to its unfavorable cardiovascular risk profile. Our results indicate that there is no apparent safe therapeutic window for NSAIDs in patients with prior myocardial infarction and challenge the current recommendations of short-term use of NSAIDs as being safe. We believe this message is important, and should be distributed as widely as possible to clinicians taking care of patients with cardiovascular disease.”